- Volume 60 , Number 2
- Page: 269–70
Role of rifampin and clofazimine ointments in the treatment of leprosy
ABSTRACT
The use of rifampin and clofazimine ointments alone and in combination over the patches of tuberculoid patients has a beneficial effect. In combination (rifampin and clofazimine), erythema, inflammation, and edema are considerably reduced. For some of the cases with a recent appearance of a patch, the patch completely disappeared. It is suggested that topical therapy with rifampin and clofazimine ointments would be economical and beneficial in tuberculoid leprosy.In an effort to increase the utility of the JOURNAL in continuing medical education, in this section we welcome contributions dealing with practical problems in leprosy work. Submissions to this section will undergo minimal editorial changes and may well contain controversial points. Letters to the Editor pointing out other viewpoints are welcome.
The tuberculoid type of leprosy is distinguished by the presence of one or two patches, normally observed at the uncovered sites, with characteristic symptoms such as loss of sensation, loss of hair growth, and the absence of sweating in these patches. In such cases, Mycobacterium leprae, if present at all, will be only in the patches and will not be found elsewhere in the body. The conventional therapy is to administer dapsone alone, or dapsone in combination with rifampin, or dapsone, rifampin and clofazimine in combination, depending upon the condition of the patient. We contend that it would be more logical and economical if such patients are given local application of rifampin, the most powerful bactericidal agent, and clofazimine, a bacteriostatic and antiinflammatory agent, in a suitable ointment base from which the drugs could be absorbed readily at the site of application. Ointment base without drugs was used for control studies.
MATERIALS AND METHODS
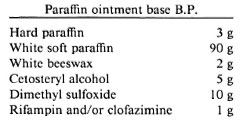
A paraffin ointment base B.P.1 was selected and modified by incorporating dimethyl sulfoxide which facilitates penetration of the drugs through the skin.
The first four ingredients were melted together by heating on a water bath. Rifampin/clofazimine was mixed with 10 g of dimethyl sulfoxide. The molten base was slowly triturated with rifampin/clofazimine in dimethyl sulfoxide in a clean dry mortar. The ointment was allowed to cool to room temperature and filled into collapsible tubes which were then crimped.
Tuberculoid patients with a patch having a distinct margin were selected for clinical trials from the Mahatma Gandhi Hospital and the Vishwakaruna Hospital, Warangal, A.P., India. The patients were advised to clean the patch thoroughly with warm water and soap and then to wipe the surface with a wet cloth. They were advised to apply the rifampin/clofazimine ointment on the patch two times a day with gentle rubbing. The ointment base without the drug was used as the control for the same patients. The patients' patches were examined for improvement, if any, once a week for 45 days; 49 patients were given this treatment.
RESULTS
The effect of rifampin and/or clofazimine ointment was investigated on 49 tuberculoid patients. There was no improvement in those patches where the ointment without drug was applied. It was observed that the rifampin ointment brought about considerable improvement on the patches. When the patch had occurred during the recent past, the ointment was able to bring it to a normal condition within 25-35 days. When the patches were distinctly hypopigmented, however, they did not disappear with this treatment. It was observed that the clofazimine ointment stained the patches. In a few patients with an inflamed, erythematous and edematous patch, the application of clofazimine ointment to the patch reduced these complications within a week, although the patch was still visible. It was observed that a combination rifampin-clofazimine ointment was much more effective than the ointments with the individual drugs.
DISCUSSION
In tuberculoid patients, a patch or two are seen on the body and the disease is highly localized. The patients are more worried about the patch than the disease itself. It was felt that for such a localized lesion topical treatment would, perhaps, serve better than systemic treatment. Preliminary tests conducted by Venkataramana2 show that rifampin in dimethyl sulfoxide when applied locally on the patch produced a beneficial effect in a limited number of patients.2 Clofazimine, apart from being an antileprotic, has antiinflammatory activity. This observation was re-examined in more patients with rifampin and clofazimine ointment alone and in combination. It is reported that in tuberculoid patients the M. leprae are found only in the patches. The blood flow to the skin is low;3 hence oral therapy may not result in the availability of adequate amounts of the drug at the affected site. To obtain high concentrations of the drug at the patch, an ointment is more suitable because large amounts of the drug can be made available at the local site and these high local concentrations of drug can attack M. leprae more effectively.
- B. Venkateswarlu
D. Venkataramana
A. V. N. Appa Rao
M. C. Prabhakar
University College of Pharmaceutical Sciences
Kakatiya University
Warangal 506 009, India
- B. Madhava Reddy
Mahatma Gandhi Memorial Hospital
Warangal, India
Acknowledgment. The authors are grateful to the staff of Mahatma Gandhi Memorial Hospital and Vishwakaruna Hospital, Warangal, A.P., India, for their cooperation. The authors are also grateful to M/S Ranboxy Laboratories Ltd., Lupin Laboratories Ltd., IDPL, for providing authentic raw material of rifampin and to ASTRAIDL Ltd. and S. G. Pharmaceuticals for providing clofazimine raw material as a gift for our present studies.
1. British Pharmacopoeia. London: Her Majesty's Office, 1988.
2. Venkataramana, D. Studies on rifampicin preparations in the treatment of leprosy. Master of Pharmacy thesis, Warangal, India, 1987.
3. Best and Taylor's Physiological Basis of Medical Practice. 11th ed. West, J. B., ed. Baltimore/London: Williams-Wilkins, 1985, pp. 136-139.
Reprint requests to Prof. Dr. M. C. Prabhakar.