- Volume 61 , Number 1
- Page: 1–7
Problems of leprosy relapse in China
ABSTRACT
The proportion of relapses among all patients detected each year increased steadily since the initiation of the national leprosy control program in China with dapsone monotherapy in 1955, reaching 18%-24% in the more leprosy-endemic provinces along the coast. Relapses were also reported in the formerly rifampin-plus-dapsone-treated patients. So far, only three paucibacillary relapses after 6 months of multidrug therapy (MDT) have been reported, and these were due to misclassification at the time of diagnosis.A short course of MDT should be given to all formerly dapsone- and/or rifampinplus-dapsone-cured patients for the prevention of relapse. If not, they should be screened every 1 to 2 years for any possible signs of relapse, and MDT given when needed.
RÉSUMÉ
La proportion de rechutes parmi l'ensemble des patients détectés chaque année a augmenté régulièrement depuis la mise en route en 1955 du programme national de lutte contre la lèpre en Chine, basé sur la dapsone en monothérapic, pour atteindre 18 à 24% dans les provinces côtières à endémie lépreuse plus élevée. Des rechutes ont également été rapportées parmi les patients traites antérieurement par la combinaison rifampicinc + dapsone. Jusqu'à présent, seulement trois rechutes paucibacillaircs après une polychimiothérapie (PCT) de six mois ont été rapportées, et celles-ci étaient DUCS à une mauvaise classification au moment du diagnostic.Un traitement court de PCT devrait être donné à tous les patients guéris traités antérieurement par dapsone et/ou rifampicinc + dapsone, pour la prévention des rechutes. Dans le cas contraire, ils devraient être examinés tous les un à deux ans pour détecter les signes de rechute, et mis sous PCT quand nécessaire.
RESUMEN
La incidencia de recaídas entre todos los pacientes detectados cada año en China ha aumentado sostenidamente desde el inicio en 1955, del programa de control de la lepra con dapsona, alcanzando niveles del 18% al 24% en las provincias de mayor endemia distribuidas a lo largo de la costa. También se reportaron recaídas en los pacientes anteriormente tratados con rifampina más dapsona. Hasta ahora, sólo se han reportado 3 recaídas paucibacilares después de 6 meses de tratamiento con poliquimioterapia (PQT) pero estos casos, en realidad se clasificaron erróneamente como paucibacilares en el momento del diagnóstico.Todos los pacientes curados, inicialmente tratados con dapsona y/o rifampina más dapsona, deberían recibir un corto tratamiento con PQT para prevenir las recaídas. Si no, los pacientes deberían ser examinados cada 1-2 años para detectar cualquier signo de recaída, y recibir la PQT en el momento que fuera necesario.
Leprosy control with intensive case finding and dapsone monotherapy in leprosaria was introduced in China in 1955. All patients reaching clinical cure (clinical, bacterial index, and histopathology negative) with dapsone monotherapy were kept on maintenance therapy with dapsone 100 mg daily [multibacillary (MB) for 5-10 years, paucibacillary (PB) for 2-5 years] and then dapsone was discontinued. Between 1979-1984 rifampin was widely used in addition to dapsone. By the end of 1981, when the national policy of leprosy control with domiciliary multidrug therapy (MDT) was adopted, the number of registered patients had fallen from 500,000 to 200,000. If at the time of initiation of MDT some patients were still on dapsone maintenance therapy, they were required to receive a course of MDT (MB for 24 months, PB for 6 months).
In 1990, the number of registered patients was further reduced to 23,000 by MDT (prevalence rate 0.2/10,000), and the number of dapsone-cured patients amounted to 360,000 who now give rise to about 500 relapses among the 4000 patients detected annually (detection rate 0.34/100,000). The experience of relapse of previously cured leprosy patients in China may throw some light on the surveillance of leprosy after MDT, and the results of the prevention of relapses with a short course of MDT may be of interest to countries with similar relapse problems.
MATERIALS AND METHODS
Most data used in this paper are from published materials appearing in China and some are from papers presented at national leprosy meetings. The cumulative relapse rate in different provinces after dapsone monotherapy until clinical cure (clinical, smear and histopathology negative) are reported to be 2%-6%. No definite figure is available from the estimated more than 6000 patients who had received rifampin at 600 mg/day or once or twice a month in addition to dapsone before MDT.
RESULTS
Relapse after dapsone monotherapy
With the progress of organized leprosy control since 1955 and the gradual decrease in the number of patients, the proportion of relapses among the number of patients detected in the three more leprosy-endemic coastal provinces between 1955-1989 increased steadily, reaching 14% in Fujian and 18% in Guangdong (5 and Shao, K. W. Relapse in leprosy and leprosy control. Paper presented at the IV National Leprosy Conference, Nanchang, 13-18 October 1990). Shandong surveyed all formerly cured patients in 1986 and 1989, which resulted in a sharp increase to 24.6% in the proportion of relapses among all patients detected during 1985-1989 (unpublished data) (Fig. 1).
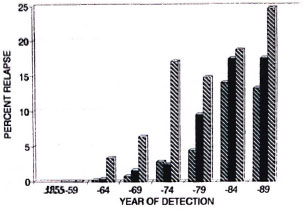
Fig. 1. Relapse in leprosy after clinical cure as a proportion of all patients detected in Fujian, Guangdong, and Shangdong Provinces, China, 1944-1989.  = Fugian;
= Fugian;  = Guangdong;
= Guangdong;  = Shandong.
= Shandong.
The relapses as a proportion of all cases detected by type in Sichuan between 1984- 1988 show a consistently higher proportion in multibacillary (MB) than in paucibacillary (PB) patients. The very high percentage of relapse in 1984 is due to the backlog of undetected relapses in previously dapsonccured patients because organized case finding was initiated in Sichuan in 1984 (Fig. 2) (6).
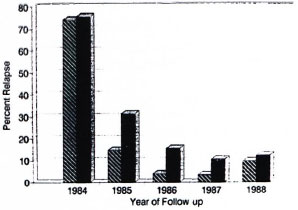
Fig. 2. Relapse in leprosy after clinical cure as a proportion of all patients detected in Sichuan Province, China, 1984-1988.  = Paucibacillary;
= Paucibacillary;  = multibacillary.
= multibacillary.
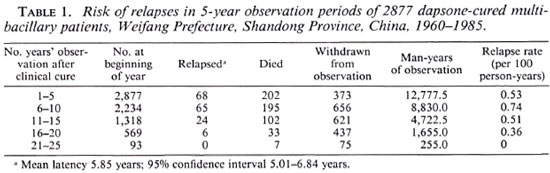
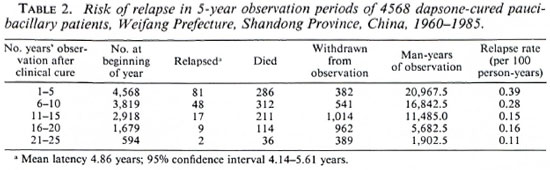
In Weifang Prefecture, Shandong Province, the average relapse rate was based upon person-years of follow up during 5-year blocks of time after cure, eliminating lost cases, deaths, and emigrations each year. The risk of relapse is consistently higher among MB cases, reaching 0.74 relapses per 100 person-years at 6-10 years of follow up (Table 1). In cured PB cases the risk of relapse is highest during the first 5 years after clinical cure, 0.39 per 100 person-years (Table 2) (7).
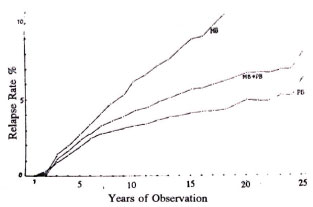
Fig. 3. Cumulative relapse rate in 2677 multibacillary (MB) and 4568 paucibacillary (PB) patients after clinical cure with dapsonc, Weifang Prefecture, Shandong Province, China, 1955-1985.
In the 11 relapses reported in 1992 in Leipo County, Liangshan Prefecture, Sichuan Province, the average bacterial index (BI) was 2.2 (range 0.5-3.6) at the time of diagnosis of relapse. These relapsed patients had an average dapsone monotherapy of more than 12 years (6-23 years) with an average period of 7.8 years (4-10 years) between clinical cure and diagnosis of relapse (unpublished data).
Relapse after rifampin-plus-dapsone therapy
Eight relapses were reported from 1646 patients (MB 887, PB 759) who received dapsone-plus-rifampin in Wenshan Prefecture, Yunnan Province, between 1976- 1985. These relapses had had dapsone 50- 100 mg/day for an average of 12.6 (5-20) years and, additionally, rifampin 600 mg/ month plus dapsone 100 mg/day for an average of 2.5 (2-5) years. The mean BI was 2.04 (0.2-4.0) and the mean period between clinical cure and diagnosis of relapse was 8.5 (2-20) years (unpublished data).
Prevention of relapse with MDT
Shanghai. With the aim to overcome the increasing relapse situation, in 1984 Shanghai treated all formerly dapsone-cured MB patients with the following modified MDT regimen:
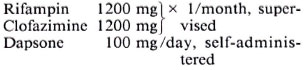
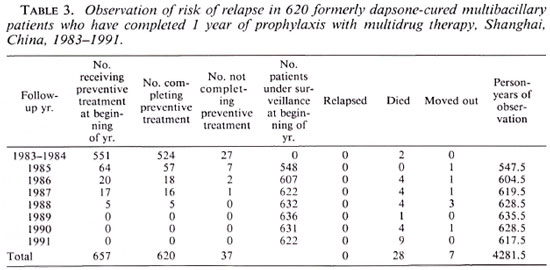
This regimen was for 12 months, and was to be completed in 15 months. Altogether 620 of 657 MB patients have completed the above regimen and 534 of them have been followed for 7 years. No relapse has yet been detected (Table 3). Of 137 formerly dapsone-cured MB patients in Shanghai who did not receive prophylactic treatment during this period (due to age and abnormal laboratory findings), 17 have relapsed (12.4% or 1.55% per year). If this rate is applied to the 620 MB patients, if they had not received MDT for the prevention of relapse, 77 relapses would have occurred. It is thus recommended that if the relapse rate among dapsone-cured patients in an area exceeds 1% per year, prophylaxis with MDT against relapse should be considered (Zhou, D. H. and Chen, J. K. Surveillance on 657 dapsone-cured patients after retrcatment with MDT. Paper presented at the IV National Leprosy Conference, Nanchang, 13- 19 October 1990).
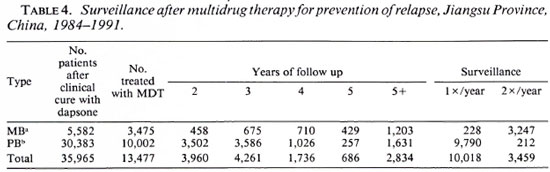
Jiangsu Province. Similarly, Jiangsu Province has also applied prophylactic therapy since 1984 on 3475 MB and 10,002 PB patients with the following regimens:
a) MB regimen for 6-12 months to be completed within 7-14 months:
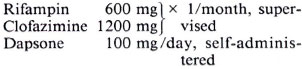
b) PB regimen for 6 months to be completed in 7 months:
Rifampin 600 mg x 1/month, supervised Dapsone 100 mg/day, self-administered.
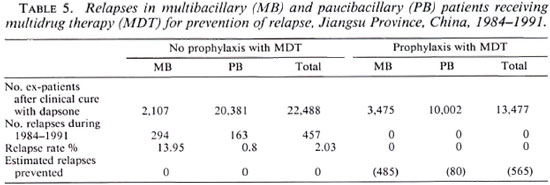
Regularity was high (MB 99.7%, PB 97.9%). There were relapses during the 5 years of follow up after prophylaxis with MDT (Table 4). During this period among the 22, 488 patients (2107 MB, 20,381 PB) who did not receive prophylactic treatment there were 457 relapses (MB 294, 14.0%; PB 163, 0.8%). If these rates were applied to the patients who received prophylaxis with MDT, 565 relapses (MB 485, PB 80) were prevented (Table 5) (Xie, Z. J. Prophylaxis of relapse with MDT in 13, 477 dapsone-cured leprosy patients. Paper presented at the IV National Leprosy Conference, Nanchang, 13-19 October 1990).
Relapses after fixed duration MDT
Since 1986, fixed duration MDT (MB 24 months, PB 6 months) was applied to seven prefectures in the three southwest provinces of China, covering about 18 million population in 59 counties with over 7000 leprosy patients (prevalence 0.21-3.25/1000/county), of whom 72% were MB. Between 1986- 1990, with the support of WHO, 6481 patients (MB 4125, PB 2356) completed MDT, only three PB relapses were reported. One relapse occurred in Wenshan Prefecture among 212 PB patients during the fourth year of surveillance (629 person-years). Kunming Prefecture reported two PB relapses among the 82 PB patients completing MDT. All three PB relapses had initially > 2-3 nerve involvement and two patients had 5-14 skin lesions. The 80 MB patients treated with 24-27 months of MDT in 1983 (4) are in their seventh year of surveillance (293 person-years). No relapses have been detected.
In another group of MB patients in Liangshan and Panzhihua Prefectures, Sichuan Province, 394 were released from treatment after 24 months of MDT. No relapses have been noted during the 1-5 years of observation (538 person-years). After termination of 24 months of MDT, the lesions continued to improve clinically and histopathologically, and the BI declined steadily. The smear-negative rate reached 95.3% in the MB patients of Menla County (41 of 43 patients) and 100% in the MB patients of Weifang Prefecture (33 of 33 patients) at the sixth year of follow up after termination of MDT (unpublished data).
It may be concluded that fixed duration MDT has a very good therapeutic effect both in MB (24 months) and PB (6 months) patients. For PB patients, careful examination of the extent and nature of skin lesions and nerve involvement is necessary to avoid misclassification and undertreatmcnt. It is well known that patients may be classified as PB but a nerve biopsy may show BL-LL histopathology (5).
DISCUSSION
Generally, compliance was good, since MB patients were treated as inpatients before the nationwide implementation of MDT in 1987, and the regularity of MDT usually exceeds 90%. The relapse rate in patients cured during the pre-MDT era is influenced by the following factors:
1. Most relapse studies were retrospective, through the examination of clinical records, which may have missing data.
2. Before 1970 the Madrid classification was used, which tends to inflate the number of MB patients.
3. Generally, the relapse rate is not differentiated into MB and PB patients. Since MB has a higher relapse rate, the rates will be high in the southwest provinces where the MB/PB ratio is high and lower in the provinces along the coast where the MB/PB ratio is lower.
4. Reactions after clinical cure are usually regarded as disease activity, hence often counted in error as relapses.
5. After attainment of clinical cure, maintenance therapy of dapsone 50-100 mg/ day was usually given to MB patients for 5-10 years and PB patients for 2-5 years. Regular maintenance of dapsone monotherapy tends to delay relapse.
6. Since many MB relapses are late, the relapse rate will be high if the follow-up period extends to 10-20 years or more (Fig. 4).
7. Before 1970, dapsone was given 50 mg/ day six times a week initially and increased to 150-200 mg/day after 3 months. Dapsone treatment was interrupted during reactions, and after the reactional episode the dapsone was restarted at the initial dose. This may have encouraged the development of dapsone resistance.
8. Since 1979, rifampin 600 mg/day or once or twice a month was widely implemented in addition to dapsone, and a large number of patients were thus cured. By rough estimate this number exceeded 6000 by the end of 1984. No effort has been made as yet to assess rifampin resistance or double resistance in these patients by the mouse foot pad method.
9. The diagnosis of relapse is usually based upon the judgment of the leprosy field worker, supported by smear and histopathological examinations, sometimes checked by the specialist from the Provincial Institute of Dermatology.
Relapse due to resistant bacilli tends to occur within a few years after cessation of chemotherapy. As yet no relapses have been noted among MB patients receiving 24-27 months of MDT with more than 7 years of follow up. We should nevertheless be aware of late relapses due to persisters after fixed duration MDT. In a well-controlled area a surveillance period of 10 years or more may be necessary to serve as a sentinel to monitor problems that may arise after the implementation of MDT. In the meantime there is need for good compliance with MDT for a minimum period of 24 months for MB and 6 months for PB, and when doubts arise in classification, the MB regimen should be administered.
Due to the high relapse rate of formerly dapsone- and/or rifampin-plus-dapsonecurcd patients, it is not enough just to screen them for clinical activity before the implementation of leprosy control with MDT. It is advisable to check them regularly for signs of relapse or, if circumstances permit, to treat all formerly cured patients with a short course of MDT.
A WHO evaluation team noted the high relapse rate among patients cured before the nationwide implementation of MDT, during a 1991 evaluation of the national leprosy program in eight provinces, and recommended (Abella, J., et al. Mission report on the evaluation of MDT implementation in Leprosy Control Program, China. WHO ICP/LEP/001 RS/91/0534) that:
1. Clinical examination of formerly dapsone- and/or rifampin-plus-dapsonecured patients at least once a year followed by smear examination if any suspicious lesion occurs.
2. Mouse foot pad sensitivity tests on relapses that have formerly received dapsone plus rifampin should be set up before retreating patients with MDT.
3. Training of leprosy workers and staff on the early recognition of lesions; relapses should be emphasized with active participation in case detection and surveillance in the leprosy control program.
Acknowledgment. The author is grateful to Dr. R. R. Jacobson for his encouragement and comments. She wishes also to express the deepest appreciation to the many leprosy field workers throughout the country for their untiring efforts to trace patients and their compassion toward those suffering from leprosy. Without their devotion to their task, this review would not have been possible.
REFERENCES
1. CHEN, J. K., WANG, S. Y., HOU, Y. H., NI, G. X., ZHANG, J. L. and TANG, Q. G. Primary dapsone resistance in China. Lepr. Rev. 60(1989)263-266.
2. JI, B. H., ZHANG, J. L., HOU, Y. H., NI, G. X. and ZHANG, R. Secondary dapsone resistance in Shanghai Municipality. Lepr. Rev. 4(1983)197-202.
3. LI, H. Y., YU, X. L., ZIIANG, M. S., DUAN, C. X., HUANG, W. B., ZIIANG, S. B., Ziiu, K. and MA, J. F. Shortterm MDT in multibacillary leprosy; review of 80 cases in two provinces of China. Int. J. Lepr. 57(1989)622-627.
4. LIU, W. C. Relapse of leprosy in Guangdong Province. China Lepr. J. 7(1991)153-155.
5. SRINIVASAN, FL RAO, K. S. and IYER, C. G. S. Discrepancy in the histopathologycal features of leprosy lesions in the skin and peripheral nerve. Lepr. India 54(1982)275-286.
6. WU, X. S. and HU, L. F. Leprosy control in Sichuan Province, 1984-1988. China Lepr. J. 6(1990)65-68.
7. ZIIENG, D. Y., CHEN, S. M. and MAO, Z. M. Study of relapse among 7, 445 clinically cured leprosy patients in Weifang, Shandong Province, China. (Abstract) Int. J. Lepr. 57(1989)424.
1. M.D., M.P.H., Leprosy Unit, Beijing Tropical Medicine Research Institute, 95 Yun An Lu, Beijing, China.
Received for publication on 19 August 1992.
Accepted for publication in revised form on 5 Januarv 1993.