- Volume 61 , Number 3
- Page: 428–32
Ambiguities in leprosy histopathology
ABSTRACT
This paper presents the percentage of definite or suggestive evidence present in 482 biopsies f rom different types of leprosy. The presence of acid-fast bacilli (AFB) and nerve involvement were taken as definite features for a diagnosis of leprosy, and infiltration of the dermal appendages, neurovascular bundles and dermis by granuloma cells and lymphocytes were regarded as suggestive signs of leprosy. Using these criteria, all cases were categorized into three groups having definite, suggestive, or no signs of leprosy. The results showed definite and suggestive features in 72.2% and 14.1% of the cases, respectively. The remaining 13.7% had none of these signs. These cases were mostly healed lesions. Large, epithelioid cell granulomas without any nerve element present and healed cases proved difficult for a definite diagnosis. Emphasis is placed on searching for residual nerve elements in AFB-negative sections because this increases the certainty level of the diagnosis. Also, it is suggested that for uniformity of understanding and reporting, terminologies need to be narrowed down and restricted to only definite, suggestive, or no diagnosis of leprosy.RÉSUMÉ
Cet article présente les le pourcentage de signes certains ou suggestifs présents dans 482 biopsies obtenues chez des patients présentant différents types de lèpre. La présence de bacilles acido-résistants (BAR) et l'envahissement de nerfs ont été considérés comme des signes de certitude de lèpre, et une infiltration des appendices dermiques, des paquets neurovasculaires et du derme par des cellules granulomatcuses et des lymphocytes comme des signes suggestifs de lèpre. Sur base de ces critères, tous les cas ont été classés en trois catégories: signes certains, signes suggestifs, ou pas de signe de lèpre. Les résultats ont montré des signes certains et suggestifs dans respectivement 72.2% et 14.1% des cas. Les 13.7% restants n'avaient aucun de ces signes. Ces cas étaient essentiellement des lésions guéries. De grands granulomes à cellules épithélioïdes sans aucun envahissement nerveux et des cas guéris ont posé des problèmes difficiles pour un diagnostic de certitude. On insiste sur la recherche d'éléments nerveux résiduels dans les coupes ne présentant pas de BAR parce que ceci augmente le degré de certitude du diagnostic. On suggère également que pour l'unité de la compréhension et de la notification, la terminologie utilisée soit plus restreinte et limitéc sculement á lépre certaíne, probable, ou pas de lepre.RESUMEN
En este trabajo se presenta cl porcentaje de evidencias definitivas o sugestivas encontradas en 482 biópsias de diferentes tipos de lepra. La presencia de bacilos ácido resistentes (AFB) y la lesión de nervios se to¬ maron como características definitivas para cl diagnóstico de lepra, y la infiltración de los anexos dérmicos, de los haecs neurovasculares y de la dermis misma por células de granuloma y por linfocitos, se considero como un signo sugestivo de la lepra. Usando estos critérios, todos los casos se catalogaron dentro de tres grupos según tuvieran signos definitivos o sugestivos de la lepra, o carência de ellos. Los resultados mostraron evidencias definitivas de la lepra en el 72.2% de los casos y sugestivas en el 14.1% de los mismos. Los casos restantes (13.7%) no tuvieron ninguna evidencia de la enfermedad. Estos casos correspondieron en su mayoría a lesiones resueltas. Los granulomas grandes con células epiteloides pero sin ningún elemento nervioso presente, y los casos correspondientes a lesiones resueltas, resultaron de difícil interpretación para establecer un diagnóstico definitivo. Se pone énfasis en la búsqueda de elementos nerviosos residuales en las secciones AFB-negati vas porque esto incrementa los niveles de certidumbre en el diagnóstico. También se sugiere restringir las terminologías a solo definitiva, sugestiva, o sin diagnóstico de lepra, para uniformizar los criterios y reportes.Confirmation of diagnosis in doubtful cases of leprosy is an important indication for histopathological examination. Diagnosis of this disease is invariably associated with medical, social, and psychological implications for a person. Hence, a diagnosis of leprosy should not be made without a certain degree of certainty. As in any other disease, the pathologist is expected to give a final diagnosis, but in reality he has also many limitations and the section may not show what he looks for. This creates several areas of ambiguity for him and limits his abilities to give a definite diagnosis. Added to this, a clear-cut definition of absolute diagnostic criteria and a common nomenclature for reporting are also lacking in this disease. Isolated reports pertaining to interobserver variations in leprosy histopathological diagnosis are alarming (4). It will be of great use to categorize the histopathological features into those that are diagnostic and those which are just suggestive of leprosy. Further, it will be interesting to learn the frequency with which these features are encountered by a pathologist during histopathological examination. In this respect, our observations on these aspects of the histopathological diagnosis of leprosy are presented.
MATERIALS AND METHODS
The study is based on the findings from 482 skin biopsies from clinically diagnosed leprosy cases who attended Regional Leprosy Training and Research Institute, Raipur, India. Four-hundred-twenty-two cases were clinically active, and the remaining 60 were inactive at the time they were subjected to biopsy. The clinically active cases were registered for multidrug therapy. The skin lesions selected for biopsy were both macular and infiltrated, although the larger number of biopsies were from the infiltrated lesions. The biopsies were adequate in size and were processed as per standard procedure. Two sections (one stained with hematoxylin and cosin, the other with Fite-Faraco stain) were examined from the biopsy material.
Regarding criteria for diagnosis, the presence of acid-fast bacilli (AFB) and/or nerve involvement were taken as definite evidence of leprosy. Granulomatous or lymphocytic infiltration of dermal appendages, neurovascular bundles, and the dermis were regarded as suggestive features of the disease. Each section was thoroughly examined for these features and relevant observations were recorded. Depending on the presence of cither definite evidence or suggestive evidence, all of the cases were separately grouped and analyzed.
RESULTS
Based on various histopathological characteristics observed in the 482 biopsies, all of the cases were divided into three groups: cases with macrophage infiltrate, 148 (30.7%); epithelioid cell granuloma, 266 (55.2%); and those lacking cither of these features, 66 (14.1%) (The Table). These groups were divided further into three subgroups each on the basis of diagnostic criteria: cases with definite features; cases with suggestive features; and cases with neither definite nor suggestive features. Of the 124 cases with macrophage granuloma with definite signs, 120 showed AFB and the remaining 4 had only nerve involvement. Similarly, out of the 212 with epithelioid cell granuloma AFB could be seen, on meticulous searching, in only 6 (2.8%) cases; the rest showed varying extents of nerve involvement. In many sections the nerve parenchyma was completely replaced by epithelioid cells and giant cells, the surviving perineurium and isolated Schwann cells could be seen as the death tombs of those affected nerves. In comparatively early cases, the granulomas were elongated and appeared to indicate the remnant of a destroyed nerve. The third group of cases showed only lymphocytic infiltration but no granuloma (Figs. 1-3). The evidence of nerve involvement could be appreciated in the forms of perineural cuffing and Schwann cell disorganization. We failed to notice AFB even after examination of more than 100 fields covering the entire length and breadth of the section.
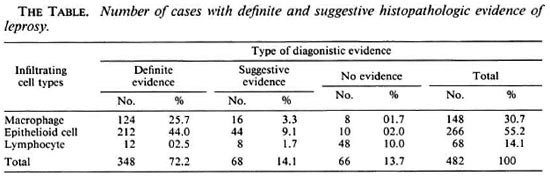

Fig. 1. Complete replacement of nerve parenchyma and surviving perineurium are shown.
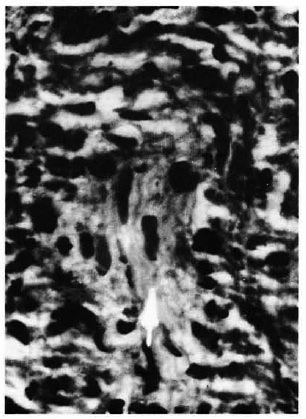
Fig. 2. Isolated Schwann cells within a granuloma are seen.
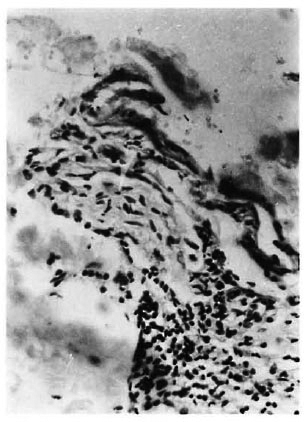
Fig. 3. Schwann cell disorganization with perineural infiltration of lymphocytes can be seen.
There were 68 cases showing only suggestive features of leprosy (The Table). These were infiltration of dermal appendages, neurovascular bundles, and the dermis by epithelioid cells, macrophages or lymphocytes. These lesions made up 14.1% of all cases.
There were 66 cases showing neither definite nor suggestive evidence of leprosy, and they constituted 13.7% of the total cases. These biopsies were mostly from the healed cases of leprosy. We observed only a few macrophages, epithelioid cells, and lymphocytes in these sections. The cells were too few in number to form an organized granuloma, and were not associated with nerves or dermal appendages. Hence, these cases were not taken as features suggestive of leprosy. These cases also showed atrophy of the dermis and dermal appendages.
To sum up the observations, as shown in The Table definite diagnostic evidence was seen in 72.2% of the cases, suggestive features were found in an additional 14.1% of the cases, and no diagnostic features were found in the remaining 13.7% of the cases.
DISCUSSION
Diagnosis and classification of leprosy are the two main indications of histopathological examination; the former deserves more attention because it makes the decision of a case or noncase. For an infectious disease the absolute diagnostic test would be to demonstrate its causative organism. Unfortunately, this is not true with leprosy. In almost three quarters of the cases Mycobacterium leprae, the causative agent of the disease, is too scarce to be demonstrated by routine skin-smear examination. The cases mostly include tuberculoid and indeterminate types, and bacilli are rarely seen in tissue sections of these cases. This emphasizes the need for some other definite criteria of diagnosis.
The neurotrophic nature of M. leprae is a unique and well-accepted fact. With present-day knowledge M. leprae is the only bacterium known to infect peripheral nerves(2, 5, 7, 10). It has also been stated that in indeterminate and tuberculoid lesions the key to diagnosis is nerve involvement (9). This may be in the form of Schwann cell disorientation, perineural infiltration, or the presence of bacilli in a nerve. These facts emphasize that the involvement of the nerve is a definite sign of leprosy. Other features constantly found in skin lesions of leprosy are infiltration of dermal appendages, neurovascular bundles, and the dermis by macrophages, epithelioid cells and lymphocytes. These features are not unique to leprosy and, hence, they are taken as suggestive evidence of the disease.
The vertical columns in The Table show groupings of the cases on the basis of definite or suggestive histopathological evidence. From The Table it is evident that the cases positive for AFB and showing nerve involvement together constituted 72.2% of the total cases. Our observation is comparable to the results of an important study (4) in which three experienced pathologists examined 143 biopsies from leprosy suspects in Malawi. In 82 of their clinically certain cases their agreement for a definite diagnosis ranged from 63% to 83%. When the opinions on the entire 143 cases were considered the certainty of diagnosis was found to be 39% to 58%. McDougall, et al. (2) reported that they could make a definite diagnosis in 354 of 686 (52%) cases detected in a population survey. Although these figures are low compared to that of the present study, they are not unusual in view of the source of their biopsy materials. Our study is institution-based; the self-reporting cases in an institution are likely to be far advanced with definite lesions compared to cases detected by survey (6).
Infiltration of dermal appendages, neurovascular bundles, and the dermis are commonly found in leprosy lesions. We observed these features in 14.1% of cases. This is comparable with the observation of Mc-Dougall, et al. (6), who found suggestive but inconclusive signs in 17% of their cases. Regarding the value of a suggestive diagnosis, it may supplement the clinical impression and assist the clinician in making an aggregate decision.
We had 13.7% of our cases with no histopathological evidence of leprosy. These biopsies were mostly from clinically regressed cases. Some of the cases had a few scattered macrophages or epithelioid cells, their numbers being too small to qualify for a granuloma. The remaining cases showed oily aggregates of lymphocytes. The dermal appendages and epidermis were atrophic. Such nonspecific features are common in healed lesions (1, 3). The availability of powerful drugs has made leprosy a curable disease. From the histologist's point of view the above cases are cured ones.
So far as the areas of uncertainty are concerned, 14 (5.3%) of our cases had epithelioid cell granulomas with no traces of neural structure left. This has been the experience with other workers also (9-10). Focal infiltration of the dermis by lymphocytes and granuloma cells, a rare occurrence in dermatopathology, can be viewed as a feature of high-resistance tuberculoid leprosy (8). We had 8 (3%) cases with epidermal involvement. The above features sufficiently point toward leprosy, but in the absence of nerve involvement and AFB they could only be included in the group with suggestive evidence. The other ambiguous group was the healed case in whom there is certain cellular activity but the patient continues to be identified as a case.
This study is an exercise to find the extent to which a pathologist is able to give a definite or suggestive diagnosis of leprosy on the basis of histological changes alone. In no way does it ignore the value of clinicalpathological correlation in the diagnosis of this disease.
To ensure comparability, a uniform expression of observations is needed and the reporting language needs to be narrowed down. The report must indicate either definite or suggestive diagnosis, depending on the qualifying features stated above. If the section shows AFB, a definite diagnosis is no problem. Opinions are prone to vary in the interpretation of nerve involvement. In our experience, even in a single section the amount of patience needed to examine the entire section and the ability to recognize the residual nerve elements are rewarding. Such a time-consuming exercise is worth doing because it makes the report decisive and increases the certainty level of the diagnosis.
REFERENCES
1. AZULAY, R. D. Histopathology of skin lesions in leprosy. Int. J. Lepr. 39(1971)244-250.
2. BINFORD, C. H. The histologic recognition of early lesion of leprosy. Int. J. Lepr. 39(1971)225-230.
3. DESIKAN, K. V. Clinicopathological correlation in Indian consensus classification. Indian J. Lepr. 63(1991)329-332.
4. FINE, P. E. M., JOB, C. K., MCD OUGALL, A. C, M EYERS, W. M. and PONNINGHAUS, J. M. Comparibility among histopathologists in the diagnosis and classification of lesions suspected of leprosy in Malawi. Int. J. Lepr. 54(1986)614-625.
5. JOB, C. K. and DHARMENDRA. Histopathology of skin lesions in leprosy. In: Leprosy Vol. II. Bombay: Samant & Company, 1985, p. 818.
6. MCDOUGALL, A. C, PONNINGHAUS, J. M. and FINE, P. E. M. Histopathological examination of skin biopsies from an epidemiological study of leprosy in northern Malawi. Int. J. Lepr. 55(1987)88-98.
7. PEARSON, J. M. H. and Ross, W. F. Nerve involvement in leprosy-pathology, differential diagnosis and principles of management. Lepr. Rev. 46(1975)199-212.
8. RIDLEY, D. S. Pathology and bacteriology of early lesions in leprosy. Int. J. Lepr. 39(1971)216-244.
9. RIDLEY, D. S. Diagnosis and differential diagnosis (of leprosy). In: Skin liiopsy of Leprosy. Basle: CIBA-GEIGY Ltd., 1977, p. 29.
10. WIERSEMA, J. P. and BINFORD, C. H. The identification of leprosy among epithelioid cell granuloma. Int. J. Lepr. 40(1972)10-32.
1. M.D.; Regional Leprosy Training and Research Institute, Raipur 492001, India.
2. M.B.B.S.; Regional Leprosy Training and Research Institute, Raipur 492001, India.
Reprint requests to Dr. Reddy.
Received for publication on 9 September 1992.
Accepted for publication in revised form on 3 May 1993.