- Volume 60 , Number 1
- Page: 102–4
Immunology of a burnt-out lepromatous leprosy patient
To the Editor:
We would like to present a 62-year-old male patient born in the province of Entre Rios, an endemic region of Argentina, who presented at our hospital without treatment and with a leonine facies (Fig. 1) and atrophy and scars (Fig. 2) consistent with Muir's description of burnt-out cases (8). The patient gave a history of having had the skin changes for 20 years. Repeated skin smears on the skin and nasal mucous membranes were negative for acid-fast bacilli (AFB). The patient underwent a skin biopsy which revealed a lepromatous infiltration of the dermis. Ziehl-Neelsen staining confirmed the lepromatous diagnosis because there were AFB in the vacuolated cells in the dermis (Fig. 3). Intradermal lepromin testing was negative for both the Fernandez and the Mitsuda reactions.
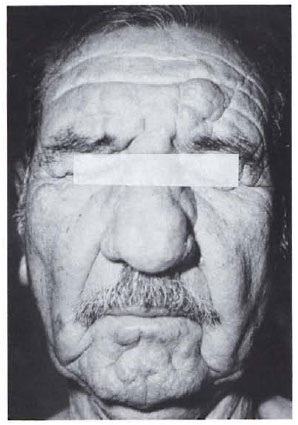
Fig. 1. Leonine facies.

Fig. 2. The strip on distal forearm and dorsum of the wrist and hand showing atrophy and scarring.
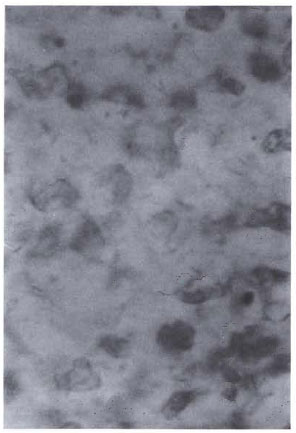
Fig. 3. Ziehl-Neelsen stain of skin biopsy showing acid-fast bacilli in vacuolated cells in the dermis.
Immunologic studies were performed as follows.
Humoral immunity. A large amount of antibodies of the IgG type against Mycobacterium leprae were found in this patient compared with a pool of treated LL patients' sera. The serum levels of IgG antibodies were tested employing sonicated M. leprae as antigen in an ELISA. IgG subclasses of anti-M. leprae antibodies were determined using monoclonal antibodies specific for the different IgG isotypes. The relative proportions of the subtypes were: IgG1, 65%; IgG2, 25%; IgG3, 10%; IgG4, not detectable.
Cellular immunity. T-cell cytotoxicity was measured against autologous macrophages with minor modification as described by Kaleab, et al. (6). Peripheral blood mononuclear cells (PMBC) were incubated for 7 days with or without the addition of M. leprae or PPD antigens. Target cells were adherent cells cultured for 6 days without antigen and pulsed 24 hr before the assay with the same antigens. Antigens were employed at the following concentrations: whole M. leprae, 1.8 x 107 bacilli/ml; M. leprae 65-kDa and 18-kDa recombinant proteins, 10 µ g/ml; and PPD (Statenseruminstitute, Denmark), 20 µ g/ml. Cytotoxicity was measured in a standard 4-hr 51Cr release assay. The following results were obtained at 40:1 effector/target cell ratio:
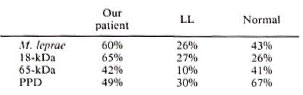
The patient thus shows a high level of T-cell cytotoxicity against autologous macrophages containing M. leprae antigens. M. leprae antigens were obtained through WHO IMMLEP. Whole and sonicated M. leprae were kindly provided by Dr. R. J. W. Rees and recombinant proteins by Dr. R. Van Der Zee.
Lymphocyte surface membrane markers. The surface membrane markers were determined from PMBC by direct reaction with fluorescein-labeled monoclonal antibodies. Anti-CD, (pan-T lymphocytes), anti-CD4 (helper-T lymphocytes), anti-CD (suppressor/cytotoxic lymphocytes), or anti-Leu 8 were used. The following results were obtained:
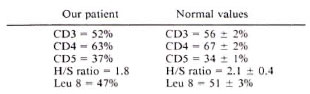
Previously we had found (10) that Leu 8 antigen was diminished in LL patients. Leu 8 antigen is analogous to Mel-14 murine lymphocyte homing receptor (2).
This patient shows cellular immunologic features of tuberculoid leprosy and humoral, immunologic and clinical histopathologic features of lepromatous disease. The patient had symptoms of the disease for 20 years, and had not been treated previously. When we started multidrug therapy, the patient experienced several episodes of erythema nodosum leprosum.
Hansen and Looft (5) pointed out that they had seen self-healing nodular leprosy in the field. The "N factor/Hansen anergic fringe" of Rotberg (9) may be decisive in a burntout lepromatous patient. The patient has a tuberculoid immunology, probably because he possessed the N factor even though he presented with a lepromatous appearance clinically. Maurano (7) studied seven burntout lepromatous patients with negative bacteriology and clinical skin lesions of atrophy and scars that resemble burns. Our patient has all the features of a burnt-out lepromatous patient.
It is pertinent to remember the patient described by Greene (4) in the book. A Burntout Case who had lost fingers and toes but had no other lesions. One can speculate that that case was pure neural tuberculoid in classification. A similar conclusion can be reached regarding the patient described in the book Inconfidencia (El Aleijadinho), which means The Little Cripple, by Arias (1), describing the life of the great sculptor of Ouro Preto, Brazil, who made the famous statues with the stumps of his hands.
To the best of our knowledge, this is the first burnt-out lepromatous case that has been studied immunologically. We would like to have information about other similar cases.
- Prof. Dr. Luis N. Baliña
Consultor Honorario
Unidad de Dermatologia
Hospital Argerich
Consulting Professor
Universidad del Salvador
Buenos Aires, Argentina
- Dra. Laura Jotimliansky
Medica Concurrente
Unidad de Dermatologia
Hospital General de Agudos "Dr. Cosme Argerich''
- Dra. Ma. del Carmen Sasiain
Bioquímica Investigadora
Inmunohematología (CONICET)
Academia Nacional de Medicina
- Dr. Fernando Minnucci, M.D.
CONICET Fellow
Academia Nacional de Medicina
- Dra. Ma. Cristina Kien
Médica Consultora
Dermapatología
- Dr. Edgardo Chouela
Jefe, Unidad de Dermatología
Hospital General de Agudos "Dr. Cosme Argerich"
REFERENCES
1. A RIAS, S. Inconfidencia (HI Aleijadinho). Buenos Aires: Editorial Sudamericana, 1979.
2. CAMERINI. D., JAMES, S. P., S TAMENKOVIC, I. and SEED, B. Leu-8/TQl is the human equivalent of the Mel-14 lymph node homing receptor. Nature 342(1989)78-82.
3. COCHRANE, R. Leprosy in Theory and Practice. 2nd ed. Bristol: John Wright & Co., 1964.
4. GREENE, G. Un Caso Acabado. 2nd ed. Buenos Aires: Editorial Sudamericana, 1975. In English: A Burnt Out Case. London: Penguin Books, Ltd., 1962.
5. HANSEN, A. and L OOFT, C. Leprosy in Its Clinical and Morphological Aspects. London: John Wright & Co., 1895.
6. KALEAB, B., OTTENHOFF, T., CONVERSE, P., HALAPI, E., TADESSE, G., ROTTEMBERG, M. and KIESLING, R. Mycobacterial-induced cytotoxic T cells as well as nonspecific killer cells derived from healthy individuals and leprosy patients. Eur. J. Immunol. 20(1990)2651-2659.
7. MAURANO, F. Contribuçoes para o estudio de cura e curabilidade da lepra. Os lepromatosos queimaos (burnt out). Rev. Bras. Leprol. 10(1942)189-205.
8. MUIR, E. Leprosy, self-healing disease. Lancet 1(1924)277-280.
9. ROTBERG, A. Some aspects of immunity in leprosy and their importance in epidemiology, pathogenesis and classification of forms of the disease; based in 1529 lepromin tested cases. Rev. Bras. Leprol. 10(1942)189-205.
10. SASIAIN, M. DEL C, DE LA BARRERA, S., VALDEZ, R. and BALINA, L. M. Reduced suppressor response to Mycobacterium leprae in lepromatous leprosy. Infect. Immun. 57(1989)951-956.
Reprint requests to Dr. L. M. Baliña, Av. Alvear 1890, 1129 Buenos Aires, Argentina.