- Volume 61 , Number 1
- Page: 20–4
Cataract surgery in a leprosy population in Liberia
ABSTRACT
In Liberia, 43 eyes of 30 patients with ocular leprosy underwent cataract extraction; 33 eyes had extracapsular cataract extraction (ECCE) and 10 eyes had intracapsular cataract extraction (ICCE). ICCE was performed in eyes with poor visualization of the anterior chamber. In 95% of the eyes, the postoperative vision improved by 2 Snellen lines or more, but functional visual acuity (better than 20/200) was achieved in only 65% (82% post-ECCE and 10% post-ICCE). Fewer postoperative complications were observed after ECCE. These findings may have been related to less ocular involvement by leprosy preoperatively. ECCE should be attempted when the visualization of the anterior chamber is fair.RÉSUMÉ
On a opéré pour cataracte au Libéria 43 yeux de 30 malades de la lèpre; on a réalisé pour 33 yeux une extraction extracapsulairc de la cataracte (EECC) et pour 10 yeux une extraction intracapsulaire (EICC). L'EICC a été réalisée pour les yeux où la chambre antérieure était mal visualisée. Pour 95% des yeux, la vision post-opératiorc s'est améliorée d'un score de 2 lignes Snellen, mais l'acuité visuelle fonctionnelle (plus de 20/200) n'a été atteinte que dans 65% des cas (82% après EECC et 10% après EICC). On a observé moins de complications post-opératoires après EECC. Ces observations pourraient être liées à un moindre envahissement oculaire par la lèpre en pré-opératoire. L'EECC devrait être tentée lorsque la visualisation de la chambre antérieure est convenable.RESUMEN
En Liberia, 43 ojos de 30 pacientes con lepra ocular se sometieron a extracción de cataratas; 33 ojos tuvieron extracción extracapsular de catarata (EECC) y 10 ojes tuvieron extracción intracapsular de catarata (EICC). La EICC se efectuó en ojos con pobre visualización de la cámara anterior. En el 95% de las ojos la visión postoperativa mejoró en 2 lineas Snellen o más, pero la agudeza visual funcional (mejor de 20/ 200) sólo se alcanzó en el 65% de los casos (82% post-EECC y 10% post-EICC). También se observó que las menores complicaciones postoperatorias ocurrieron después de la EECC; ésto pudo haber estado en relación con menos afección ocular antes de la operación. La EECC debe intentarse cuando la visualización de la cámara anterior es buena.The incidence of ocular involvement in patients with leprosy has varied from as low as 6% (13) to as high as 90% (5). Since many of these patients have amputated limbs, vision becomes extremely important for their rehabilitation. Few studies have reported the visual complications of leprosy in Africans (2,9,13) and none have addressed the visual outcome following cataract surgery. We report the results of cataract surgery in a leprosy population in Liberia.
PATIENTS AND METHODS
Two-hundred-forty patients with leprosy were hospitalized and treated in the Rehabilitation Center for Leprosy in Mcthodistic Hospital in Ghanta, Liberia. Of this population, 125 patients with ocular complaints were examined between January 1985 and December 1986. Thirty patients, 17 men and 13 women, ranging in age between 30 to 65 years old (mean 48 years) had significant cataracts in 43 eyes and underwent cataract extraction. Of this group, 18 patients had lepromatous leprosy, 8 had borderline leprosy, and 4 had tuberculoid leprosy. At the time of the surgery, all patients had negative skin tests and had been treated with the usual antileprosy treatment.
Preoperatively, each patient underwent an ophthalmic evaluation including visual acuity, slit-lamp examination, and intraocular pressure (IOP) measurement by Schiotz tonometry. The view of the fundus was obscured by a dense cataract in all examined eyes.
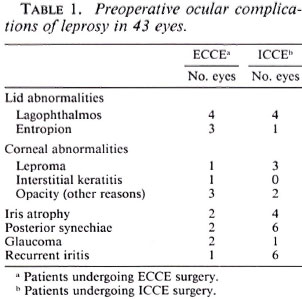
Preoperative visual acuity was 25 cm to 1 meter finger count in 9 eyes and hand movements or less in 34 eyes. Mature, intumescent, or hypermaturc cataracts were observed in all except three eyes which had moderately cloudy corneas and progressive cataracts. The intraocular pressure was greater than 22 mmHg in three eyes. The ocular complications of leprosy in 43 eyes are presented in Table 1.
All surgery was performed by one surgeon (JF-P). Extracapsular cataract extraction (ECCE) was performed in 33 eyes of 22 patients (with combined trabeculectomies in 2 eyes) and intracapsular cataract extraction (ICCE) in 10 eyes of 8 patients. ECCE was routinely attempted in all except 3 eyes of 2 patients with cloudy corneas. In these eyes planned ICCE was performed.
Lignocainc 2% was used for retrobulbar block (3 to 4 ml) and for akinesia of the lids (O'Brien modification-5 ml). A fornixbased conjunctival flap was made followed by limbal groove from 11 to 2 o'clock, then the anterior chamber (AC) was entered with a blade. Anterior synechiae were broken with a cyclodialysis spatula. If the iris was atrophic and the pupil remained small following synechialysis, or the visualization of the iris structures was markedly reduced, the limbal groove was extended, one preplaced 8-0 silk suture was used and sector iridectomy was performed followed by ICCE using a disposable cryoprobe (7 eyes of 6 patients). In the remaining 33 eyes of 22 patients anterior capsulotomy, with a 25gauge bent needle, was performed under irrigation. The limbal wound was enlarged to 10 mm and the nucleus was extracted by simultaneous depression of the sclera with 0.12 corneal forceps at the level of the limbal incision and with a muscle hook at 6 o'clock. The liquefied cortex was irrigated with a 23-gauge cannula connected to a bulb filled with saline. In most eyes, the AC was free of cortical material and the wound was sutured. When residual cortical material remained in the AC, it was irrigated and aspirated with coaxial I/A cannula (Visitec, Florida, U.S.A.). Optical iridectomies were performed when necessary. The wound was sutured with separate 8-0 or 10-0 sutures (total 5 to 6 sutures for ECCE and 8 to 10 sutures for ICCE) and 5% chloramphenicol ointment was applied into the lower fornix.
Postoperatively patients remained in the rehabilitation center (for at least 6 months) and were treated with topical chloramphenicol 0.5% four times a day, 1% atropine sulfate four times a day, and topical dexamethasone phosphate 0.1%, six times a day for 1 week. Then the chloramphenicol 0.5% was discontinued and the other drops were used four times a day for 2 more months, then tapered and stopped after a total period of 4 months. The patients were followed at 1 week, 1, 2 and 3 months, then every 3 months, or as needed in case of postoperative complications. Each postoperative examination included: visual acuity taken with a +10.00 diopter lens, IOP measurement, and indirect and direct ophthalmoscopy of the posterior pole. Refraction was not performed in these patients. The patients were followed for 6-18 months, and the last examination of each patient was used for the evaluation of the results.
RESULTS
Of 240 patients in the Ghanta Leprosy Center, 125 underwent eye examination. In 57 patients (23.75%) cataractous changes were discovered and 43 eyes of 30 patients (12.5%) underwent cataract surgery.
Postoperatively all eyes except two gained at least two lines of vision (corrected with + 10.00 diopter lens). Of the total 43 eyes, 28 (65%) had functional visual acuity of better than 20/200 (Table 2).
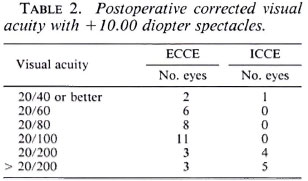
In the group that underwent ECCE, 12 of the 22 patients had lepromatous leprosy, 7 patients had borderline leprosy and 3 had tuberculoid leprosy. Of the 33 eyes in this group, 2 eyes had synechialysis, 3 had optic iridectomies, and 2 had combined ECCE + trabeculectomy. Postoperatively 27 eyes (82%) had functional visual acuity but only two (6%) had vision better than 20/40 (Table 2). In three eyes (9%), the visual acuity was less than 20/200 as a result of optic atrophy, macular scar, and glaucoma.
In the group that underwent ICCE, 6 of the 8 patients had lepromatous leprosy, 1 patient had borderline leprosy and 1 had tuberculoid leprosy. Of 10 eyes in this group, 6 eyes had synechialysis, 3 eyes had optic iridotomies, and 1 had vitreous loss. Postoperatively only one eye (10%) had vision better than 20/200 and four eyes (40%) had vision of 20/200. In five eyes (50%), the vision was less than 20/200 (range of finger count between 1 to 5 meters). Of these 5 eyes, 2 had significant corneal leproma, 1 had optic atrophy, 1 had glaucomatous optic atrophy and 1 had chronic iritis.
Fifteen eyes of 11 patients had postoperative complications (Table 3). Seven eyes (6 patients) had complications post-ECCE and eight eyes (5 patients) had complications following ICCE. Six eyes had postoperative glaucoma (3 post-ECCE, 3 post-ICCE) and were controlled with topical timolol 0.5%, pilocarpine 2% to 4% and oral acetazolamide. In one case, intraocular pressure was steroid induced and dropped to normal levels after steroids were discontinned. Two patients had post-ICCE iritis. Both had a history of iritis prior to the surgery and postoperatively were controlled with topical steroids during the follow-up period.
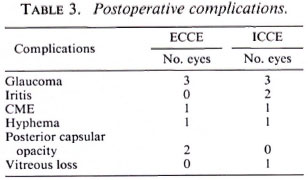
Clinically significant cystoid macular edema (CME) was observed in 2 eyes (1 post-ECCE, 1 post-ICCE). Two patients had postoperative hyphemas (1 post-ECCE, 1 post-ICCE) that cleared within 3 days. Two eyes post-ECCE had mild posterior capsular opacifications after 2 and 4 months, but neither had a loss of visual acuity. One eye post-ICCE had vitreous loss. No cases of endophthalmitis were observed.
DISCUSSION
In Africa, ocular leprosy has been reported to be less prevalent than in Asia (1,3,5,7.8,13,14). Cataract surgery has not been documented in this population. In the Ghanta Rehabilitation Center (Liberia) the majority of the patients are handicapped and some are immobile. All patients were available for ocular examinations for at least 6 months. Since no ophthalmologist had been attainable in this area for at least 7 years, it is not surprising that almost 24% of this population had cataracts and 14% needed cataract extraction. Significant lenticular opacities in a lepromatous population have ranged from 29%-79% (1,3,7,8,11,14). These findings may reflect the natural history of cataract formation in leprosy in different races, the severity of ocular leprosy involvement, or the accessibility of ophthalmic treatment in different populations.
When eyes after ICCE and ECCE were placed into one group, 65% had vision better than 20/200. All eyes except two gained at least 2 lines of vision. Furthermore, of the 43 eyes that were corrected with a + 10.00 diopter lens, 28 (65%) had functional visual acuity of better than 20/200. If refracted, better vision would probably have been achieved, but (at the present time) the standard aphakic spectacles of + 10.00 diopter power are the only optical device available for this population.
A large variety of visual results (functional vision in 27%-80%) following cataract surgery in leprosy populations has been reported (4,10,12). The postoperative visual results are probably related to the variability of the types of leprosy in different populations, to the preoperative ocular involvement by leprosy, the different inclusion criteria for cataract surgery, the use of different surgical techniques, or the quantities of postoperative use of corticosteroids (4,10,12). Blindness with visual acuity of hand motion or less coupled with severe involvement of limbs results in an extreme form of disability. Therefore, any postoperative visual acuity, of even finger count, is of great importance for rehabilitation of these handicapped patients.
Of the 30 patients in this study, 18 (60%) had lepromatous leprosy. However, the lepromatous leprosy group comprised 75% of those who underwent ICCE and 55% of patients who had ECCE surgery. Of the leprosy population, lepromatous leprosy presents the most severe involvement of the eye. It is not surprising, therefore, that a majority of the patients who underwent ICCE because of the inability to perform ECCE belonged to this group. These eyes had severe manifestations of ocular leprosy (Table 1) including: cloudy corneas; small pupils; atrophic, nonresponsive and easily breakable irises. Postoperatively 8 of the 10 eyes after ICCE had complications (Table 3) and 9 (90%) of these eyes had vision of 20/200 or less. The rate of complications, the poor visual acuity post-ICCE, and the fact that four fellow eyes in these patients lost their sight reflects the more serious ocular disease in patients with advanced lepromatous leprosy (Table 1).
Planned ECCE had not been reported previously in patients with leprosy, possibly due to the prevalence of leprosy in communities with limited resources where operating microscopes and aspiration and irrigation units are not available. In addition, ECCE in eyes with corneal haze and atrophic, nonrcactive iris may be a very complicated procedure.
In this study ECCE was performed only when it was technically possible. Although 12 of the 22 patients had lepromatous leprosy, preoperative evaluation revealed only mild or moderate ocular complications of leprosy (Table 1). Postoperatively, 30 of these eyes (91%) had visual acuity of 20/ 200 or better, not differing from a healthy population who also underwent cataract surgery and received standard aphakic spectacles (12). Seven of the 33 eyes after ECCE had nonsignificant postoperative complications that could easily be controlled (Table 3). It is impossible to compare the complications of the ICCE group to those of the ECCE group because the patients in the former group had such severe eye disease that it was impossible to perform ECCE. Obviously the ICCE group had more postoperative complications. However, none of the complications in this study was severe.
Postoperative glaucoma was controlled with medication in six eyes. Hyphema (two eyes) cleared within the first postoperative week. Persistent postoperative iritis manifested in two eyes (6%) with preoperative iritis. The inflammation was controlled with topical steroids during the follow-up period. Two eyes (6%) had mild postoperative opacification of the posterior capsule without loss of visual acuity. If vision becomes compromised in the future, capsulotomy should restore the sight. We noticed the low incidence of opacification of posterior capsules post-ECCE in mature and hypermature cataracts in the healthy black population in Africa (unpublished data) as did Hemo (6) in a similar population in Swaziland. Various rates of complications postcataract surgery in populations with leprosy have been reported in other studies (3,10,12) However, severe postoperative complications which were reported in these studies, such as endophthalmitis or opacification of the cornea (3,10), shallow anterior chambers (10,12), retained lens material in the anterior chamber or retinal detachments (12), were not observed in our patients.
In Liberia the operated patients were observed monthly for at least 6 months, which would allow medical or surgical intervention had complications occurred. These ideal circumstances are unusual in Third World countries. One should consider the postoperative complications in terms of the ability of the patient to present for examination as well as the availability of an ophthalmic surgeon in the district after the surgery is done. ECCE has the disadvantage of possible secondary capsular opacities which are less common and less opaque than in the Western population; furthermore, it may reduce the sight but does not cause blindness as do other complications. ICCE has greater rates of other complications such as cystoid macular edema or retinal detachment. All of these complications can be treated but sometimes may lead to blindness, particularly when an ophthalmologist is unavailable. Regardless of these unfortunate circumstances, the surgeons in these parts of the world should perform as many ECCE or ICCE surgeries as they can, and perhaps train other medical staff to follow the patients when the ophthalmologist is not available.
The use of the operating microscope for ICCE or ECCE is advantageous over the abexterno technique (11) or ICCE with cryoprobe without the microscope (10). However, it does not necessarily replace these techniques. This study suggests that cataract surgery should be encouraged in lepromatous patients. While ECCE is advised in less complicated cases, ICCE is suggested in the rest of the patients.
REFERENCES
1. DE BARROS, M. J. The ocular complications of leprosy. Am. J. Opthalmol. 29(1946)162-170.
2. EMIRU, V. P. Ocular leprosy in Uganda. Br. J. Ophthalmol. 54(1970)740-743.
3. FFYTCHE, T. J. Cataract surgery in the management of the late complications of lepromatous leprosy in South Korea. Br. J. Ophthalmol. 65(1981)243-248.
4. FFYTCHE, T. J. Cataract surgery in leprosy patients. J. R. Soc. Med. 59(1988)67-70.
5. HARLEY, R. D. Ocular leprosy in Panama; a study of 150 cases. Am. J. Ophthalmol. 29(1946)295-299.
6. HEMO, I. Intraocular lens implantation in an underdeveloped country. J. Cataract Refract. Surg. 13(1987)414-416.
7. HOLMES, W. J. Leprosy of the eye. Trans. Am. Ophthalmol. Soc. 55(1957)145-161.8. Hornblass, A. Ocular leprosy in South Vietnam. Am. J. Ophthalmol. 75(1973)478-480.
9. MCLAREN, D. S., SHAW, M. J. and DALLEY, K. R. Eye disease in leprosy patients; a study in central Tanganyika. Int. J. Lepr. 29(1961)21-28.
10. RAO, V. A. and KAWATRA, V. K. Cataract extraction in leprosy patients. Lepr. Rev. 59(1988)67-70.
11. SHIELDS, J. A., WARING, G. O, III and MONTE, L. G. Ocular findings in leprosy. Am. J. Ophthalmol. 77(1974)880-890.
12. SURYAWANSHI, N . and RICHARD, J. Cataract surgery on leprosy patients. Int. J. Lepr. 56(1988)238-242.
13. TICHO, U. and BENSIRA, I. Ocular leprosy in Malawi. Br. J. Ophthalmol. 54(1970)107-112.
14. WEEKEROON, L. Ocular leprosy in Ceylon. Br. J. Ophthalmol. 56(1969)106-113.
1. M.D., Department of Ophthalmology, Hadassah University Hospital, P.O. Box 12000, 91120 Jerusalem, Israel.
2. M.D., University of California San Diego, La Jolla, California, U.S.A.
Received for publication on 9 September 1992.
Accepted for publication in revised form on 5 January 1993.