- Volume 61 , Number 2
- Page: 298–325
II Würzburg symposium on the chemotherapy of leprosy
Organized by the
German Leprosy Relief Association
in cooperation with the
Institute for Experimental Biology and Medicine,
Borstel, Germany
16-18 September 1992
OPENING ADDRESS
Ladies and Gentlemen,
On behalf of the Board of the German Leprosy Relief Association (GLRA), it is a great pleasure for me to welcome you in Würzburg for the II Würzburg Symposium on Chemotherapy in Leprosy.
With this Symposium GLRA resumes a tradition which dates back to the two colloquia held at the Borstel Institute in the early 1970s followed by the first Symposium on Multidrug Therapy in Leprosy in 1986 in Würzburg.
Another reason for selecting this date is the fact that GLRA and the Institute for Experimental Biology and Medicine at Borstel look back on 20 years of close and fruitful cooperation. This cooperation between a relief association and a research institute may well be considered unique.
GLRA had realized at a very early stage that better and more effective drugs are necessary to fight leprosy effectively. In the person of Professor Dr. Enno Freerksen, who was the director of the Borstel Institute at that time, GLRA found a dedicated and interested scientist who was prepared to undertake efforts to achieve this goal with GLRA's support. The result of this joint venture, the development of a multidrug therapy (MDT) against leprosy with full right, may subsequently be called a pioneer deed. However, it took some time before this achievement was officially recognized. Today treatment of leprosy without MDT is hardly conceivable.
Under the motto "help for leprosy patients by leprosy research" GLRA made it its business to support research activities in the fields of chemotherapy, immunology and cultivation of the leprosy bacillus. At the same time, however, GLRA always was and is interested in convening scientists and therapists in order to help them develop a better understanding of each other. With the background of up-to-date research work it is, therefore, the declared objective of this Symposium to provide a problem-oriented and discussion-seeking forum.
We wish to express our sincere thanks to all of the scientists who have accepted our invitation and who agreed to make contributions toward this Symposium within the next 3 days.
We are also very grateful to the pharmaceutical companies "action medeor," CIBA GEIGY, FATOL-Arzneimittel and SANAVITA for their generous financial support. Please observe their information booths in the lobby.
Last but not least I wish you all, scientists and doctors from the field, fruitful discussions motivated by mutual understanding.
If the time permits, you should not fail to go for a stroll through our beautiful city which will surprise you with many historical sights and romantic places. Not to forget, of course, that famous people like Wilhelm Conrad Röntgen, Robert Koch and Werner Heisenberg once taught and worked at the time-honored Würzburg University.
Dr. Helmut Müller, President
German Leprosy Relief Association
Würzburg, September 1992
INTRODUCTION
In 1986, the German Leprosy Relief Association (GLRA) organized a "Symposium on Multidrug Therapy in Leprosy," the purpose of which was to exchange and discuss recent results in leprosy research and to establish communication between the scientist and the therapist.
The II Würzburg Symposium on Chemotherapy in Leprosy is meant to be a research-based, problem-oriented and discussion-seeking forum.
The decision to hold another Symposium in Wûrzburg between the American Leprosy Mission's (ALM) Concensus Development Conference held in the spring and the XIV International Leprosy Association Congress to take place next year deserves some explanation. The date was selected as especially appropriate to demonstrate and acknowledge our deep appreciation for the close cooperation with the Institute for Experimental Biology and Medicine at Borstel, which has been very fruitful over the past 20 years. At the same time, a number of doctors from the field will be in Würzburg and will participate in a meeting of our overseas representatives to be held subsequent to this Symposium. Our special interest is to inform and motivate these doctors to help them accomplish their work in the field.
Unlike the ALM Concensus Development Conference, which presented a very wide spectrum of patient treatment, and in contrast to the ILA Congress, which will deal with the overall problems of leprosy, the II Würzburg Symposium will concentrate on the chemotherapy in leprosy with special emphasis on basic research and its conclusions. This has already been an established tradition dating back to the two colloquia at Borstel held in the 1970s and resumed by the first Würzburg Symposium on Multidrug Therapy in Leprosy in 1986.
Believing in the driving force of competing opinions, we hope to promote promising alternatives within the scope of this Symposium and to create a forum for discussion for as many competent scientists as possible with the aim of encouraging mutual stimulation, criticism and cooperation.
Together with the Borstel Institute a program was worked out which includes the following topics:
I. The Malta Experience
The Leprosy Unit of WHO has been invited and has been requested to give a statement about the significance of the Malta Project.
II. Efficacy and Side Effects of Isoprodian-RMP
Session II will discuss information which exists about the efficacy and the side effects of Isoprodian-rifampin (RMP) in the treatment of leprosy and tuberculosis.
III. Methods in Drug Screening and/or Therapeutical Monitoring
The presentation of the different methods for screening antileprosy drugs and in monitoring the efficacy of treatment by the investigators who developed these techniques shall demonstrate the necessity of discussing a comparative assessment of these methods.
At the end of this session a Round Table Discussion about problems with current regimens is planned which will deal with the following suggested points: discussion of WHO-MDT; critical evaluation of drug screening and monitoring techniques; organization of new trials; and recommendations for the field. Contributions of not more than 5 minutes' duration may be prepared.
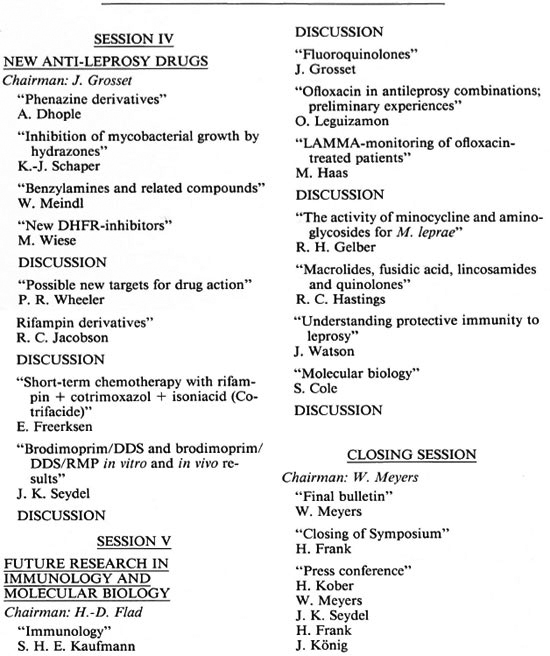
IV. New Antileprosy Drugs
An overview shall be given of the different new drugs or combinations of known drugs and their stage of laboratory testing or clinical trial.
V. Future Research in Immunology and Molecular Biology
Future research in fields other than chemotherapy will be presented as a special service to the audience.
The lecturers who have been invited to make contributions toward the different topics of the Symposium are listed on pages 321-323.
The audience will mainly consist of approximately 20 doctors from the field who are either working for GLRA or who are government officials responsible for national leprosy control programs.
Dr. Horst Frank
Medical Advisor-GLRA Board
Dr. Jiirgen Konig
Medical Director GLRA
Würzburg, June 1992
SCIENTIFIC PROGRAM
Wednesday, 16 September 1992
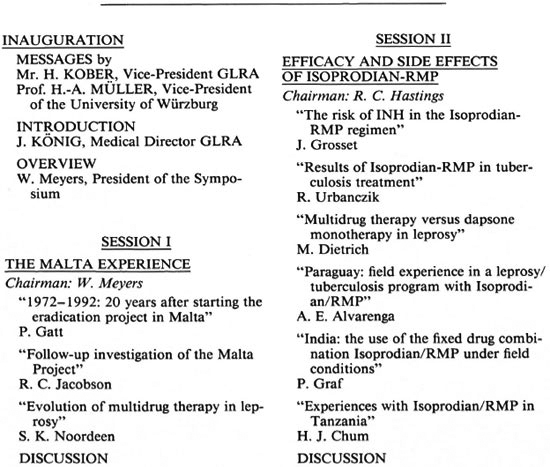
Thursday, 17 September 1992
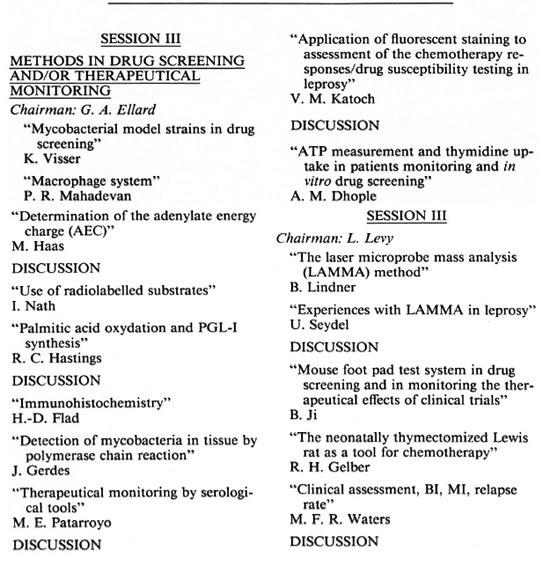
ROUND TABLE DISCUSSION PROBLEMS IN CURRENT REGIMENS
Chairman: J. K. Seydel
Friday, 18 September 1992
ABSTRACTS
Session I
THE MALTA EXPERIENCE
Chairman: Wayne M. Meyers
Gatt, P. 1972-1992: 20 years after starting the eradication project in Malta.
Since the Malta Leprosy Eradication Program was inaugurated in June 1972, 257 patients have been treated with Isoprodian-rifampin. The duration of treatment was not fixed, but was determined for each patient by the individual patient's clinical and bacteriological responses. The mean duration of treatment was 23 months, and the medication was safe and well tolerated. The small size of the island facilitated post-treatment surveillance in a large number of patients who completed MDT: the mean period of observation has been 12.26 years (S.D. 5.3) with a range of 0-19 years and more than half the patients still attend regularly for follow up. To date only one patient has re lapsed, 17 years after completion of MDT, and the last case of leprosy was notified in 1989.-51/1 College Street, Rabat, Malta.
Session II
EFFICACY AND SIDE EFFECTS OF ISOPRODIAN-RMP
Chairman: Robert C. Hastings
Grosset, J. The risk of isoniazid in the Isoprodian-rifampin regimen.
In order to assess the potential additive liver toxicity of isoniazid to that of antileprosy drugs, we conducted for 24 weeks a prospective double-blind trial involving 772 adult patients in four leprosy centers, two in India, one in Madagascar, one in Ivory Coast. Patients were given the following three drugs, daily 100 mg dapsone (DDS) and 350 mg prothionamide (PTH) plus monthly 600 mg rifampin (RMP), in combination with either 350 mg isoniazid (INH) or a placebo. After detailed clinical and laboratory examination on admission, the side effects and especially liver toxicity were assessed at regular intervals during treatment by laboratory testing (aminotransferases, bilirubin, alkaline phosphatase, HBs-Ag) and recording of spontaneous complaints. An analysis of the frequency and seriousness of side effects was made before breaking the code (with or without INH). No significant difference in the occurrence or not of mild or serious side effects was observed between patients treated with or without INH. Most (75%) of the observed side effects occurred during the first 4 weeks of treatment, and their onset was not related to INH. On the other hand, body weight and age were factors related to frequency of side effects: the higher the body weight, the less the rate of side effects (p = 0.03); the rate of serious side effects increased with age (p = 0.02).-Service Bactériologie, Faculté de Médecine Pitié-Salpêtrière, 91 Blvd. de l'Hôpital, 75634 Paris 13, France.
Urbanczik, R. Results of Isoprodian-rifampin in tuberculosis treatment.
Isoprodian (IPD), usually with rifampin (RMP), was/is being used for tuberculosis (TB) chemotherapy in at least 35 countries worldwide; most experiences come from Germany, Austria, Tanzania, Republic of South Africa (RSA), Paraguay and India. IPD-RMP contains at least 3 potent anti- Mycobacterium tuberculosis drugs; thus high sputum conversion and low relapse rates are not surprising: e.g., in 1.189 M + pulmonary TB cases in Paraguay (V. Pereira, in preparation) conversion rates (M+ to M-) achieved 86% after 2 months and 90% after 3 months, with a 2.2% relapse rate. Therefore side effects and other problems (e.g., compliance) seen in different places with IPD-RMP are discussed preferentially. In a RSA-controlled trial (H. H. Kleeberg, Chemotherapy 33 [1987] 219) among 114 persons 3 cases of hepatitis were seen. In Germany (Ch. Hoose, Pneumologie 44 [1990] 458) among 678 patients hepatotoxicity was observed in 7.4%. In Paraguay 1.3% of hepatitis was observed among 1486 patients receiving IPD-RMP. Such a low hepatotoxicity rate may be due to lower than conventional prothionamide (PTH) dosage in IPD (= 350 mg/day); this is possible due to increased PTH blood levels when PTH is given simultaneously with INH (H. Franz, et ai, Prax. Pneumol. 28 [1974] 605). However, other factors may be important: e.g., in China (Ji, et ai, Lepr. Rev. 55 [1984] 283) hepatotoxicity of RMP + PTH exceeded 20%. Also, roughly 5% to 30% of persons receiving IPD-RMP may experience gastrointestinal troubles (e.g., G. A. Ellard, et ai, Lepr. Rev. 59 [ 1988] 163), which may affect their compliance. In summary, IPD-RMP may be a more suitable (effect/ economy) alternative ofSM + INH + TSC, particularly (?) in regions with an high HIV + load. -Fatol Arzneimittel GmBH, D/W6685, Schiffweiler, Germany.
Dietrich, M., Gaus, W., Kern, P., Meyers, W. M. and Clinical Study Group. Multidrug therapy versus dapsone monotherapy in leprosy: an international randomized study with long-term follow up.
Dapsone monotherapy in leprosy was replaced by the WHO multidrug treatment (MTD) concept 10 years ago. We performed a multicenter, prospective randomized treatment study on leprosy starting in 1979. Dapsone was compared with two different drug combination regimens in patients with either lepromatous (A) or borderline (B) leprosy from different centers in India and Sierra Leone. A 3-year treatment phase was followed by a 5-year observation phase without treatment. In the final analysis 233 patients were included. Randomization and stratification with two clinical diagnoses (L and B) revealed a close comparability of groups. Histopathology as the primary outcome variable was determined objectively and independent from the clinical observations and the treatment group. Mouse foot pad tests were performed at entry; 13 patients were regarded as dapsone resistant and treated further with drug combination regimen. In all treatment groups there was a parallel decrease of the mycobacterial load except a single nonresponder in the dapsone group (mouse foot pad test was sensitive). Two relapses observed in patients who did not adhere to the protocol of treatment and follow up.
Dapsone monotherapy has the same frequency of cure as the combinations of dapsone and rifampin or rifampin and isoprodian. The statistical test was not significant, indicating that the differences in therapeutic success between the three treatment groups can be due to pure chance. Further, a power calculation showed that only a rather small difference between dapsone monotherapy and the used MDT schemes could have been overlooked by the study. Thus, we provide evidence that dapsone monotherapy is an effective and safe treatment for leprosy. This is in contradiction to the general opinion but indicates that carefully designed clinical studies are needed to determine the superiority of MTD treatment regimens. -Bernhard Nocht Institute for Tropical Medicine, Bernhard-Nocht-Str. 74, 2000 Hamburg 36, Germany.
Alvarenga, A. E. Field experience in leprosy/tuberculosis program with Isoprodian-rifampin.
After 11 years of experience with Isoprodian-rifampin (RMP) in the field of leprosy and tuberculosis treatment, our achievements are as follows. In the leprosy program, 4898 patients were treated with multidrug therapy (MDT) since October 1979 in Paraguay. To date, 3116 cases have completed their treatment. After 5 years of posttreatment control, 1478 cases are cured. Relapses were detected in 11 cases (0.74%), the cause of which was not possible to determine. The prevalence rate decreased from 1.7 per thousand inhabitants in 1979 to 0.38% in 1971. Several orders of side effects, that caused a change of the therapeutic regimen, were detected in 57 cases (1.16%). From 1979 until 1991, 14,709 tuberculosis patients received Isoprodian-RMP. In cohort analysis performed since 1987 to 1991, out of 3779 patients, 2930 (77.5%) were cured on average. Among 11,766 patients, treated since 1983 to 1991, 212 (1.8%) relapsed. Therapy was changed in 99 cases (1.6%) out of 6002 cases treated between 1988 and 1991 because of drug intolerance and other reasons. Treatment was abandoned by 2543 (17.3%) cases out of 14,709 treated during 1979-1991. Among 14,709 patients treated during 1979-1991, 555 (3.8%) died. -Ministerio de Salud Publica y B.S., Departamento de Lepra, Casilla de Correo 3054, Asuncion, Paraguay.
Graf, P. India-the use of the fixed drug combination Isoprodian-rifampin under field conditions.
Aim of the study: To test the practical application of the fixed drug combination under field conditions focusing on: feasibility, complications (reactions and side effects), and efficacy.
Methods and material: 250 leprosy patients (MB and PB) from eight Indian leprosy centers were checked at regular intervals for clinical activity, bacterial index and complications.
Results: a) The specific problems of a multicenter study were highlighted, b) The feasibility of using a fixed drug combination under field conditions was proven and the efficacy of the treatment was shown, c) A thorough investigation of side effects showed a considerable number of minor side effects; major side effects were few.-Tanzania Leprosy Association, P.O. Box 5478, Dar-es-Salaam, Tanzania.
Chum, J. H. Experiences with Isoprodianrifampin in Tanzania.
Tanzania has had over 10 years' experience with Isoprodian-rifampin (RMP). More than 20,000 patients have used the drugs in our routine program conditions. Compliance in both PB and MB patients has been good, especially in the former group (PB) as shown by our cohort reporting. While minor side effects (like nausea and abdominal discomfort) are sometimes encountered, major side effects (like liver toxicity) occur but rarely. The paper highlights cure rates and compliance as shown by our cohort reports of the last 3 years. Figures and graphs on various observations with the drugs are presented. -Ministry of Health, P.O. Box 9083, Dar-es-Salaam, Tanzania.
Session III
METHODS IN DRUG SCREENING AND/OR THERAPEUTICAL MONITORING
Chairman: Gordon A. Ellard
Visser, K. and Seydel, J. K. Mycobacterial model strains in drug screening.
During the preclinical development of new drugs in chemotherapeutic research, in vitro test systems are used for the screening of a great number of compounds because they are fast and reproducible methods to show the direct interaction between the drug and the microorganism without the influence of pharmacokinetic processes. The lack of an in vitro test system for Mycobacterium leprae therefore leads to difficulties in the development of new antileprosy drugs or drug combinations. To overcome these disadvantages model strains of other mycobacteria have been used as substitutes for M. leprae, such as M. "lufu," M. marinum, M. avium, M. kansasii, M. tuberculosis and others, under the assumption that the modes of action of old and new drugs on M. leprae and these model strains are identical. One of the main features of a model strain should be the same or a similar pattern of sensitivity as has been found for M. leprae against already known antileprosy drugs. The model strains have been used not only for the in vitro testing of new drugs or drug combinations showing synergistic or antagonistic behavior, but also as sources of target enzymes, for human serum activity tests and as causative organisms in animal infection models. -Med. Pharm. Chem., For- schungsinstitut, 2061 Borstel, Germany.
Mahadevan, P. R. Macrophage system.
Membrane surface alteration leading to reduction in the number of Fc receptor bearing macrophages, in the presence of live Mycobacterium leprae, has been one of the in vitro methods that has been used successfully. The method has been helpful to determine the viability of any M. leprae sample from patients under therapy or screen unknown compounds for antibacterial ability using isolated M. leprae. This method is well correlated with the mouse foot pad (mfp) as well as the ATP assay systems. The Fc receptor assay system, as well as fluorescence staining with FDA, has helped to identify drug-resistant bacilli from relapsed patients. Such patients have been under treatment with dapsone, rifampin, and ofloxacin in combination. New drugs developed for leprosy also have been screened by the Fc receptor assay and later confirmed by the mfp method. Such identified compounds include brodimoprim, K130 and KS10. These specific examples are presented.-Foundation for Medical Research, 84A R. G. Thadani Marg, Worli, Bombay 400018, India.
Katoch, V. M. Application of fluorescent staining to assessment of the chemotherapy responses/drug susceptibility testing in leprosy.
During the last decade, fluorescent diacetate-ethidium bromide (FDA-EB) staining has been used in different laboratories all over the world for determining the viability of mycobacteria including Mycobacterium leprae. The technique has been used on smears, bacillary suspensions and has been applied to monitor the chemotherapy responses as well as in the drug screening. At JALMA, Agra, FDA-EB staining has been tried and compared with morphological index (MI), ATP measurements, gene probe hybridization/gene amplification techniques as well as conventional parameters of viability. Our experience, as well as an overview of other published data, shows that FDA-EB staining is an easy and rapid method for measuring the trends of chemotherapy responses as well as drug susceptibility testing. However, the persistence of greenstaining character for some time after death, intermediary stained forms, subjectivity, requirement of a fluorescent microscope, and lack of applicability to paucibacillary cases (including relapses/reactions) are important limitations. Such limitations are comparatively much less with bioluminescent/molecular gene probe and gene amplification techniques.-Central JALMA Institute for Leprosy, Taj Ganj, Agra 282001, India.
Dhople, A. ATP measurment and thymidine uptake in patient monitoring and in in vitro drug screening.
Mycobacterium leprae has not yet been grown in vitro in the true sense. Thus, until recently the only method available to determine the viability of M. leprae has been mouse foot pad inoculations. However, it has not been practical to adopt this method either to monitor the progress of patients or for screening potential antileprosy compounds. The ubiquitous distribution and metabolic importance of ATP make precise, quantitative measurement of ATP a promising chemical method for quantitating microorganisms. The method of measuring ATP is based on bioluminescent reaction of luciferase and ATP. The technique is simple, inexpensive, rapid and sensitive enough to be used with M. leprae usually obtained from standard biopsies. Because ATP per cell can distinguish between deteriorating populations and those capable of genuine growth, this technique can be applied for screening potential antileprosy compounds using axenic media. Suspensions of M. leprae are able to take up 3H-fhymidine, an important precursor in DNA synthesis. Thus, it has been adopted to measure viability of M. leprae in axenic media. Because of the limitations in M. leprae required, this method can only be used in screening potential antileprosy compounds. Results obtained from both methods agree well with foot pad data for both drug screening and patient monitoring. -Florida Institute of Technology, Department of Biological Sciences, Melbourne, FL 32901, U.S.A.
Haas, M. Determination of the adenylate energy charge (AEC).
The adenylate energy charge (AEC) defines the proportion of energy-rich adenine nucleotides referred to the total amount of adenine nucleotides. The ratio is given by the equation AEC = ( ½ ATP + ADP)/(ATP + ADP + AMP). The determination of the AEC is (in contrast to the determination of the ATP content) independent from the number of bacterial organisms and well reproducible as shown in a variety of publications for different bacterial genera and also for eucaryotic cells. For mycobacterial species (cultivable as well as noncultivable) only few data have been published in literature so far. We discuss the technical details of the method with particular emphasis on the noncultivable species Mycobacterium leprae. Furthermore, present AEC data determined for different untreated and drugtreated mycobacterial species, including M. leprae isolated from armadillo tissue, are presented to demonstrate the applicability of the method for the determination of drug effects and with that for drug screening. Implications of the method for in vivo therapy control are discussed. -Division of Biophysics, Institute for Experimental Biology and Medicine, 2061 Borstel, Germany.
Nath, I. Use of radiolabeled substrates.
Our laboratory has developed a rapid in vitro radiometric assay for the evaluation of the viability and drug sensitivity of Mycobacterium leprae using 3H-thymidine, 3H-adenosine and other labeled purines. Bacilli from skin biopsies of leprosy patients have been maintained in human/murine macrophages and pulsed with the radiolabeled substrates. Over a 10-15-day period the cultures with freshly extracted M. leprae show a significant (p < 0.05 to <0.001) incorporation of the radiolabel as compared to the control with the equivalent heat-killed bacilli. This assay has been found to compare favorably with the mouse foot pad method. Over 700 leprosy patients have been screened for drug resistance and effectivity of multidrug therapy at the hospital and field levels. Radiolabeled compounds aimed at assessing essential metabolic steps or at DNA synthesis of M. leprae appear to be useful as markers of viability, drug resistance and screening of newer drugs. Their advantage is in the rapidity of diagnosis and easier quantification of the end results. Although these techniques appear to be high tech, they can be easily fitted into regional laboratories with rapidly trainable technicians. This proves more effective than the mouse foot pad assay which needs long-term maintenance of animals in air-conditioned rooms. -Department of Biotechnology, All India Institute of Medical Sciences, New Delhi 110029, India.
Franzblau, S. G., Harris, E. B. and Hastings, R. C. Palmitic acid oxidation and PGL-I synthesis.
Over the past few years we have developed several in vitro methods to follow the metabolic integrity of Mycobacterium leprae harvested fresh in a highly viable condition from the foot pads of infected nude mice. Initial work with ATP was replaced with the Buddemeyer system in which radiolabeled palmitate is catabolized by the organism to CO2. Biophysical parameters such as pH, temperature, pO2, and pCO2 were optimized and adapted to the in vitro synthesis of PGL-I by measuring rates of incorporation of radiolabeled palmitate, and finally to the commercially available BAC-TEC 460 system. The systems were verified internally by viability determinations in mice, by comparison to each other, and by comparison to PCR results. The BACTEC and Buddemeyer systems were verified in a double-blind trial of unknown drug solutions in an external trial sponsored by the World Health Organization. For many purposes, particularly drug screening, these in vitro metabolic activities of M. leprae can act as a surrogate for viability determinations in mice. -Laboratory Research Branch, GWL Hansen's Disease Center at Louisiana State University, P.O. Box 25072, Baton Rouge, LA 70894.
Flad, H.-D., Richter, E., Arnoldi, J., von Ballestrem, W. G., Alvarenga, A. E. and Gerdes, J. Immunohistochemistry.
Immunohistochemical investigations have demonstrated clearly that lesions of tuberculoid leprosy are characterized by the presence of CD4* T lymphocytes and cells producing the cytokines IL-1β, TNF-α, and IFN-γ; whereas in lepromatous leprosy lesions the latter cells are usually lacking or very rare. Moreover, preliminary data have suggested that the cytokine pattern in skin lesions from LL patients under chemotherapy changes to a pattern in which more cytokine-producing cells are detectable in patients under chemotherapy (Flad, et al., Trop. Med. Parasitol. 41 [1990] 307-309; Arnoldi, et al, Am. J. Pathol. 137 [1990] 749-753). In a recent therapy trial with dapsone, prodioprim and rifampin, patients were monitored by follow-up biopsies. Cellular infiltrates were determined, and mycobacterial DNA was assessed by polymerase chain reaction (see abstract Gerdes, et al., this conference). The data so far indicate that in patients in whom mycobacterial DNA is found to be reduced during therapy, there is a clear tendency of an increase of subepidermal Langerhans' cells, an increase of infiltrating interferon-γ-producing cells, and a decrease in γ/δ T cells. Collectively, these data suggest that cytokine patterns, characterization of cellular infiltrates, and assessment of mycobacterial DNA can help in establishing criteria for the duration of therapy in patients with various forms of leprosy.-Department of Immunology and Cell Biology, Forschungsinstitut Borstel, Parkallee 22, D-2061 Borstel, Germany.
Gerdes, J., Richter, E., Hahn, M., von Ballestrem, W. G., Alvarenga, A. and Flad, H.-D. Detection of mycobacteria in tissue by polymerase chain reaction.
Conventional histopathological diagnosis of mycobacterial infections is limited to the detection of acid-fast bacilli. A species-specific diagnosis was impossible until we recently introduced in situ hybridization and polymerase chain reaction (PCR) for this purpose (Arnoldi, et al., Lab. Invest. 66 [1992] 618-623) using Mycobacterium leprae as the model organism. For specific amplification of M. leprae DNA by PCR, primers were employed which comprise DNA sequences coding for species-specific 16S rRNA. Species specificity of the PCR products was confirmed by a) the application of three primers per PCR assay, resulting in a genus-specific and a species-specific PCR product, and b) by direct sequencing of the PCR amplificates. These techniques were applied to follow-up skin biopsies enrolled in a multidrug treatment study. We could assess the presence and the relative amount of M. leprae DNA in the biopsies under the different treatment conditions. In 75% of the cases investigated thus far, a clear cut decrease of M. leprae -specific PCR products could be demonstrated in the follow-up biopsies of lepromatous leprosy patients under multidrug therapy. The correlation of the latter findings with immunological parameters (see abstract Flad, et al .) are detailed. We assume that PCR techniques in conjunction with immunohistochemistry may be powerful tools for therapy monitoring of leprosy. -Department of Immunology and Cell Biology, Forschungsinstitut Borstel, Parkallee 22, D-2061 Borstel, Germany.
Patarroyo, M. E. Therapeutical monitoring by serological tools.
Leprosy remains an important health concern for developing countries, mainly due not to its mortality rate but to the social consequences suffered by the diseased. Although the Hansen bacillus was discovered over a century ago, there still remain problems associated with its diagnosis, classification, and therapeutical monitoring. One of the main tools proposed to solve these problems is the use of synthetic peptides as antigens in ELISA-based tests with the aim of detecting circulating antibodies against Mycobacterium leprae native proteins. During the last decade our laboratory has purified several M. leprae proteins from human-derived lepromas. We have synthesized 15-30 residue peptides from the N-terminal amino acid sequences of these proteins, and they have been tested with untreated patients corresponding to all the spectrum of leprosy, as well as with healthy household contacts, active tuberculosis patients, and normal donors. Our results show a good correlation between leprosy infection and reactivity to the synthetic peptides. Likewise, there is a low recognition of these peptides by normal donors, active tuberculosis patients, and healthy household contacts.-Instituto de Inmunologia, Hospital San Juan de Dios, Carrera 10 Calle 1, Bogota, Colombia.
Lindner, B. The laser microprobe mass analysis (LAMMA) method.
In the LAMMA-instrument a high-power pulse laser is focused through the objective of a light microscope onto the sample with a lateral resolution of approximately 1 µm. The laser irradiation leads to the evaporation and partial ionization of a small sample volume and the produced ions are registered in a time-of-flight mass spectrometer. The high lateral resolution in combination with the high sensitivity (approximately 0.01 ppm for sodium) of the instrument allows the analysis of individual bacterial organisms. The mass spectra of bacteria contain information on intrabacterial concentrations of elemental ions, e.g., Na+, K+ and on the organic cell matrix. The latter is hidden in complex patterns of organic fragment ions which were shown to be typical for a given bacterial population and, thus, can serve as mass fingerprints. Bacterial impairment is reflected in changes in the ratio of the intrabacterial concentrations of Na+ and K+ (Na+, K+-ratio) and of the fingerprint patterns. Thus, from the evaluation of these parameters for a limited number of individual organisms from samples taken during treatment, statements on drug-induced impairments can be derived. -Forschungsinstitut Borstel, Parkallee 10, D-2061 Borstel, Germany.
Seydel, U. Experiences with LAMMA in leprosy.
Laser microprobe mass analysis (LAMMA) of a limited number of individual Mycobacterium leprae organisms allows the determination of the physiological state (viability) of a bacterial population and its changes upon the influence of drugs from the measurements of the intrabacterial Na+ , +-ratios and the evaluation of the mass fingerprint spectra. The method can be applied to the in vivo therapy control and to in vitro drug screening. In the first application, M. leprae are isolated for mass analysis from patients' skin biopsies taken at different times during treatment. In principle, the results can be obtained only a few days after arrival of the biopsy specimens.
Limitations of the method arise from the fact that not every biopsy contains sufficient numbers of bacteria and from difficulties in connection with the isolation procedure. For in vitro drug screening, armadillo-derived M. leprae are kept in culture medium up to 4 weeks, exposed to a drug at different concentrations or for different times, and samples arc prepared for LAMMA. Since M. leprae do not multiply under these conditions, only the action of such drugs which do not interfere with replication or cell division can be monitored this way. A quantification of the LAMMA data in terms of percent viables is achieved by the determination of a limiting value of the Na+ , K+-ratio for viability. Examples for both applications are presented. -Forschungsin- stitut Borstel, Parkallee 10, D-2061 Borstel, Germany.
Ji, B.-H. Mouse foot pad system in drug screening and in monitoring the therapeutic effects of clinical trials.
The mouse foot pad technique is by far the universally accepted system for screening new drugs with antileprosy activity. All of the effective antileprosy drugs have been demonstrated to exert at least bacteriostatic activity in the system; whereas no compound shown to be inactive in mice displays definite effects in leprosy patients. The system is time consuming, requires many mice and gram amounts of the compounds to be tested, and therefore can be employed to investigate only limited numbers of compounds that represent a very few selected classes. However, the anti-Mycobacterium leprae activity of any new compound identified by in vitro method must be established firmly in the foot pad system prior to the initiation of a clinical trial. Serial mouse foot pad inoculations with M. leprae recovered from skin biopsies have been applied as one of the most efficient techniques in monitoring the therapeutic effects of new drugs or combined regimens in clinical trials. It needs only a small number of multibacillary patients, and allows one to measure the initial killing of 2 or 3 logs of M. leprae with immunocompetent mice and 4 or even 5 logs with nude mice. However, the technique is not sensitive enough to measure precisely the bactericidal effects of rifampin (RMP) administered more than a few doses and, therefore, is unable to compare various RMP-containing regimens or any regimen containing more than one powerful bactericidal drug. Mouse foot pad inoculation is also the most reliable technique to confirm the diagnosis of bactériologie relapse, one of the most important parameters in monitoring the long-term therapeutic effect in MB leprosy. -Bactériologie et Virologie, Faculté de Médecine Pitié-Salpêtrière, 91 Blvd. de l'Hôpital, 75634 Paris 13, France.
Gelber, R. H. The neonatally fhymectomized Lewis rat as a tool for chemotherapy research.
We have found that detection of viable Mycobacterium leprae from the skin of lepromatous leprosy patients by the neonatally thymectomized Lewis rat (NTLR) is a more sensitive monitor of M. leprae viability in short-course chemotherapy with rifampincontaining regimens than the normal mouse. We found 3 days to 1 month after the initiation of two rifampin-containing regimens that, while only 1 of 66 skin specimens grew M. leprae in normal mice, 33 of 66 grew directly in NTLR or on subpassage to BALB/c mice or other NTLR.
We have also utilized the NTLR model to simulate chemotherapy of the "persister" state. In these studies, we infected NTLR in the hindfoot pads with 5000 M. leprae, and 1 year later, when the number of M. leprae per foot pad was > 107, these NTLR were treated with various regimens for 4 months; 2 or more months after discontinuing therapy, treated NTLR foot pads were harvested so as to assess the presence of any surviving "persisters" by subpassage to both NTLR and BALB/c mice. We found several regimens that do not regularly eliminate "persisters" in this model: rifampin alone, two schedules of rifampin plus dapsone, dapsone plus ethionamide, minocycline alone, and rifampin pius clofazimine. On the other hand, "persisters" can be eliminated in this model by rifampin plus minocycline, rifampin plus ofloxacin, and rifampin plus ethionamide. -Medical Research Institute at California Pacific Medical Center, 2200 Webster Street, San Francisco, CA 94115-1896, U.S.A.
Waters, M. F. R. Clinical assessment, BI, MI, relapse rate.
Controlled clinical trials require the concurrent admission and random distribution of patients to all treatment groups, and must include a control group receiving standard therapy for a standard duration. Clinical assessments should, as far as possible, be performed "blind," although treatment methods (e.g., surgery in neuritis) or drug side effects (e.g., clofazimine discoloration or thalidomide sleepiness) may be unavoidably obvious. The timing and nature of assessments should normally be the same for each group.
The rate of fall of the bacterial index (BI) (related to classification) is important in assessing the long-term response to chemotherapy, and also the effect of cytokine or other immunotherapy. Smear sites should be well chosen, and quality control is essential. Although the morphological index (MI) is not standardized, it is of particular value in the early detection of relapse and for the selection of the biopsy site as a source of Mycobacterium leprae for mouse foot pad inoculation.
The long-term relapse rate is the essential assessment of "cure" by any chemotherapy regimen. Whereas confirmation of relapse in multibacillary leprosy is usually simple (but should include mouse foot pad inoculation), in paucibacillary leprosy it may be very difficult to distinguish from late reversal reaction, and possible methods arc discussed.-Hospital for Tropical Diseases, 4 St. Pancras Way, London NW1 OPE, U.K.
Session IV
NEW ANTILEPROSY DRUGS
Chairman: Jacques II. Grosset
Dhople, A. M. New antilcprosy drugs: phena/.ine derivatives.
Clofazimine, a deeply colored iminophenazine, was first introduced for treatment of leprosy in 1962. It binds externally to cytosine-guanine DNA base pairs in vitro. It is very effective against dapsone and rifampin-resistant strains of Mycobacterium leprae. However, this drug is poorly absorbed from the gastrointestinal tract and accumulates in the body fat, causing reddening and darkening of the skin. To alleviate this situation, a number of analogs recently have been synthesized. The efficacy of these compounds was evaluated in the in vitro system and also, in come cases, in the mouse foot pad system; results were compared with those obtained with clofazimine.
In the in vitro system, there was a definite structure-related activity among the compounds. Halogenation of p-anilino group in position 3, as well as in position 7, of the phenazine ring influenced the activity. Dichlorocompounds were more active than monochloro, and furthermore, bromination in these positions gave higher activity than chlorination. In position 2, replacing isopropyl group on iminonitrogen with both mono and dichloro compounds also gave higher activity. Among the compounds tested in the mouse foot pad system, similar structure-related activity was observed. Replacing clofazimine in the MDT regimens with some of these active compounds did not yield any better results. -Florida Institute of Technology, Department of Biological Sciences, Melbourne, FL 32901, U.S.A.
Schaper, K.-J., Seydel, J. K. and Dhople, A. M. Inhibition of mycobacterial growth by hydrazones.
Using thiacetazone (TAZ) as a starting point, our efforts at developing a new drug against leprosy resulted in the discovery of the antimycobacterial activity of heterocyclic hydrazones. The properties of these compounds suggest the enzyme ribonucleotide reductase (RR) to be the mycobacterial target whose inhibition indirectly stops the synthesis of DNA. The hydrazones show a synergistic potentiation of activity when combined with other inhibitors of mycobacterial multiplication as dapsone, rifampin or isoniazid. The synergism probably is caused by the simultaneous inhibition of several steps of the enzyme pathway leading to DNA synthesis. Since the pharmacokinetics and toxicology of the above-mentioned heterocyclic hydrazones have not yet been investigated, we returned to our starting point TAZ. Assuming also that this nonhetcrocyclic hydrazone is an inhibitor of reversal reaction, we indeed found a very remarkable synergism of antimycobacterial activities also in combinations of TAZ with dapsone, rifampin, isoniazid and ethambutol. These combinations enabled excellent results in the clinical treatment of patients with atypical tuberculosis ( M. avium infections, including AIDS). Recent investigations have shown synergism of the combination of TAZ + rifampin also against M. leprae in the mouse foot pad test. -For- schungsinstitut Borstel, Med.-Pharmazeut. Chemic, Parkallee 4a, D-2061 Borstel, Germany.
Meindl, W. Benzylamincs and related compounds.
N-Alkylbenzylamines are specifically active against mycobacteria. The most active compounds against Mycobacterium tuberculosis H37Ra also exhibit an inhibitory effect on atypical mycobacteria such as M. marinum, M avium and M. "Ittfu." Compound 93, N-methyl-3,5-dichloro-benzylamine-HCl, is also tested against M. leprae in vitro (Dhople's method) and in the mouse foot pad test. Since the development of resistance appears when compound 93 is given alone, the testing in combinations with anti leprosy drugs in vitro and in vivo are described: Strong synergisms can be seen in combinations either with dapsone or with rifampin. Compound 93 is well tolerated by all mice even at high doses. In a pharmacological screening system, the only side effects are antihistaminic activities and an antagonism of the slow-reacting substances of anaphylaxis. In order to reduce the doses that are needed for inhibiting growth of mycobacteria new compounds related to the benzylamines, such as 1-phenyl-1-alkylamino-alkanes and others, arc presented including the MIC-valucs against AI. tuberculosis, M. avium-intracellulare and M. leprae in vitro. The most active new drug inhibits growth of M. tuberculosis at a concentration of 0.125 µg/ml. - Institut fur Pharmazie, Universitat Regensburg, Universitatsstra. 31, 8400 Regensburg, Germany.
Wiese, M. New dihydrofolatc reductase inhibitors.
A new, highly active, dihydrofolate reductase inhibitor (K-130) has been developed for the treatment of leprosy. This was demonstrated on Mycobacterium "lufu" as a model strain as well as on M. leprae in vitro. The in vitro efficacy was convincingly confirmed in mouse foot pad experiments. On the basis of these results, toxicity studies in rats and monkeys were performed at the Central Drug Research Institute in Lucknow, India, showing that the drug is safe up to the highest concentrations tested. The data have been submitted to the Indian Drug Controller for permission to initiate phase I clinical trials. -Med.-Pharmaceutical Chemistry, Borstel Research Institute, D-2061 Borstel, Germany.
Wheeler, P. R. Possible new targets for drug action.
This paper considers the targets in envelope biosynthesis. Virtually nothing is known about biosynthesis of envelope components so it is difficult to know whether any of the presently available agents act on envelope biosynthesis. However, evidence that isoniazid and ethambutol act on mycolate synthesis and assembly, respectively, is reviewed. The mycobacterial envelope contains many characteristic structures. Thus, the enzymes for their biosynthesis arc potentially attractive as targets for selective agents. Particularly attractive targets for new agents are biosynthetic activities, which must make the following components unique to mycobacteria: the mycolylarabinogalactan-peptidoglycan linkage; the methyl terminus of the meromycolate moiety of mycolic acids themselves; mycoccrosic acids (the enzyme has been purified); glycolipids and pcptidoglycolipids. It is encouraging that the mycobacterial wall appears to be the permeability barrier to hydrophillic solutes, which may include potential antimycobacterial agents. Therefore any disruption of the cell-wall structure-even short of causing lysis of the bacterial organism-could increase its permeability to agents that do not get into mycobacteria.-London School of Hygiene and Tropical Medicine, Keppel Street, London WC1E 7HT, U.K.
Grosset, J. Fluoroquinolones.
Because fluoroquinolones inhibit bacterial DNA gyrascs and have powerful activities against gram-negative and also grampositive microorganisms, and favorable pharmacokinetic properties, their activities against Mycobacterium leprae have been tested in the mouse foot pad system. Daily 150 mg/kg ciprofloxacin was inactive; whereas daily 50 mg/kg pefloxacin showed bacteriostatic activity, and daily 150 mg/kg displayed bactericidal activity. Daily 50 mg/ kg ofloxacin was as active as daily 150 mg/ kg pefloxacin, and daily 150 mg/kg ofloxacin displayed bactericidal activity; although sparfloxacin was more active than ofloxacin on a weight-to-weight basis, its real advantage over ofloxacin in the treatment of experimental leprosy remains unclear. Patients with newly diagnosed lepromatous leprosy tolerated well up to 6 months of treatment with twice daily 400 mg or once daily 800 mg pefloxacin, and once daily 400 or 800 mg ofloxacin. Although a single dose of pefloxacin or ofloxacin only displayed a modest degree of bactericidal effect, about 99.99% of the organisms viable on day 0 were killed by 22 doses of either 800 mg pefloxacin or 400 mg ofloxacin. In conclusion, ofloxacin represents the first lead to an important new antileprosy drug in many years since the introduction of rifampin.-Service Bactériologie, Faculté de Médecine Pitié-Salpêtrière, 91 Blvd. de l'Hôpital, 75634 Paris 13, France.
Leguizamon, O. R. Ofloxacin in antilcprosy combinations; preliminary experiences.
Since preliminary studies had demonstrated considerable antimycobacterial activity of ofloxacin, it seemed necessary to utilize it to elaborate our own opinion about its activeness in leprosy with 9 and 1 LL and BL patients, respectively. In our standard therapy (Isoprodian-rifampin) we replaced prothionamide with ofloxacin. A relatively high dosage (500 mg/day) was chosen. During the treatment, 4 cases complained about diarrhea without colic, 2 cases complained of headache, gastric disturbance and vomiting in 1 of them. In this latter one we decided to reduce the dosage of the combination and, after a week, the patient, when again on the initial dosage showed good tolerance. In the remaining 4 cases, good tolerance was observed. The duration of the treatment was limited to 2 months, followed by a period of observation without treatment from 2 to 6 months. As a final result, the therapy was excellent in 2 cases, and in the remaining 8 cases the treatment was continued with our standard therapy.-Ministerio de Salud Publica, Depart mento de Lepra, Casilla de Correo 3054, Asuncion, Paraguay.
Haas, M. LAMMA monitoring of ofloxacin-treated patients.
In a clinical trial including 17 multibacillary leprosy patients, the in vivo effectiveness of ofloxacin (200 mg twice daily for 3 months) on Mycobacterium leprae was tested via mass spectromctric determination of the intrabacterial ratios of the concentrations of the sodium and potassium ions (Na+, K+-ratio) of individual bacteria isolated from skin biopsies. In parallel, mass spectra of the fragment ions originating from the organic cell matrix were registered and evaluated as mass fingerprints with statistical methods to provide additional information on drug-induced impairment. Both methods revealed that in five cases the bacteria did not respond to the therapy. They did not show any significant changes in the Na+, K+-ratio or in the mass fingerprint spectra relative to the untreated controls. In two cases, these findings were backed by ATP measurements. In the responder cases, the M. leprae were severely impaired. From the cation ratios the percentage of viable organisms averaged over all untreated biopsies was determined to be 58% on the basis of a limiting value of the Na+, K +ratio for a viability of 0.43. The percentage killing during the first 3 months of monotherapy was 72%. -Division of Biophysics, Institute for Experimental Biology and Medicine, D-2061 Borstel, Germany.
Gelber, R. H. Activity of minocycline and aminoglycosides for Mycobacterium leprae.
We found both in mice and in clinical trial that minocycline has great potential for the treatment of leprosy: In mice minocycline was consistently bactericidal (99.7% and 99.4%) for Mycobacterium leprae, regularly inhibited all isolates (15) tested at levels easily attained in man by standard dosages, was additive in activity for M. leprae when combined with other antimicrobials (dapsone, rifampin, and kanamycin), and was active administered intermittently (once weekly and at times once monthly). In our clinical trial of 100 mg minocycline administered once daily to eight lepromatous leprosy patients, clinical improvement was uniquely rapid, and by mouse foot pad inoculation no detectable viable M. leprae were found in the dermis of any patient after 3 months' therapy, a faster rate than for either dapsone or clofazimine monotherapy. Minocycline has the distinct advantage over other newer agents in proved safety for periods of administration longer than 1 month. Our findings in mice and clinical trial have now been confirmed in several locales.
We found in mice that kanamycin, streptomycin, and amikacin resulted in impressive killing of M. leprae (respectively, 99.7%, 97%, and 96%), while gentamicin and tobramycin had no such significant bactericidal effect. Importantly, we noted in mice that monthly streptomycin resulted in synergistic killing when combined with monthly rifampin. Although a number of studies have shown that streptomycin is effective against lepromatous leprosy, its requirement for injection and the high frequency of presumed drug-resistant relapse when used as monotherapy have limited its usefulness. With the current emphasis on developing very short, fully supervised therapy, perhaps it may yet play a role in the therapy of lepromatous leprosy. -Medical Research Institute at California Pacific Medical Center, 2200 Webster Street, San Francisco, CA 941 15-1896, U.S.A.
Franzblau, S. G., Harris, E. B. and Hastings, R. C. Macrolides, fusidic acid, lincosamides, and quinolones.
Using the in vitro metabolic activity of freshly harvested and highly viable Mycobacterium leprae from infected nude mice as a surrogate for viability of the organisms, we have screened over 100 compounds for antileprosy activity. In addition to the known antileprosy drugs we have found activity in unusual classes of drugs. The first of these was erythromycin. Customary screening concentrations of erythromycin in diets resulted in no detectable blood levels in mice. We then tested several newer macrolides with more favorable mouse pharmacokinetics and showed that clarithromycin, among others, was bactericidal in vivo as well as active against M. leprae in vitro. Fusidic acid is also active in vitro and, like erythromycin, has poor pharmacokinetics in the mouse. Fusidic acid is undergoing a clinical trial in leprosy patients without a preliminary mouse screening. Among the lincosamides, clindamycin seems promising in vitro. Among the fluoroquinolones, sparfloxacin is most potent in vitro against the leprosy bacillus. -Laboratory Research Branch, GWL Hansen's Disease Center at Louisiana State University, Baton Rouge, LA 70894, U.S.A.
Jacobson, R. R. Rifampin derivatives.
Rifamycin SV was the predecessor of rifampin and the first of the rifampin group of antibiotics to be extensively studied. Its activity in the treatment of leprosy patients was first reported in 1963. It was clearly effective but the necessity of giving it by injection limited its usefulness. Rifampin itself was then developed and its powerful bactericidal activity against Mycobacterium leprae and M. tuberculosis ultimately revolutionalized the treatment of leprosy and tuberculosis. Since that time, large numbers of rifampin derivatives have been developed and some have been tested in animal models and/or for activity in human leprosy. Thus far none has proven to have any significant advantage over rifampin itself.- GWL Hansen's Disease Center, 5445 Point Clair Road, Carville, LA 70721, U.S.A.
Freerksen, E. Short-term chemotherapy with rifampin + Cotrimoxazol + isoniazid (cotrifazide).
The experimental basis of the combination rifampin + Cotrimoxazol + isoniazid is briefly described. Its clinical application in the Paraguay Project with mostly LL cases revealed: a) high tolerance (in no case had treatment to be discontinued because of side effects), b) high practicability (due to its being offered as a fixed combination), c) a rapid effect allowing a short duration of treatment (a minimum of 2 months is recommended), d) good compliance, and e) attainment of bacterial negativity in the smear. This combination excels by its broad therapeutical spectrum, covering also infections often associated with leprosy (e.g., tuberculosis and other mycobacterioses, certain infections of the intestine or the urinary tract, as well as unspecific skin processes in relation with ulcera, etc.).-Sterleyer Str. 44, D-2410 Mölln, Germany.
Seydel, J. K. Brodimoprim/dapsone and brodimoprim/dapsone/rifampin; in vitro and in vivo results.
A new combination consisting of dapsone (DDS) and the dihydrofolate reductase inhibitor brodimoprim (BDP) has been developed for the treatment of leprosy. The combination of these two drugs shows strong synergistic inhibitory activity. This is demonstrated on Mycobacterium "lufu" as a model strain as well as on M. leprae in vitro. The in vitro efficacy has been convincingly confirmed in mouse foot pad experiments. The combination shows a perfect fit in its pharmacokinetic properties resulting in parallel serum concentrations (approximately 1:1 ratio) with a half life of approximately 24 hr. On the basis of these results, trials on previously untreated patients (≈ 100) have been performed in ALERT/Ethiopia and Asuncion/Paraguay with the following regimens: ALERT, A: 200 mg BDP daily, B: 200 mg BDP + 25 mg DDS daily and in Asuncion, C: 200 mg BDP + 100 mg DDS + 600 mg rifampin daily. Regimens A and B were stopped after 3 months of treatment and treatment was continued with WHO MDT in accordance with the initial protocol. Regimen B shows convincing clinical and laboratory efficacy after 3 months. Treatment with Regimen C was- in contrast to the initial protocol-completely stopped because of the excellent clinical results. Patients are now under relapse control. Tolerance of all three regimens was generally good. The combination of BDP/ DDS is highly effective and safe. -Forschungsinstitut Borstel, Med-Pharmazeut. Chemie, Parkalice 4a, D-2061 Borstel, Germany.
Session V
FUTURE RESEARCH IN IMMUNOLOGY AND MOLECULAR BIOLOGY
Chairman: Hans-Dieter Fiad
Kaufmann, S. H. E. Immunology.
T lymphocytes are the major mediators of protection against and the pathogenesis of leprosy. Two major T-cell populations are known: T cells expressing the α/β T-cell receptor represent > 90% of all peripheral T cells; the minor (< 10%) population expresses a γ/δ receptor. While only limited information is available about γ/δ T cells, α/β T cells have been analyzed more fully. So-called TH1 cells produce the cytokines interleukin 2 (IL-2) and interferon-gamma (IFN-γ) which activate important effector functions of antimicrobial resistance and often are cytolytic; so-called TH2 cells primarily secrete the B-cell stimulating IL-4, IL-5, and IL-10. These two T-cell subsets seem to negatively regulate each other. α/β T cells of the CD8 phenotype are primarily cytolytic and produce THl-like interleukins. Recently, production of TH2-like interleukins by CD8 T cells also has been described. Also, γ/δ T cells, after activation with mycobacteria, are cytolytic and secrete TH1 -like interleukins. Recent evidence indicates that interactions between these T-cell sets determine the final outcome of the immune response. Interleukins from TH 1 cells as well as cytolytic T cells contribute to protection. Target cell lysis may participate in pathogenesis. TH2-like activities are involved in specific unresponsiveness. A better understanding of these immune interactions may provide helpful information toward the rational design of immunomodulatory regimens for the therapy of leprosy.-Department of Immunology, University of Ulm, Albert-Einstein-Allee 11, D-7900 Ulm, Germany.
Watson, J. D. Understanding protective immunity to leprosy.
Leprosy remains a major health problem in tropical areas. An effective vaccine for leprosy is an important goal for immunologists. Recently, a large trial of a vaccine which incorporated BCG and killed Mycobacterium leprae was reported to have given no increased protection over the use of BCG alone (Convit, et al., Lancet 339 [1992] 446). This result is in agreement with animal studies, where it has been shown that vaccination with killed M. tuberculosis did not give protection against subsequent challenge with live M. tuberculosis (Orme, J. Immunol. 140 [1988] 3589). These studies have been interpreted to show that induction of protective immunity requires contact with live organisms. However, a recent study has shown that mice vaccinated with a protein extract of M. leprae are protected against subsequent challenge with live M. leprae in the foot pad (Gelber, et al., Infect. Immun. 60 [1992] 1840). Thus, the reason that killed mycobacteria do not confer protective immunity may be that they contain immunosuppressive components such as phenolic glycolipids and lipoarabinomannan. A major focus of recent research has been the cloning, sequencing and expression of the genes for M. leprae antigens, including the 18-kDa and 65-kDa antigens and superoxide dismutase. It seems likely that a suitable combination of recombinant-derived mycobacterial antigens will be able to make up an effective antimycobacterial vaccine. We are currently testing this concept in an animal model of mycobacterial disease. -Department of Molecular Medicine, School of Medicine, University of Auckland, Private Bag 92019, Auckland, New Zealand.
Cole, S. Molecular biology.
During the 1980s, leprosy research has benefitted considerably from the application of molecular biology, and several important advances in our understanding of the biology, genetics and immunology of Mycobacterium leprae were made. It is clear that our knowledge of the etiological agent of leprosy will expand on a much greater scale during the 1990s due to the impact of the M. leprae genome sequencing project and the implementation of surrogate molecular genetics. The vast quantities of data generated should lead to improvements in our conception of the problem and provide new leads for research in the chemotherapy and immunoprophylaxis of leprosy. Details are presented of the progress on the molecular biological front and points covered include the rapid detection of drug resistance, identification of new drug targets, and the construction of a centralized data base containing all available information of interest to leprosy research workers. -Laboratoire de Génétique Moléculaire Bactérienne, Institut Pasteur, 28 Rue du Dr. Roux, 75724 Paris 15, France.
FINAL REPORT
The Malta Experience
Although leprosy exists in sizable numbers in most parts of Africa, Asia and Latin America, prevalence is very uneven among and within countries. Of all registered leprosy patients 82% live in five countries: India, Brazil, Myanmar (Burma), Nigeria and Indonesia. Globally, there has been a reduction of 42% in registered cases between 1985 and 1992. However, approximately 600,000 new patients are detected each year, and the true annual incidence of leprosy may currently be close to 1 million. It is estimated that between 2 and 3 million individuals in the world are disabled because of leprosy, including those considered cured and removed from the registries.
Multidrug therapy (MDT) was attempted as early as the 1950s to improve the effect of treatment in those leprosy patients who were "poor responders" to sulfone. The therapy workshops of the 1963 and 1973 International Leprosy Congresses recommended some form of MDT to prevent or manage resistance to sulfone therapy.
In 1972 a unique program for the eradication of leprosy by multidrug chemotherapy was initiated by Prof. Enno Freerksen (Research Institute Borstel) in the island nation of Malta. Two-hundred-fifty-seven patients have been treated with Isoprodian-RMP. The mean duration of treatment was 23 months. The mean period of observation was 12.26 years. To date only one patient has relapsed 17 years after having completed MDT. In September 1992 the third independent review of the Malta study, under the auspices of the World Health Organization (WHO), was carried out. In agreement with the previous visits it was found at that time that in the 130 cases studied there is no evidence of active leprosy. This historical leprosy treatment trial initiated in Malta with the combined drug regimen of Isoprodian-RMP showed extremely encouraging results. It is considered today as an important landmark in the chemotherapy of leprosy (quoting Dr. Noordeen from WHO).
This Malta Isoprodian-RMP MDT trial has demonstrated that a) it is possible to have finite periods of treatment in leprosy irrespective of fears of relapse through persistence of M. leprae, b) successful chemotherapy of patients can reduce transmission of infection, and c) international cooperation involving nongovernmental organizations can be highly successful in contributing to leprosy control. In this connection the WHO and others noted the importance of recognizing the highly significant contribution made by the German Leprosy Relief Association in reducing the prevalence of leprosy in the world.
Ten years later in 1982 the WHO Study Group introduced an alternative MDT for the treatment of leprosy. Unfortunately, a decade later still only approximately 50% of all known leprosy patients receive MDT. There are over 4 million patients who are not being treated at all or not receiving MDT.
Efficacy and Side Effects of Isoprodian-RMP
Several presentations at this Symposium reviewed the efficacy of Isoprodian-RMP multidrug therapy. Large field trials have been conducted in countries such as India, Tanzania and Paraguay. The feasibility of the use and the efficacy of the Isoprodian-RMP treatment has been shown. Side effects reported for this drug combination were mostly minor. The more serious side effects (hepatotoxicities) were relatively rare. Hepatotoxicity may also be a problem of definition and may be caused by a number of geographic- and ethnic-dependent factors and drug unrelated (e.g., hepatitis, alcohol intake). Hepatotoxicity was seen in only 1.3% to 1.4% of treated patients, and gastrointestinal complaints in 5% to 30%. As already stated, major side effects were rare, possibly due to the strict adherence to dosage and administration according to body weight.
It was generally found at the II Wiirzburg Symposium on Chemotherapy that the Isoprodian-RMP treatment advocated by Prof. Freerksen back in the early 1970s has now been widely accepted.
Methods in Drug Screening and/or Therapeutic Monitoring
Many different in vitro tests were presented for drug screening and monitoring treatment. They included the macrophage system, fluorescent staining, ATP and adenylate charge measurement, thymidine uptake, palmitate oxidation, PGL-I synthesis, and the determination of sodium/potassium ratios and mass fingerprint pattern by the LAMMA technique as well as the use of a bacteriological in vitro test using model strains or M. leprae and BACTEC.
The use of immunochemical methods to study the cellular changes that occurred in leprosy lesions as a result of effective treatment was described, as well as the employment of the polymerase chain reaction (PCR) to detect leprosy bacilli in tissue samples. Evidence was presented for the increased sensitivity of the neonatally thymectomized Lewis rat for detecting small proportions of viable M. leprae from treated patients.
It was encouraging that when different techniques had been used concurrently to assess potential loss of viability, parallel findings were usually obtained. It would therefore be valuable to mount further comparative studies to assess the time pattern of losses in mouse foot pad infectivity, and losses of M. leprae's metabolic and synthetic activities following exposure in vitro and in vivo to different antileprosy drugs.
During the Round Table Discussion it became clear to all participants that existing MDT regimens have their limitations. They should be improved regarding antimicrobial activity, acceptability and ease of implementation in the field. The main difficulty in developing new drug combinations is the fact that there is no one method to date that may predict the cure or relapse of a leprosy patient.
New Antileprosy Drugs
There have been repeated efforts to synthesize improved clofazimine derivatives without significant success. However, one derivative (B 4100) showed slightly improved activity. Interest in heterocyclic hydrazones and N-alkylbenzylamines and in their synergistic combinations with other drugs was stressed because of their antileprosy activity. The importance and practical interest of dihydrofolate reductase inhibitors (K-130 and brodimoprim), alone or in combination with other drugs including dapsone and rifampin, has been studied at length in in vitro and in vivo tests in animals and in man with excellent short-term results. Among possible new targets for drug action, unique components of the mycobacterial cell wall might be of great interest for rational drug development. The powerful bactericidal activity of new fluoroquinolones such as ofloxacin and pefloxacin, clarithromycin and minocycline were stressed. In addition, fusidic acid and clindamycin seem to be promising in vitro. None of the newly developed rifampin derivates has demonstrated any significant advantage over rifampin itself.
Because of the highly promising activities of the newly developed antileprosy drugs the main emphasis of research in leprosy might be as follows:
- What are the drugs that should be combined with rifampin to obtain the most powerful activity against actively multiplying M. leprae and against metabolically inactive M. leprae (persisters)? In other words, what is the most efficacious drug combination which would permit the reduction of the length of treatment to a more acceptable duration, thus assuring a more generalized implementation of MDT?
- What are the laboratory and clinical tests which would permit the demonstration of the superiority of new drug combinations over the standard MDT regimens without having to evaluate efficacy by waiting for relapses?
Future Research in Immunology and Molecular Biology
Leprosy is one of a number of infectious diseases where the knowledge of both the pathogen and the host immune response following infection is essential for the understanding of the clinical spectrum of disease.
Three areas have been updated for the future:
• Analysis of the pathogenesis of the disease at the molecular and cellular level. This also involves the development of better methods for the early diagnosis of the disease.
• Generation of new vaccines to protect against infection. This involves the cloning, sequencing, and expression of genes of M. leprae and the definition of epitopes of M. leprae antigens which are recognized by human T lymphocytes and, thus, able to induce protective immunity.
• Need for better techniques to monitor chemotherapy and future immunotherapy, including the determination of serum antibodies and reactive T cells and immunohistochemistry.
SYMPOSIUM COMMITTEE
President
Wayne M. Meyers
Chief, Mycobacteriology
Armed Forces Institute of Pathology
Research Affiliate, Tulane University
Division of Microbiology
Armed Forces Institute of Pathology
Washington, DC 20306-6000/USA
Chairmen
Robert C. Hastings
Chief, Laboratory Research Branch
GWL Hansen's Disease Center at Louisiana State University
P.O. Box 25072, Baton Rouge, LA 70894/USA
G. A. Ellard
Scientific Officer
National Institute for Medical Research
The Ridgeway, Mill Hill London NW7 1AA, Great Britain
Louis Levy
Visiting Professor
Department of Dermatology
Hadassah University
P.O. Box 12000
IL-91120 Jerusalem, Israel
Jacques Grosset
Professor of Microbiology Faculté de Médecine Pitié-Salpêtrière
91 Boulevard de l'Hôpital
75634 Paris 13 France
Hans-Dieter Flad
Director
Department of Immunology and Cell Biology
Institute for Experimental Biology and Medicine
D-2061 Borstel, Germany
Responsible Organizers
Dr. Jürgen König, Medical Director GLRA
Prof. Dr. Joachim K. Seydel, Borstel
LECTURERS
Arnaldo E. ALVARENGA
Director del Departamento de Lepra, Ministerio de Salud Publica, Casilla de Correo 3054, Asunción, Paraguay
H. J. CHUM
Principal TB/Leprosy Consultant Ministry of Health, Ministry of Health, P.O. Box 8083 Dar es Salaam, Tanzania
Stewart T. COLE
Head of Laboratory, Laboratoire de Génétique Moléculaire Bactérienne, Institut Pasteur, 28, rue du Docteur Roux, F-75724 Paris Cedex 15, France
Arvind M. DHOPLE
Director, Infectious Diseases Laboratory, Department of Biological Sciences, Florida Institute of Technology, Melbourne, Florida 32901, U.S.A.
Manfred DIETRICH
Chief, Clinical Department Institute of Tropical Medicine, Bernhard Nocht Institute for Tropical Medicine, Bernhard-Nocht-Strasse 76, D-2000 Hamburg 36, Germany
G. A. ELLARD
Scientific Officer, National Institute for Medical Research, The Ridgeway, Mill Hill, London NW7 1AA, Great Britain
Hans-Dieter FLAD
Director, Department of Immunology and Cell Biology, Institute for Experimental Biology and Medicine, D-2061 Borstel, Germany
Enno FREERKSEN
Professor emer., Dr. med. Dr. phil., Sterleyer Strasse 44, D-2420 Mölln, Germany
Paul GATT
Senior Registrar in Dermatology, University Department of Dermatology, Sir Paul BofTa Hospital, Floriana Malta, 51/1 College Street, Rabat, Malta
Robert H. GELBER
Clinical Professor of Medicine, University of California, San Francisco; Director, San Francisco Regional Hansen's Disease Program, Kuzell Institute for Arthritis and Infectious Diseases, 2200 Webster Street, San Francisco, California 94115-1896, U.S.A.
Johannes GERDES
Head, Division Molecular Immunology, Institute for Experimental Biology and Medicine, D-2061 Borstel, Germany
Petra GRAF
Senior Medical Officer, Ministry of Health, TB/Leprosy Central Unit, Dar es Salaam, Tanzania, Tanzania Leprosy Association, P.O. Box , 5478, Dar es Salaam, Tanzania
Jacques GROSSET
Professor of Microbiology, Faculté de Médecine Pitié-Salpêtrière, 91, Boulevard de l'Hôpital, 75634 Paris CEDEX 13, France
Monika HAAS
Division of Biophysics, Institute for Experimental Biology and Medicine, D-2061 Borstel, Germany
Robert C. HASTINGS
Chief, Laboratory Research Branch, GWL Hansen's Disease Center at Louisiana State University, P.O. Box 25072, Baton Rouge, LA 70894, U.S.A.
Robert R. JACOBSON
Director, Division of National Hansen's Disease Programs; Director, Gillis W. Long Hansen's Disease Center, 5445 Point Clair Road, Carville, LA 70721-9607, U.S.A.
Baohong JI
Scientific Advisor, Association Française Raoul Follereau, Paris; Visiting Scientist, Faculté de Médecine Pitié-Salpêtrière, 91 Boulevard de l'Hôpital, 75634 Paris CEDEX 13, France
V. M. KATOCH
Head, Department of Microbiology, Central JALMA Institute for Leprosy, Taj Ganj, Agra 282 001, India
S. H. E. KAUFMANN
Chair, Department of Immunology, Institute of Microbiology of the University of Ulm, Albert-Einstein-Allee 11, D-7900 Ulm, Germany
Oscar LEGUIZAMON
Ministerio de Salud Pública, Departamento de Lepra, Casilla de Correo 3054, Asunción, Paraguay
Louis LEVY
Visiting Professor, Department of Dermatology, Hadassah University, P.O. Box 12000, IL-91120 Jerusalem, Israel
Buko LINDNER
Division of Biophysics, Institute for Experimental Biology and Medicine, D-2061 Borstel, Germany
P. R. MAHADEVAN
Director, The Foundation for Medical Research, 84-A, R. G. Thadani Marg, Worli, Bombay 400 018, India
Wolfgang MEINDL
University of Regensburg, Institute of Pharmacy, Universitatsstrasse 31, D-8400 Regensburg, Germany
Wayne M. MEYERS
Chief, Mycobacteriology, Armed Forces Institute of Pathology; Research Affiliate, Tulane University, Division of Microbiology, Armed Forces Institute of Pathology, Washington, D.C. 20306-6000, U.S.A.
Indira NATH
Professor and Head, Department of Biotechnology, All India Institute of Medical Sciences, New Delhi 110 029, India
S. K. NOORDEEN
Chief Medical Officer, Leprosy Unit, Division of Control of Tropical Diseases, World Health Organization, CH-1211 Geneva 27, Switzerland
Manuel Elkin PATARROYO
Professor, Universidad Nacional de Colombia; Director and Founder, Instituto de Inmunología; Adjunct Professor, Rockefeller University, Hospital San Juan de Dios, Carrera 10 Calle 1, Santafé de Bogotá D.C., Colombia
Klaus-Jürgen SCHAPER
Medicinal and Pharmaceutical Chemistry, Institute for Experimental Biology and Medicine, D-2061 Borstel, Germany
Joachim K. SEYDEL
Head, Medicinal and Pharmaceutical Chemistry, Institute for Experimental Biology and Medicine, D-2061 Borstel, Germany
Ulrich SEYDEL
Division of Biophysics, Institute for Experimental Biology and Medicine, D-2061 Borstel, Germany
Richard URBANCZIK
Chief, R& D Division of Fatol GmbH and Bacteriological Diagnostic Institute, Saarstickstoff Fatol GmbH, Robert-Koch-Strasse, D-6685 Schiffweiler, Germany
Klaus VISSER
Medicinal and Pharmaceutical Chemistry, Institute for Experimental Biology and Medicine, D-2061 Borstel, Germany
Michael F. R. WATERS
Consultant Leprologist and Microbiologist, Hospital for Tropical Diseases, London; member, Senior Scientific Staff of the British Medical Research Council; Consultant Adviser in Leprosy to the British Ministry of Health, Hospital for Tropical Diseases, 4 St. Pancras Way, London NW1 OPE, Great Britain
James D. WATSON
Professor and Head of the Department of Molecular Medicine, Department of Molecular Medicine, School of Medicine, University of Auckland, Private Bag 92019, Auckland, New Zealand
Paul R. WHEELER
Postdoctoral Scientific Officer, Department of Clinical Sciences, London School of Hygiene and Tropical Medicine, Keppel Street, London WC1E 7HT, Great Britain
Michael WIESE
Research Scientist, Medicinal and Pharmaceutical Chemistry, Institute for Experimental Biology and Medicine, D-2061 Borstel, Germany
PARTICIPANTS
Thomas ABRAHAM
Technical Advisory Unit, German Leprosy Relief Association, Regional Secretariat India, 4, Gajapathy Street, Shenoynagar, Madras 600 030, S. India
Wolfgang Count BALLESTREM
Casilla de Correos 661, Asunción, Paraguay
BEFIKADU Sissay
Head, National Leprosy Control Programme, P.O. Box 5033, Addis Ababa, Ethiopia
François BOILLOT
Leprosy Control Programme, P.O. Box 673, Freetown, Sierra Leone
Jean-Louis CARTEL
Institut de Léprologic Appliquée de Dakar (ILAD), B.P. 1 1023, Dakar-CD, Senegal
CHAROON Pirayavaraporn
Director, Leprosy Division, Soi Bamrasnaradoon Hospital, Tiwanond Road, Moo 4 Tambon Talaad Kwuan, Muang District, Nonthaburi 11000, Thailand
D. S. CHAUDHURY
Director, GRECALTES Training Centre, 23, Market Street, Calcutta 700 087, India
Thomas CHIANG
Marie Adelaide Leprosy Centre, Mariam Manzil, P.O. Box 8666, AM 21, off Shah-Rah-E. Liaquat, Karachi 74400, Pakistan
Maria da Graça CUNHA
Director, Instituto de Dermatologia Tropical e Venereologia "Alfredo da Matta," Rua Codajâs, 25, Cachocrinha 69063 Manaus, Amazonas, Brasil
George DEPASQUALE
% University Department of Dermatology, Sir Paul Boffa Hospital, Floriana, Malta
Martin DIETZ
% ALERT, P.O. Box 165, Addis Ababa, Ethiopia
Helmut FRANZ
Fatol Arzneimittel GmbH, Robert-Koch- Strasse, D-6685 Schiffweiler, Germany
R. GANAPATI
Bombay Leprosy Project, 6/27 Amar Bhuvan, Sion (East), Bombay 400 022, India
Herr GRÜTER
Aktion Medeor, St. Töniser Strasse 21, D-4154 Tönisvorst 2, Germany
P. HEINIGER
Ciba Geigy, CH-4002 Basle, Switzerland
Tonetaro ITO
Sasakawa Research Building, Soi Bamrasnaradoon Hospital, Tiwanond Road, Moo 4 Tambon Talad Kwuan, Muang District, Nonthaburi Province 11000, Thailand
Joseph KAWUMA
Buluba Leprosy Centre, P.O. Box 1059, Jinja, Uganda
Jindrich KAZDA
% Institute for Experimental Biology and Medicine, D-2061 Borstel, Germany
Young-Hoon KO
National Leprosy Control Supervisor, Korean Leprosy Control Association, Anyang P.O. Box 27, San 86, Ohjeonli, Euiwang-ub, Siheung-gun, Kyungkido, Republic of Korea
Sarah LACEY
ILEP Coordinating Bureau, 234 Blythe Road, London W14 0HJ, Great Britain
Mr. LAUF
Aktion Medeor, St. Töniser Strasse 21, D-4154 Tönisvorst, Germany
Derek LOBO
GREMALTES Referral Hospital & Leprosy Centre, 5 Gajapathy Street, Shenoynagar, Madras 600 030, S. India
Mrs. MALMESI
Ciba Geigy, CH-4002 Basle, Switzerland
Jaf MEHTA
Honorary President, Poona District Leprosy Committee, 35, "Manisha," 2-A Moledina Road, Pune 411 001, India Horst MÜLLER-BÜTOW Reppersberg Strasse 66, D-6600 Saarbrücken, Germany
Jean-Claude NAUDIN
German Leprosy Relief Association Secretariat, B.P. 8262, Dakar-Yoff, Senegal
Mr. PASTORS
Aktion Medeor, St. Töniser Strasse 21, D-4154 Tönisvorst, Germany
Ruth PFAU
Marie Adelaide Leprosy Centre, Mariam Manzil, P.O. Box 8666, AM 21, off Shah-Rah-E-Liaquat, Karachi 74400, Pakistan
Yasin Al-QUBATI
City of Light Hospital, P.O. Box 55722, Taiz, Republic of Yemen
Magdalena ROSENFELD
% Institute for Experimental Biology and Medicine, D-2061 Borstel, Germany
Mr. RYPKEMA
Aktion Medeor, St. Töniser Strasse 21, D-4154 Tönisvorst, Germany
Mr. SCHÜTZ
Fatol Arzneimittel GmbH, Robert-Koch- Strasse, D-6685 Schiffweiler, Germany
Wim VAN BRAKEL
Project Director, Leprosy Control Programme, Post Box No. 5, Pokhara 33701, Nepal
Matthias VENNEMANN
German Leprosy Relief Association, P.O. Box 18158, Ogbete, Enugu State, Nigeria
Hans-Uwe WENDL-RICHTER
German Leprosy Relief Association, P.O. Box 3017, Kampala, Uganda
YOUSSEF Wahba Aziz
Caritas Egypt, 13, Rue Dr. Abdel Hamid Said, Cairo, Egypt