- Volume 61 , Number 3
- Page: 433–8
Clinical and histopathological correlation in the classification of leprosy
ABSTRACT
This study reports our observations on the correlation between clinical and histopathological diagnoses of the classification of leprosy. The histopathological classification of leprosy in 1351 cases was done per Ridley-Jopling criteria and was compared with the clinical diagnoses of the same cases. These 1351 cases included 79 cases diagnosed clinically as having a "reaction." However, the histopathologists could not detect any evidence of reaction in 16 of these 79 cases (20%).Of the remaining 1272 cases, 68 (5%) were reported as "no evidence of leprosy" by the histopathologists; 37 of these 68 were found to be f rom the clinically indeterminate type of leprosy. Histopathological and clinical diagnoses of the classification of leprosy coincided in 69% of the cases. Concordance between the clinical and histopathological diagnoses for different types of leprosy was: indeterminate (I) = 36%, tuberculoid (TT) = 50%, borderline tuberculoid (BT) = 77%, borderline (BB) = 26%, borderline lepromatous (BL) = 43%, and lepromatous (LL) = 91%. When some of the types were combined (BT with TT, BL with LL), the overall concordance figure was 76%; concordance for the TT/BT group was 80%, for the BL/ LL group it was 93%. Since both TT and BT are considered paucibacillary and LL or BL are considered multibacillary for treatment purposes, differentiating TT f rom BT or BL f rom LL is, perhaps, therapeutically irrelevant. However, for classification purposes it appears that the weight given to different signs and/or histopathological parameters for classifying leprosy cases (especially TT, BB and I) needs to be reassessed.
RÉSUMÉ
Cette étude rapporte nos observations relatives à la corrélation entre les diagnostics clinique et histopathologique de la classification de la lèpre. La classification histopathologique de la lèpre a été réalisée chez 1351 patients selon les critères de Ridley-Jopling et a été comparée au diagnostic clinique des mêmes cas. Ces 1351 cas comprenaient 79 cas diagnostiqués cliniquement comme ayant une "réaction." Cependant, les histopathologistes ne purent détecter aucun signe de réaction pour 16 de ces 79 cas (20%).Pour les 1272 cas restants, 68 (5%) furent rapportés comme n'ayant "pas de signe de lèpre" par les histopathologistes; trente-sept de ces 68 étaient du type clinique indéterminé. Les diagnostics histopathologique et clinique de la classification de la lèpre coïncidaient dans 69% des cas. La concordance entre les diagnostics clinique et histopathologique était la suivante pour les différents types de lèpre: indéterminé (1) = 36%, tuberculoide (TT) = 50%, borderline tuberculoide (BT) = 77%, borderline (BB) = 26%, borderline lepromateux (BL) = 43%, et lepromateux (LL) = 91%. Quand on a combiné certains types (BT avec TT, BL avec LL), le taux de concordance globale était de 76%; la concordance pour le groupe TT/BT était de 80%, et pour le groupe BL/LL de 93%. Puisque TT et BT sont tous deux considérés comme paucibacillaires et LL et BL comme multibacillaires en ce qui concerne le traitement, différencier TT de BT ou BL de LL est peut-être sans intérêt sur le plan thérapeutique. Cependant, dans des buts de classification, il apparaît que le poids donné à différents signes et/ou paramètres histopathologiques pour classer les cas de lèpre (particulièrement TT, BB et 1) a besoin d'être réévalué.
RESUMEN
Este estudio se refiere a nuestras observaciones sobre la correlación entre los diagnósticos clínico e histopatológico en relación a la clasificación de la lepra. Siguiendo los criterios de Ridley Y Jopling se hizo la clasificación histopatológica de 1351 casos de lepra y se comparó con la clasificación clínica de los mismos casos. Aunque dentro de estos 1351 casos se incluyeron 79 diagnosticados clínicamente como casos "en reacción," los histopatólogos no pudieron detectar ninguna evidencia de reacción en 16 de estos 79 casos (20%).De los 1272 casos restantes, 68 (5%) se reportaron como "sin evidencias de lepra" por los histopatólogos; 37 de estos 68 casos fueron clínicamente diagnosticados como lepra indeterminada. Los diagnósticus clínico e histopatológico coincidieron en el 69% de los casos. La concordancia entre los diagnósticos clínico e histopatológico para los diferentes tipos de lepra fue como sigue: indeterminada (I) = 36%, tuberculoide (TT) = 50%, tuberculoide subpolar (HT) = 77%, intermedia (BB) = 26%, lepromatosa subpolar (BL) = 43%, y lepromatosa (LL) = 91%. Cuando se combinaron algunos de los tipos (BT con TT, BL con LL), la cifra de concordancia general fue del 76%; la concordancia para el grupo TT/BT fue del 80%, mientras que para el grupo BL/LL fue del 93%. Puesto que para propósitos de tratamiento tanto TT como BT se consideran paucibacilares y BL y LL se consideran multibacilares, diferenciar entre TT y BT o entre BL y LL es, quizá, terapéuticamente irrelevanle. Consideramos que el peso que se le dá a los diferentes signos y parámetros histopatológicos con motivos de clasificación de los casos de lepra (especialmente TT, BTe I) necesita una revaloración.
Leprosy is an infectious disease primarily affecting the skin and the nerves. The cellular characteristics in leprosy lesions are related to the immunological status of the patient. Ridley and Jopling proposed a histological classification reflecting the immunological spectrum (8), and this classification has been widely accepted by leprologists and histopathologists. Simultaneously, clinicians also have adopted the Ridley-Jopling nomenclature and, at present, the clinical diagnosis is being made along the lines of Ridley-Jopling classification even when a histopathologic examination has not been done. Subsequently, a number of studies have attempted to correlate this histological classification with the clinical picture of leprosy (2, 3, 7, 9,10). Results of these studies have not been uniform, and in some of these studies the sample sizes have been rather small. Research in leprosy demands accurate classification of the types of leprosy and, in this paper, we report a retrospective analysis of our data in order to assess the concordance between clinical and histopathologic classifications in leprosy.
MATERIALS AND METHODS
During the periods 1979-1981 and 1984-1987, 1553 skin biopsies from leprosy patients "reported as untreated" were done at Central JALMA Institute for Leprosy (CJIL), Agra, India, and these patients had been clinically examined and classified (8) before a biopsy was done. These biopsies were reported on by two pathologists -pathologist A during 1979-1981 and pathologist B during 1984-1987. Cases biopsied during 1981-1984 are not included in the analysis.
The histopathologic diagnosis of the types of leprosy was made according to the well laid down criteria of Ridley and Jopling (8). Hematoxylin and eosin as well as Fite-Faraco stained slides were examined for histopathology. Among the 1553 cases reported, there were some instances in which the clinicians had reported a type 1 or type 2 reaction (5). The clinical charts and histopathology reports of these 1553 patients were re-examined and data pertaining to age, sex, clinical classification of the type of leprosy(8), histopathologic classification (8) and reactional status (4, 5) were collected and analyzed using standard statistical techniques with the help of a computer program (Dixon, W. J., et al. BMDP Statistical Software. Los Angeles: University of California, 1987).
RESULTS
Out of the 1553 cases which have been included in the present study, there were 201 cases classified as in-between types (e.g., BT-BB, BB-BL, etc.) either by the clinicians, the pathologists, or both. These were excluded from the analysis. The remaining cases included one case of neuritic leprosy which also was excluded from analysis. Out of the remaining 1351 cases, 79 were diagnosed by the clinicians as having reactions. The results of concordance for these cases are presented.
Table 1 gives the overall association between the clinical and histopathologic diagnoses of types of leprosy for the 1272 cases which did not include any reactional case or any case with an in-between type of classification.
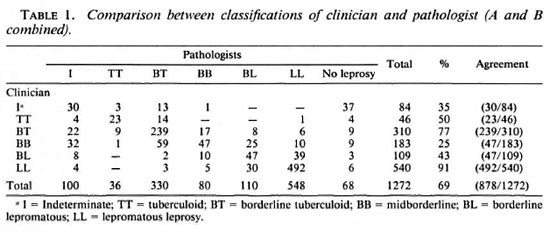
It can be seen that there was an overall concordance of 69%. Concordance figures were very high for LL cases (91%) followed by BT cases (77%). For TT and BL cases, the concordance figures were rather low, 50% and 43%, respectively. Thirty percent of the TT cases were classified as BT and 36% of the BL cases were classified as LL by the pathologists. The observed concordance was minimal for the indeterminate or I (36%) and BB (26%) types of leprosy. The overall concordance was 75% and 72% when BT/ BB, BB/BL (clinical diagnosis) cases were considered as single entities. However, if we consider TT and BT together, and also BL and LL together, the overall figure of concordance was 76%; concordance for the TT/ BT group was 80%, for the BL/LL group, 93%.
The observed concordance between the histopathologic and clinical diagnoses was also analyzed in relation to the age and sex of the patients. The present data did not show any evidence of a relationship of these variables with the concordance between the clinical and histopathologic diagnoses.
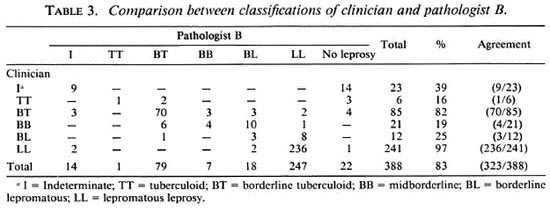
Since the histopathologic diagnosis was made by two different persons, it may be necessary to consider them individually. Tables 2 and 3 give the correlation between the clinical and histopathologic diagnoses with respect to pathologists A and B. Pathologist A (Table 2) had classified 884 biopsies, the remaining 388 were classified by pathologist B (Table 3).
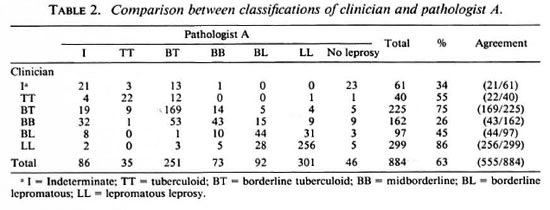
Pathologist A versus clinician. Out of the 884 cases classified by pathologist A, no evidence of leprosy was seen in 46 (5%) biopsies. The overall concordance rate was 63%. A maximum amount of concordance was observed for LL (86%) and BT (75%). A poor rate of concordance was seen in BB (26%) and I (34%) cases; 23 out of 61 (38%) of the I cases were classified as "no leprosy" by the histopathologist. Combining TT with BT cases and BL with LL cases, the overall concordance rate was 72%. For the TT/BT and BL/LL groups, the agreement between the clinician and pathologist A was observed in 80% and 91%, respectively.
Pathologist B versus clinician. Pathologist B classified 388 biopsies; in 22 (6%), no evidence of leprosy was reported. An overall concordance of 84% was observed between pathologist B and the clinician. A high order of concordance was observed for LL cases (98%) followed by 82% for BT cases. Minimal concordance was observed for the I and BB types of leprosy; for 61 % of the indeterminate cases, pathologist B did not find any evidence of leprosy. The combining of TT with BT cases and BL with LL cases resulted in an overall concordance rate of 87%; for the TT/BT group agreement was observed in 80%, for the BL/LL group, 98%.
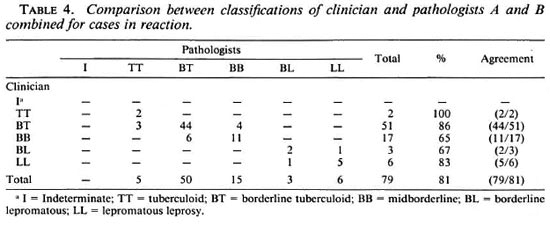
Diagnosis of classification for cases with reactions. Since the proportion of cases reported as having reactions was low, the concordance between the clinical and histopathologic diagnoses of classification and reactions was studied, taking the pooled samples of pathologists A and B. Concordance between the clinical and histopathologic diagnoses of the classification of 79 cases reported to be "in reaction" by the clinician is given in Table 4. A high level of concordance was observed for LL and BT cases. For the TT and BL types, since very few cases were available, the results may not be meaningful. A fairly good concordance was found for borderline reaction cases; overall agreement was observed in 81% of the cases.
DISCUSSION
A total of 1272 patients was analyzed to assess the degree of correlation between clinical and histopathologic classifications of leprosy. The patients were graded clinically by at least one of the physicians of the Institute and histopathologically classified by two pathologists. Although the overall percentages of agreement are somewhat different, the pattern of correlation for the various types of classifications is the same for the two histopathologists as for the clinician's diagnosis. Although there was no formal blinding, the independent nature of the histopathologic diagnosis is reflected by the significant discordance in clinical and histopathologic diagnoses, especially in borderline cases. LL cases seem to present the least problem for classification. For BL cases, as compared with LL cases, the amount of agreement was low. A majority of the discordant cases was classified as LL by histopathology. At the other end of the leprosy spectrum, although fairly good concordance was observed for the BT type, a low degree of agreement was seen for TT cases, with a fairly good majority of discordant cases being classified as BT by histopathology. For both pathologists, minimal agreement was seen in the I and BB cases.
Our study shows that there are problems of discordance in the clinical and histopathologic diagnoses of some types of leprosy (TT, BB and I). Since the same types of trends were observed among different pathologists and clinicians, the observed disparity does not appear to be because of the subjective nature of the observations, either clinical or histopathologic. This suggests that the criteria of giving weight to certain clinical signs versus clinical types or histologic parameters versus clinical types or considering any of these as a "Gold Standard" may not be ideal.
A sizable proportion of leprosy cases is in a continuously changing immunological spectrum, i.e., BT-BB-BL. In some early cases, clinical signs and symptoms may precede the presently known characteristic tissue changes, or vice versa. If a biopsy is taken at an early stage, there is likely to be discordance between the clinical and histopathologic observations. Although these cases were reported as "untreated," the chances that some of these cases had taken treatment earlier cannot be ruled out. The results may be affected partially by the stage of treatment. It would be of interest to follow proven untreated borderline cases after chemotherapy.
Tuberculoid leprosy (TT) is only slightly different from BT leprosy, both clinically and histopathologically. Clinically, these cases present as well-defined lesion(s) with partial or complete loss of sensation with or without a thickened nerve and very few acidfast bacilli (AFB), if any. Histologically, both of these leprosy types have very well-defined granuloma with lymphocytic infiltration and very few AFB. Immunologically, both also are similar to a large extent and differ only in degree. Therefore, the line of demarcation between TT and BT often overlaps both clinically and histologically. Since many cases diagnosed as TT have histopathologic evidence of BT, the present criteria of differentiating them does not appear to be adequate. It is also possible that that proportion of cases belonging to the stable polar tuberculoid type may be much lower than thought earlier. Therapeutically, TT and BT cases arc treated similarly and so are LL and BL cases. Therefore, combining these two groups (TT, BT and LL, BL) does not affect the chemotherapy of the disease. BB cases present special problems and even combining these cases with BT or BL does not seem to reduce the discordance significantly. Whether they should continue to be considered along with lepromatous (BL, LL) cases, or some changes are necessary, cannot be predicted from our present study.
In the work published to date, the overall agreement figures reported a range from a low of 33% (9) to a high of 77% (2). It should be noted that the percentage of overall agreement observed in a particular situation, besides depending upon other factors, is a function of the proportion of cases of classification of each type of leprosy in the total sample. Since the percentage of cases of each type of leprosy is different in various reported studies (3,9,10), the comparisons made on the basis of overall percentage of concordance may not be valid. Although the overall agreement observed is also dependent upon the individual histopathologist and clinician, a better way of making such a comparison between various studies is to work out these percentages of agreement separately for each type of leprosy. For the purpose of comparison of overall percentages between studies, some standardized procedure should be adopted.
The indeterminate cases appear to be problematic due to the nonspecific histology of their lesions. Definitive indeterminate diagnosis presently depends upon the demonstration of nerve lesion(s) (6). Pathologist A could not find any evidence of leprosy in 38% of indeterminate cases; pathologist B could not demonstrate bacilli in 61% of these cases. As expected, the ultimate failure/usefulness of histopathology in suspected and indeterminate leprosy will depend upon several factors such as the nature and depth of the biopsy, the quality of the section, and the number of acid-fast-stained sections examined, etc. Since the Institute is a referral center, these aspects are usually kept in mind. Because this was not a formal prospective study, some possible influence of any of these factors cannot be ruled out. By employing fluorescence, biochemical and molecular markers/gene amplification techniques, it may be possible to characterize these cases in a better way in the future. It may also be important to study the interobserver variations in the clinical diagnoses in borderline and indeterminate leprosy versus the results of histopathologic and other markers.
In the reactional cases, the degree of concordance between the clinician and the histopathologist is, by and large, reasonable in the diagnosis of types. For TT and BT only a few cases were available. Since the polar variety of tuberculoid (TT) leprosy is believed to be immunologically stable, these cases could have been of a subpolar variety also. It is, however, a question of debate and subclassification since reactions in tuberculoid (TT) have been described by some authors (3). The observed disagreement, though in a small proportion of cases, calls for the reappraisal of criteria for identifying reactions histopathologically as well as clinically.
The study reported has a number of limitations. Due to the lack of absolute standards, it was not possible to measure the sensitivity or specificity of the diagnosis/ classification made by either the clinician or the histopathologist. The design of the present study did not permit us to work out inter-observer variations between the two pathologists and between any two clinicians. Also, due to limitations in the study design, Cohan's Kappa (1) could not be reported. The present data, being hospital generated, cannot be regarded as representative of the population of leprosy patients in general.
To conclude, in-depth studies are required to reassess the criteria, giving weight to different clinical signs and histopathologic parameters, in relation to the diagnosis of the different types of leprosy.
Acknowledgment. The authors are indebted to Dr. H. Srinivasan, Director, and Dr. V. M. Katoch, Assistant Director, Central JALMA Institute for Leprosy, Agra, for their valuable comments on a previous draft. The wordprocessing help provided by Mr. Arun Kumar Babar and the secretarial help of Mr. J. D. Kushwah are also acknowledged. The referees of the submitted manuscript are gratefully acknowledged for their useful comments.
REFERENCES
1. COHEN, J. A. A coefficient of agreement for nominal scales. Educ. Psycho. Measure. 20(1966)37-46.
2. FINE, P. E. M., JOB, C. K., MCDOUGALL, C. M., M EYERS, W. H. and PONNIGHAUS, J. M. Comparability among histopathologists in the diagnosis and classification of lesions suspected of leprosy in Malawi. Int. J. Lepr. 54(1986)614-625.
3. JERTH, V. P. and DESAI, S. R. Diversities in clinical and histopathologic classification of leprosy. Lepr. India 54(1982)130-134.
4. JOB, C. K. and DHARMENDRA. Histopathology of reacting skin in leprosy. In: Leprosy, Vol. 2. Dharmendra, ed. Bombay: Sawant & Company, 1985, pp. 823-827.
5. Jopling, W. H. Leprosy reactions (reactional states). In: Handbook of Leprosy. 3rd edn. Trowbridge, U.K.: Redwood Burn Limited, 1984, pp. 68-77.
6. Liu. T.-C, Yen, L.-Z., Ye, G.-Y. and DUNG, G.-J. Histology of indeterminate leprosy. Int. J. Lepr. 50(1982)172-176.
7. Meyers, W. H., Heggic, C. D., Kay, T. L., Staple, E. M. and KVERNES, S. The Ridley-Jopling five group classification of leprosy-correlation of parameters of classification in 1429 leprosy patients. Int. J. Lepr. 47(1979)683-684.
8. Ridley, D. S. and JOPLING, W. H. Classification of leprosy according to immunity; a five-group system. Int. J. Lepr. 34(1966)255-273.
9. SEHGAL, V. N.,REGE, V. L. and REY, M. Correlation between clinical and histopathologic classification in leprosy. Int. J. Lepr. 40(1977)278-280.
10. SINGH, K., IYENGAR, B. and SINGH, R. Variations in clinical and histopathologic classification of leprosy: a report and possible explanation. Lepr. India 52(1983)472-479.
1. M. Stat., Assistant Director; Central JALMA Institute for Leprosy, Taj Ganj, Agra 282001, India.
2. M.D., Assistant Director; Central JALMA Institute for Leprosy, Taj Ganj, Agra 282001, India.
3. Ph.D., Ex-Research Officer; Central JALMA Institute for Leprosy, Taj Ganj, Agra 282001, India.
4. M.D., Ex-Deputy Director; Central JALMA Institute for Leprosy, Taj Ganj, Agra 282001, India.
5. M.D., Deputy Director; Central JALMA Institute for Leprosy, Taj Ganj, Agra 282001, India.
6. M.D., Research Officer, Central JALMA Institute for Leprosy, Taj Ganj, Agra 282001, India.
Dr. Mukherjee's present address is Institute of Pathology (ICMR), Ansari Nagar, New Delhi 110029, India.
Dr. Lavania's present address is Railway Hospital, Sholapur, Maharashtra, India.
Received for publication on 2 January 1992.
Accepted for publication in revised form on 15 April 1993.