- Volume 59 , Number 3
- Page: 392–7
Progression of eye lesions in leprosy: ten-year follow-up study in the netherlands
ABSTRACT
Forty-eight leprosy patients in The Netherlands were re-examined 10 years after initial examination. Forty-six of these patients had received a course of multidrug therapy (MDT), according to the World Health Organization recommendation, at the time of their initial examination. Two patients had burned-out disease and had been merely under observation. Out of 40 patients, who initially did not show eye complications due to leprosy, 37 patients were essentially the same 10 years later. The eyes had changed in 3 multibacillary patients: 1 patient had developed a late type 1 reaction with facial nerve involvement and lagophthalmos; 2 patients had undergone intra-ocular surgery for cataract and acute glaucoma, respectively. Out of 8 patients with pre-existing eye involvement, 1 patient recovered and the lesions in 2 patients remained unaltered. One patient showed progression of pre-existing exposure keratitis. Four patients had undergone cataract extractions; all four patients were lepromatous, with a long history of disease and signs of iris involvement at the first examination. The main progressive lesions were cataracts in lepromatous patients.RÉSUMÉ
Quarante-huit patients aux Pays-Bas ont été réexaminés 10 ans après l'examen initial. Quarante-six de ces patients avaient reçu un traitement par polychi-miothérapie (PCT), conformément à la recommandation de l'Organisation Mondiale de la Santé, à l'époque de leur examen initial. Deux patients avaient une maladie éteinte, et étaient simplement restés sous observation. Parmi les 40 patients qui à l'origine ne montraient pas de complications oculaires ducs à la lèpre, 37 étaient toujours ainsi 10 ans plus tard. Les yeux s'étaient modifiés chez 3 patients multibacillaires: 1 patient avait développé une réaction de type 1 tardive, avec atteinte du nerf facial et lagophtalmos; 2 patients avaient subi une chirurgie intra-oculairc, l'un pour cataracte, l'autre pour glaucome aigu. Parmi les 8 patients avec une atteinte oculaire pré-existante, 1 patient se rétablit, et les lésions de 2 patients restèrent inchangées. Un patient montra une progression de sa kératite. Quatre patients ont subi une intervention pour cataracte; tous les quatre étaient lépromateux, avec une maladie de longue durée et des signes d'atteinte de l'iris lors du premier examen. Les principales lésions qui ont montré une évolution défavorable étaient des cataractes chez des patients lépromateux.RESUMEN
Se reexaminaron 48 pacientes en Holanda, 10 años después de su examen inicial. Cuarenta y seis de estos pacientes habían recibido el tratamiento con múltiples drogas propuesto por la Organización Mundial de la Salud cuando se examinaron por primera vez. Dos pacientes habían eliminado la enfermedad y estaban solo en observación. De 40 pacientes, que inicialmcnte no mostraron alteraciones oculares debidas a la lepra, 37 pacientes permanecieron prácticamente igual 10 años después. En 3 pacientes, la situación ocular había cambiado: un paciente había desarrollado una reacción tardía del tipo 1 con afección de los nervios faciales y logoftalmos, dos habían sido sometidos a cirugía intraocular debido a cataratas o a glaucoma agudo. De 8 pacientes con afección ocular pre-existente: uno se había recuperado, en dos las lesiones permanecieron sin cambio, uno mostró progresión de su queratitis pre-existente, y cuatro habían sufrido extracción de cataratas: estos cuatro últimos pacientes eran lepromatosos con una enfermedad de larga evolución y signos de afección del iris en el tiempo de su primer examen. Las principales lesiones progresivas en los pacientes lepromatosos fueron cataratas.Some of the major complications in leprosy are potentially sight-threatening lesions. They are the result of either type 1 or type 2 reactions, or they are due to direct intra-ocular invasion by Mycobacterium leprae. Type 1 reactions may cause lagoph-thalmos through facial nerve involvement, and corneal hypesthesia through trigeminal nerve involvement. Type 2 reactions may cause acute iritis and scleritis. Invasion by M. leprae may give rise to a number of intraocular lesions of which chronic iritis and the resulting pin-point pupils with secondary cataract are potentially sight threatening. The World Health Organization (WHO) estimates that there are about 250,000 blind patients in a total of about 12 million leprosy patients (10). The statement "all leprous patients will eventually develop ocular complications" (13) is still regularly quoted. However, very few follow-up studies on the appearance or progression of ocular lesions have actually been published. Most data on eye involvement in leprosy have been derived from cross-sectional point-prevalence studies from institution-based or clinic-based populations (9). Little is known about the influence of antileprosy treatment on eye lesions.
We report here long-term follow-up results of eye examinations of a series of leprosy patients in The Netherlands. The great majority of the patients had been treated with a course of multidrug therapy (MDT) according to the WHO recommendations (24). Although the number of patients is fairly small, the scarcity of published follow-up data stimulated us to report our findings.
PATIENTS AND METHODS
In 1979, we studied eye involvement among 121 unselected consecutive leprosy patients attending the monthly leprosy outpatient clinic of the Department of Dermatology, Academic Medical Center of Amsterdam, The Netherlands (15). All patients were immigrants to The Netherlands or had contracted the disease while living in leprosy-endemic countries, and had been classified according to the Ridley-Jopling classification as modified by Leiker (16). Most patients had been using dapsone monotherapy and other antileprosy drugs for varying periods of time before they had been treated with MDT according the the WHO recommendations, with minor modifications, at the time of ophthalmological examination. Two patients had burned-out disease and had been merely followed.
Type 1 reaction patients had been treated with a course of systemic steroids, and type 2 reaction patients had generally been treated with thalidomide. After release from treatment the patients had been seen for regular follow-up by the dermatologist (WRF) once yearly. In case of complications, they were seen more frequently, as required.
In 1989, we called all patients who had been studied by us in 1979 for ophthalmological re-examination. The eye examinations at entry and re-examination were performed by the same person (MH) with an identical protocol. A history of any eye treatment during the last 10 years was taken. The routine eye examination consisted of inspection of the ocular adnexae, assessment of visual acuity (VA) for distance, slit-lamp examination, direct and indirect ophthalmoscopy and applanation tonometry for intra-ocular pressure (IOP).
Facial nerve function was tested by asking the patient to close the eyes gently as in sleep and as tightly as possible and then observing the completeness of closure and muscle strength. Corneal sensitivity was tested by touching the cornea with a wisp of cotton.
RESULTS
We re-examined 48 (40%) patients from the original study group of 121 (Table 1). The age range in the different classifications, the duration of the disease, and the period of follow-up since the end of the MDT course at the time of re-examination are given in Table 2. Borderline lepromatous (BL) and lepromatous (LL) patients generally were older and had a longer history of disease than tuberculoid (TT) and borderline tuberculoid (BT) patients. The mean period of follow-up since the end of the MDT course was 7 years.
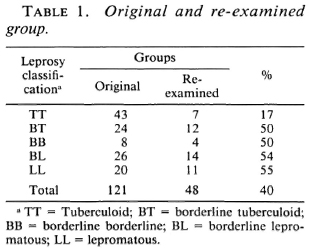
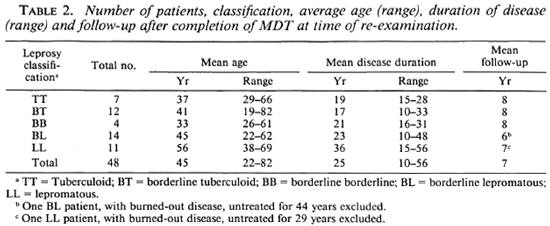
Table 3 shows the results of eye examinations in the re-examined group. Mada-rosis only, without eye lesions, was considered as "no eye complications.'" Out of 48 patients, 40 originally had had no eye complications due to leprosy; at re-examination 37 (92.5%) of them still had no eye complications. However, one BL patient (54 years of age; history of disease 24 years) had gone through a late type 1 reaction 5 years after completion of MDT, developing an erythematous patch on the face, bilateral facial nerve involvement, and lagophthal-mos. Two multibacillary (MB) patients, with initially normal eyes, had undergone intraocular surgery for cataract (LL) and acute glaucoma (BL), respectively.
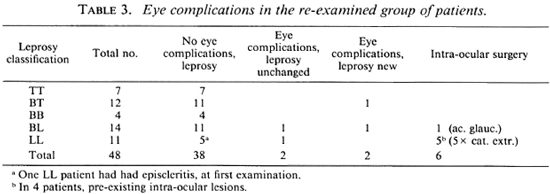
Eye complications at the original examination had been present in eight of the reexamined patients. Of them, one LL patient had had an episcleritis during type 2 reaction; he no longer showed any eye lesions. Eye lesions in two patients with longstanding disease essentially had remained unaltered: iris atrophy with a moth-eaten enlarged pupil and anterior synechiae and a staphylomatous blind second eye in a LL patient treated with MDT (50 years old; history of disease 38 years). Corneal chalky deposits, iris atrophy and pin-point pupil were symmetrical in both eyes of a BL patient (82 years old; history of disease 64 years; no treatment since 1955). Lesions in five patients progressed: one BT patient with pre-existing bilateral lagophthalmos and corneal hypesthesia had undergone unilateral tarsorrhaphy. This patient declined lid surgery on his other eye because of subjective loss of visual field after the surgery. The unprotected eye had developed corneal scarring in the lower temporal quandrant due to exposure keratitis. Four patients with longstanding lepromatous disease and preexisting iris involvement, such as iris atrophy and small pupils with or without posterior syncchiae, had been operated on for cataract, with or without artificial lens implantation.
Overall, no eye complications due to leprosy were seen in 38 (79%) out of 48 patients at the time of re-examination. Two patients had developed new lesions: lagophthalmos due to late type 1 reaction in a patient originally with normal eyes, and exposure keratitis in a patient with pre-existing lagophthalmos. Pre-existing eye lesions in two patients remained unaltered. Six patients underwent intra-ocular surgery, of whom four had shown signs of intra-ocular eye involvement before.
The visual acuity (VA) in the 48 re-examined patients was > 0.8 (> 20/25 or > 6/7.5) in one or both eyes of 41 (85%) patients and > 0.3 (> 20/60 or > 6/18) in 46 (96%) patients. No patient experienced a loss of visual acuity of > 2 lines on the Snellen chart during the time of observation. One BL patient with longstanding disease and multiple signs of intra-ocular leprosy had a VA of < 0.3 but > 0.1 (< 20/ 60 or 6/18 but > 20/200 or 6/60) unchanged since 1979. One patient was visually handicapped due to optic atrophy not related to leprosy. One eye of a lepromatous patient was blind in this series of 48 patients (96 eyes) due to staphyloma, unchanged since 1979. Intra-ocular pressure was essentially within normal limits (8-22 mm Hg).
DISCUSSION
Our original group of 121 patients had consisted mainly of immigrants. These people frequently move and therefore we had difficulties in tracing our original patients. We finally re-examined 48 (40%) of the original group. If TT patients, in whom eye complications are not to be expected, are excluded, we re-examined 39 (50%) of 78 patients. These problems in long-term tracing of leprosy patients are probably responsible for the scarcity of follow-up data.
Studies from the period before antilepro-sy drugs became available reported eye complications and blindness in up to 96% and 50% of the patients, respectively (13). At that time the prognosis of ocular leprosy was regarded as hopeless. After the introduction of dapsone treatment, several workers reported a favorable outcome of general antileprosy treatment on the occurrence and progression of eye lesions (1,4,7,22), and the reported prevalence of blindness in leprosy declined (11).
In the few follow-up studies of patients treated with dapsone monotherapy (2,5,21), lagophthalmos did not appear as a new lesion except in the case of dapsone-resistant disease. However, in existing lagophthalmos, exposure keratitis could develop or progress, with the risk of blindness. Therefore, timely tarsorrhaphy was advocated. Iritis appeared to be less favorably influenced by dapsone monotherapy and new cases of iritis appeared, especially in patients with continuing positive skin smears.
Recently a follow-up study over 2-4 years on 237 MB leprosy patients treated with MDT reported that the ocular status in 75% of the patients had remained normal or unaltered. Lesions such as (epi)scleritis, iritis and leproma subsided on MDT. New complications were usually minor in nature and were related to reactions and the duration of disease. Steroids, used for the treatment of reactions, induced posterior subcapsular cataracts (19).
Lagophthalmos develops as a result of type 1 reaction in the facial nerve. For corneal hypesthesia, the same mechanism is assumed. The great majority of type 1 reactions occur cither before treatment or during the first 6 months of treatment, especially in BT patients. Type 1 reaction in BL patients may occur over a longer period (up to 2 years 17). Late type 1 reaction after MDT occurs infrequently. Borderline patients are, therefore, most at risk for the development of lagophthalmos either before the onset of treatment or during the first 2 years of treatment. Indeed, lagophthalmos, as a new lesion, did not occur in the previously published follow-up studies. However, in our series it appeared once in a late type 1 reaction.
Type 2 reaction may develop in MB patients with longstanding untreated disease, but usually develops 2-3 years after the start of antileprosy treatment (6,18). Acute iritis and scleritis are considered manifestations of type 2 reaction in the eye. Therefore, BL and LL leprosy patients are, in particular, at risk of iritis and scleritis during treatment and early follow-up. However, once an eye has had acute iritis it seems to be more prone to recurrent iritis, without generalized signs of type 2 reaction. In longstanding and well-treated disease, the chance of the sudden appearance of these complications, as new lesions, seems small.
A large group of complications due to in-tra-ocular invasion with M. leprae may occur in MB patients with longstanding disease. Chronic iritis and iris atrophy leading to pin-point pupils with or without posterior synechiae and secondary cataract is the main cause of poor vision and blindness in such patients (8,14,23). Cataract was the most important lesion to progress in our series, and involved all LL patients with longstanding disease; 4 of the 5 patients had shown signs of iris involvement at the first examination. There may be four reasons for cataract in longstanding MB leprosy: a) secondary cataract due to iritis, b) secondary cataract due to treatment with systemic steroids in reactions, c) secondary cataract due to low IOP, and d) age related. Most cataracts in such patients seem to be secondary and occur at a relatively young age (3). This seemed to be the case in our patients as well.
Several authors have reported satisfactory results of cataract surgery in leprosy patients provided the patient is on regular treatment or released from treatment and has been free of reactions during the last 6 months (12,20). Care should be taken because of small pupils with friable iris tissue and in the case of low IOP (10). Therefore, intra-ocular lens implantation may be less suitable, in the case of eyes with chronic iritis.
We have found that the great majority of patients who had no lesions at initial examination did not develop eye lesions during a period of follow-up of 10 years. Nearly all of these patients had received a course of MDT. However, we should not ascribe these results to MDT alone, because the patients had relatively longstanding disease and most had been treated with dapsone monotherapy before. The critical period for the appearance of reactions might have already passed and the invasion of bacilli already halted. It is not yet clear if chronic iritis and secondary iris atrophy are due to persistent bacilli in the ciliary body or to an autoimmune process. In the first case, MDT, in which rifampin is bactericidal, may have a favorable influence. In the second case, the effect of MDT on chronic iritis will be less obvious. None of our patients had active chronic iritis at the time of re-examination.
In conclusion leprosy patients, after completion of MDT or with burned-out disease, run little chance of developing new lesions due to leprosy. The appearance of new eye lesions may, therefore, be a sign of relapse. Existing lesions usually stabilize or disappear. The manifold ocular complications that are seen in elderly patients with longstanding disease are probably due in the majority to a long delay between the onset of disease and the start of antileprosy treatment, reactions, or irregular treatment and relapses. However, exposure keratitis in lagophthalmos may progress as well as cataract in eyes which previously have been invaded by M. leprae and show signs of iris involvement. Acute iritis, once it has occurred, may recur at any time, without general symptoms of type 2 reaction and in spite of well controlled disease.
For the prevention of eye lesions in leprosy, all attention should be focussed on the early recognition and treatment of the disease to prevent further invasion of M. leprae into the eye and on the appropriate treatment of type 1 and type 2 reactions.
Acknowledgment. We thank Mrs. W. Knoote and the Q. M. Gastmann-Wichers Foundation for their kind support and administrative assistance.
REFERENCES
1. Amendola, F. Ocular and otolaryngological leprosy before and since sulfone therapy. Int. J. Lepr. 23(1955)280-283.
2. Brandt, F., Adiga, R. B. and Pradhan, H. Lag-ophthalmus und hintere Synechien der Iris bei der Behandlung der Lepra mit Diamino-diphenyl sul-fon. Klin. Monatsblat. Augenheilkd. 184(1984)28-31.
3. Brandt, F., Kampik, A., Malla, O. K., Pokhard, R. P. and Wos, J. Blindness from cataract formation in leprosy. Dev. Ophthalmol. 7(1983)1-12.
4. Brandt, F., Kist, P. and Wos, J. Augenbefunde bei Lepra. Ergebnisse einer Studie im Green-Pastures-Leprosy-Hospital Pokhara/Nepal. Klin. Monatsblat. Augenheilkd. 178(1981)55-58.
5. Brandt, F. and Shrestha, K. B. Uber den Wandel von ophthalmologischen Befunden bei Morbus Hansen untcr Chemothcrapic. Fortschr. Ophthalmol. 79(1983)455-457.
6. Browne, S. G. Erythema nodosum in leprosy. J. Chron. Dis. 16(1963)23-30.
7. Choyce, D. P. Ocular complications of common tropical disease, leprosy. Int. Ophthal. Clin. 7(1967)493-512.
8. Choyce, D. P. Diagnosis and management of ocular leprosy. Br. J. Ophthalmol. 53(1969)217-223.
9. Courtright, P. D. Defining the magnitude of ocular complications from leprosy: problems of methodology. Int. J. Lepr. 56(1988)566-573.
10. Courtright, P. and Johnson, G. Blindness Prevention in Leprosy. London: International Centre for Eye Health, 1988.
11. Emiru, V. P. Ocular leprosy in Uganda. Br. J. Ophthalmol. 54(1970)740-743.
12. ffytche, T. J. Cataract surgery in the management of the late complications of lepromatous leprosy in South Korea. Br. J. Ophthalmol. 65(1981)243-348.
13. Harley, R. D. Ocular leprosy in Panama. Am. J. Ophthalmol. 29(1946)295-316.
14. Houbs, H. E. Leprotic iritis and blindness. Int. J. Lepr. 40(1972)266-374.
15. Hogeweg, M. and Leiker, D. L. A survey on eye involvement among leprosy patients in The Netherlands. Doc. Ophthalmol. 56(1983)69-76.
16. Leiker, D. L. Classification of leprosy. Lepr. Rev. 37(1966)7-15.
17. Naafs, B. and Wheate, H. W. The time interval between the start of anti-leprosy treatment and the development of reactions in borderline patients. Lepr. Rev. 49(1978)153-157.
18. Pfaltzgraff, R. E. and Bryceson, A. Clinical leprosy. In: Leprosy. Hastings, R. C, cd. Edinburgh: Churchill Livingstone, 1985, pp. 168-171.
19. Rajan, M. A. Eye in multi drug therapy. Indian J. Lepr. 62(1990)33-38.
20. Rao, V. A. and Kawatra, V. K. Cataract extraction in leprosy patients. Lepr. Rev. 59(1988)67-70.
21. Somerset, E. J. and Sen, N. J. Prognosis of the ocular lesions of leprosy. Lepr. India 29(1957)142-147.
22. Ticho, U. and Sira, I. B. Ocular leprosy in Malawi. Clinical and therapeutic survey of 8,325 leprosy patients. Br. J. Ophthalmol. 54(1970)107112.
23. Weerekoon, L. Ocular leprosy in Ceylon. Br. J. Ophthalmol. 53(1969)457-465.
24. WHO Study Group. Chemotherapy of Leprosy for Control Programmes. Geneva: World Health Organization, 1982. Tech. Rep. Ser. 675.
1. M.D., Department of Ophthalmology, Erasmus University Rotterdam, P.O. Box 1738, 3000 DR Rotterdam, The Netherlands.
2. M.D., Department of Dermatology, Academic Medical Centre, University of Amsterdam, Meibergdreef 9, 1105 AZ Amsterdam, The Netherlands.
Reprint request to Dr. Hogeweg at present address: Department of Ophthalmology, Leiden University, P. O. Box 9600, 2300 RC Leiden, The Netherlands.
Received for publication on 15 November 1990.
Accepted for publication in revised form on 26 March 1991.