- Volume 59 , Number 3
- Page: 398–404
Detection of M. leprae-specific antigens with dot-ELISA in urine and nasal samples f rom leprosy patients
ABSTRACT
One-hundred-two urine and nasal samples collected f rom leprosy patients of different classifications of disease were studied for the presence of Mycobacterium leprae antigens, including phenolic glycolipid-I (PGL-I). Lipids were extracted f rom the urine samples, and nasal washings were concentrated and used as such in the dot-ELISA. Two types of primary antibodies, a polyclonal antibody obtained f rom lepro-matous (LL) leprosy patients' pooled and absorbed sera and an anti-PGL-I monoclonal antibody, were used for the detection of M. leprae antigens f rom these samples. The polyclonal sera detected 23% to 36% of the paucibacillary (PB) and 100% of the multibacillary (MB) leprosy cases f rom the urine samples. Corresponding values for nasal detection were 10% to 18% for PB and 100% for MB cases. The monoclonal antibody against PGL-I could not detect tuberculoid (TT) leprosy cases. F rom the urine samples, however, 16% of the borderline tuberculoid (BT), 25% of the borderline (BB), 80% of the borderline lepromatous (BL), and 100% of the LL leprosy cases were detectable. It was interesting to note that PB, skin-smear negative cases were detectable f rom urine examination. The specificity and sensitivity of the test is discussed in relation to the crossreacting antigens.RÉSUMÉ
Cent-deux échantillons d'urine et en provenance des fosses nasales prélevées chez des patients lépreux présentant différents types de la maladie ont été étudiés pour rechercher la présence d'antigènes de Mycobac-terium leprae, y compris le glycolipide phénoliquc-1 (PGL-1). Les lipides ont été extraits des échantillons d'urine, et les lavements en provenance des fosses nasales ont été concentrés et utilisés comme tels pour l'ELISA. Deux types d'anticorps primaires, un anticorps polyclonal obtenu à partir de sérums mis ensemble et absorbés provenant de patients lépromateux (LL), et un anticorps monoclonal anti-PGL-I ont été utilisés pour la détection des antigènes de M. leprae à partir de ces prélèvements. Les sérums polyclonaux ont détecté de 23% à 36% des cas paucibacillaires (PB) et 100% des cas de lèpre lépromateusc (MB). Les valeurs correspondantes pour les prélèvements à partir des fosses nasales étaient de 10% à 18% pour les cas PB et 100% pour les cas MB. L'anticorps monoclonal vis-à-vis de PGL-I ne pouvait pas détecter les cas de lèpre tuberculoïde (TT). A partir des échantillons d'urine, cependant, 16% des cas borderlinc tuberculoides (BT), 25% des borderline (BB), 80% des borderline lépromateux (BL) et 100% des cas LL pouvaient être détectés. Il était intéressant de remarquer que des cas PB, négatifs au frottis cutané, pouvaient être détectés à partir de l'examen des urines. La spécificité et la sensibilité du test sont discutées en relation avec les antigènes réagissant de manière croisée.RESUMEN
Se colectaron muestras de orina y de secreciones nasales de 102 pacientes con lepra de diferente clasificación para buscar la presencia de antígenos del My-cobacterium leprac incluyendo al glicolípido fenólico 1 (PGL-I). Los lípidos extraídos de las muestras de orina y los lavados nasales concentrados, se usaron en una prueba de ELISA en gota (dot-ELISA). Para la detección de antígenos del M. leprae se usaron dos tipos de anticuerpos primarios: uno policlonal obtenido de una mezcla de sueros de enfermos con lepra, y uno monoclonal anti-PGL-I. Los anticuerpos policlonales detectaron del 23 al 36% de los casos paucibacilares (PU) y al 100% de los casos multibacilarcs (MB) a partir de las muestras de orina. Los valores correspondientes para la detección nasal fueron del 10-18% para los casos PB y del 100% para los casos MB. El anticuerpo monoclonal anti-PGL-1 no pudo detectar a los casos tuberculoides (TT). Sin embargo, a partir de las muestras de orina se pudieron detectar, el 16% de los casos intermedios-tubereuloides (BT), el 25% de los casos intermedios (BB), el 80% de los casos íntermedios-lepromatosos (BL), y el 100% de los casos LL. Fue interesante notar que los casos PB, negativos en los extendidos de linfa cutánea, pudieron ser detectados a partir de las muestras de orina. Se discute la especificidad y sensibilidad de la prueba en relación a los antígenos de reacción cruzada.The detection of leprosy based on conventional clinical, bacteriological, and his-topathological examinations is often possible only at a time when physical deformities and nerve damage have disturbed the routine life of the patients. In fact, early leprosy is difficult to diagnose but easy to treat. Therefore, the diagnosis of leprosy at an early stage before clinical manifestations is of great interest today. Several attempts have been made in this direction without much success. Failure in cultivation and isolation of the causative organism of leprosy has left serological diagnosis as the most promising alternative.
There seems to be little involvement of the internal organs in leprosy, but the kidneys have been one of the target organs of infection (15), and antigens/antibodies are reported to be excreted in the urine of leprosy patients (10,14). In our own observations (8), the presence of antigens in the urine of different types of leprosy patients has been detected by dot-ELISA.
In addition to urine, nasal secretions also have been examined for the presence of acid-fast bacilli (AFB) as a prelude to diagnosis by several leprologists (6,7,13) who, beyond doubt, have proven that a heavy load of AFB is excreted in nasal discharges of leprosy patients having disseminated disease (BL/LL). The relationship of actual excretion of bacilli with the spectrum of the disease is not known precisely. Shedding of detectable bacilli in the nasal mucus may be preceded by excretion of soluble anti-gen(s). The detection by serological tests of soluble antigens in nasal excretions has not attracted much attention. The development of methods for detecting soluble excretory antigen(s) in urine and nasal samples simultaneously may provide useful information leading to the diagnosis of even early cases of leprosy; this we have attempted during the present studies.
MATERIALS AND METHODS
Collection of samples. A total of 102 urine samples (100-300 ml) and 102 nasal samples were collected from fresh cases (having no known history of any treatment) of different types of leprosy classified according to the Ridlcy-Jopling scale (16). The samples consisted of 30 TT, 22 BT, 5 BB, 20 BL, and 25 LL cases attending the Leprosy Control Unit, Chandar Nagar, Lucknow, U.P., India. Duration of the clinical disease varied from 1 month to 13 years (Table 1). In addition, 12 contacts (4 contacts of BT cases and 8 of BL patients) who were either siblings or spouses of leprosy patients (Table 2) were also included in the study (6 to 10 years of contact). A total of 10 urine samples and nasal swabs were collected from apparently healthy persons (ages varying from 20-30 years) from nonendemic areas (incidence of leprosy < 0.5 per thousand and 130 km away from an endemic area having 1-5 per thousand incidence rate) were included as normal controls. Urine samples were first centrifuged at 37,000 x g. The deposits were smeared, stained by the Ziehl-Neelsen method, and examined for the presence of AFB.
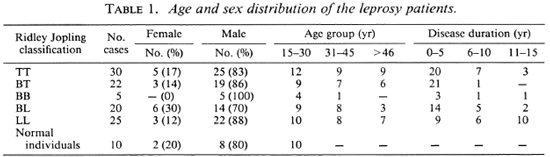
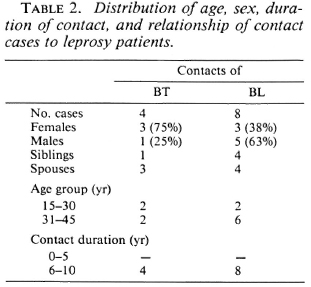
Nasal excretions were collected by rinsing the nasal tract with a moist cotton swab, finally suspended thoroughly in 5 ml normal saline (0.85% w/v). Two smears from each nasal sample were made, stained, and examined for intact bacilli. The saline suspension was finally concentrated to 20 x volume by lyophilization and used for the detection of Mycobacterium leprae antigens.
Slit-skin smears from six different sites (carlobes, chin, eyebrows and from an actual patch on the body) were made, stained, and examined for AFB.
Anti-M. leprae hyperimmune serum was prepared by collecting 15 ml of venous blood from each of five LL patients which was then pooled and preserved by deep freezing. Similarly, anti-A/. tuberculosis hyperimmune serum was prepared from frank cases of pulmonary tuberculosis, pooled together, and stored by deep freezing.
Lipid extraction from urine samples. The method of Bligh and Dyer (3) was applied for the extraction of lipids from the urine samples (50 ml each), and the final lipid extract was dissolved in 1 ml hexane and used in a dot-ELISA.
Preparation of mycobacterial antigens. The cultivable mycobacteria representing each group of Runyon's classification (17) and other related species were cultivated in Sauton's liquid medium. These included BCG, M. phlei, M. vaccae, M. intracellulare, M. scrofulaceiun, and M. sineginatis. The mycobacteria were grown separately, harvested, washed with saline, and sonicated with a cell disruptor (Model W-22F; Heat Systems-Ultrasonics, Inc., U.S.A.) at 20 kc/ sec for 4 x 5 min in an ice-water bath until about 90% of the cells were disrupted and the protoplasmic contents liberated (on smear examination of sonicates). The sonicates were centrifuged at 16,000 x g to separate the debris from the protoplasmic contents, and the supernatants were collected and stored at - 20ºC until used.
Absorption of sera. Soluble (sonicated) antigens of these mycobacteria were used in the agglutinin-absorption test to make the pooled LL-patient and TB-patient sera monospecific following the method of Abe, et al. (1). In brief, a minimal quantity of 0.5 ml of scrum was mixed with an equal volume of six sonicated antigens (0.05 ml of each of six mycobacterial antigens) to make a final concentration of 0.30 ml of total antigens in 0.05 ml of serum. This was diluted to a final concentration of 1:10 with the addition of 0.15 ml cardiolipin-lecithin mixed in phosphate buffered saline (PBS) (1:19). The mixture was incubated at 37ºC for 1 hr, and centrifuged at 500 x g for 15 min to clear off the agglutinated mass from the supernatant solution. The supernatant was recentrifuged at 5500 x g for 5 min in a microcentrifuge (M-15; Sakuma Seisaku-sho Ltd., Ohta-Ku, Tokyo, Japan). The clear supernatant was collected and diluted in antibody buffer to prepare the optimal dilution for the test.
Anti-PGL-I monoclonal antibody. Anti-phenolic glycolipid-I (PGL-I) monoclonal antibody was obtained through the kind courtesy of Dr. Thomas Shinnick, Centers for Disease Control, Atlanta, Georgia, U.S.A., through the UNDP/World Bank/ Special Programme for Research and Training in Tropical Diseases.
Standardization of the optimal dilution of serum and conjugate. One µg/ml of known PGL-I antigen (obtained from Dr. Patrick Brennan, Colorado State University, Fort Collins, Colorado, U.S.A.) was tested with a series of serum dilutions ranging from 1:50 to 1:500 of pooled and absorbed LL patients' sera along with 1:500 to 1:5000 dilutions of horseradish peroxidase (HRP)-antihuman IgM conjugates in different sets. On the basis of the highest color intensity, the 1:100 dilution of serum and the 1:1000 dilution of HRP-antihuman IgM were found to give the optimal reaction in dot-ELISA, and were used in further studies.
Dot-ELISA. The dot-ELISA was performed according to the method described by Aguado Sanchez, et al. (2) with slight modifications. Two types of primary antibodies were used in the test: One was monospecific, antileprosy hyperimmune sera from LL patients prepared by us, and the other was a monoclonal antibody against the PGL-I antigen obtained elsewhere. Nitrocellulose (NC) filter strips (pore size 0.22 yum; S and S Company, Germany) were used as the solid support. These NC strips were soaked in distilled water and then air dried. Five µl of the samples in two sets were dotted on the separate strips. Nonspecific sites were blocked by incubation in Tris buffered saline (TBS)-BSA (20 mm Tris, 150 mm NaCl, pH 7.4, 0.5% w/v bovine serum albumin) for 1 hr at 37ºC. One set of NC strips was washed 4x5 min in TBS and then incubated for 1-2 hr at 37ºC with standard (pooled and absorbed) LL patients' sera diluted by TBS-0.5% BSA (1:100). The other set was incubated with BT patients' monospecific hyperimmune sera. NC strips were rewashed 4x5 min in TBS, rinsed twice with Tris-saline, and incubated with HRP antihuman IgM (Sigma Chemical Co., St. Louis, Missouri, U.S.A.) at 1:1000 dilution in TBS-BSA for 1 hr at 37ºC. After 4x5 min washing in TBS, the NC strips were stained with 3'3-diaminobenzidine tetra-hydrochloride (Sigma) in 20 mM Tris with 25 µl H2O2. Finally, the strips were rinsed in TBS and dried between Whatman filter paper no. 1, and examined for color development at the test spots.
Dot-ELISA with anti-PGL-I monoclonal antibody, using the method of Kaldany and Nurlign (11), was performed similarly except that the PGL-I monoclonal antibody was used as the primary antibody and anti-mouse peroxidase conjugate as the secondary antibody.
RESULTS
With LL patients' monospecific sera, it can be seen that the lipid extracts of urine from the LL patients developed the highest color on the nitrocellulose strips (Fig. 1), thereby showing the presence of lipid antigens in the urine samples. No color developed in the urine of the contacts, suspected cases, or normal controls. There was 100% positivity for all of the multibacillary (MB) leprosy cases, whereas 23% of the TT and 36% of the BT cases were found to be positive for the presence of M. leprae-spc-cific antigens (Table 3).
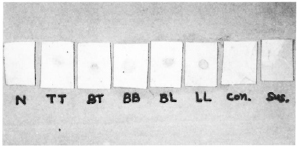
Fig. 1. Detection of M. leprae-specific lipid antigens in urine samples (lipid extracts) using horseradish peroxidase anti-human IgM.
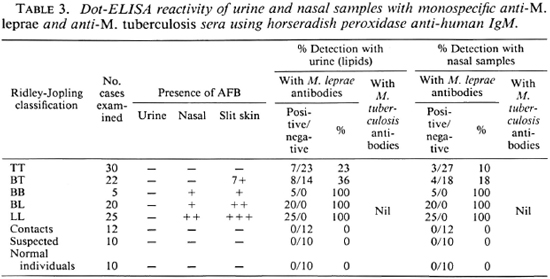
Corresponding values obtained from nasal swabs of the same patients, using LL patients' monospecific sera as primary antibody, resulted in 10% and 18% positivity for M. leprae-specihe antigens among TT and BT cases, respectively. All of the MB cases were detectable from the nasal samples by dot-ELISA (Table 3, Fig. 2). None of the nasal samples from contacts, suspected cases, or normal individuals were positive. There were variations in the color intensities of the dots from different patients of the same type of leprosy (i.e., among different TT cases and among different BT cases, etc.), which possibly may be due to differences in the duration of the disease.
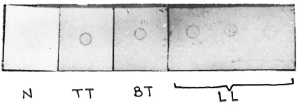
Fig. 2. Differences in color intensities between nasal samples of different classifications of leprosy patients and normal individuals.
Slit-skin smears (at six different sites), urine smears, and nasal smears were all examined for the presence of AFB. The urine smears from all of the samples, irrespective of disease, were negative for the presence of intact AFB. All TT patients were found to be AFB negative on skin and nasal smear examinations. A total of 7 out of 22 BT cases showed small numbers of AFB in skin smears, whereas all BB, BL, and LL cases were skin-smear positive (1 +-5+ bacterial index). However, the nasal smears of only the BL and LL cases were AFB positive (Tables 3 and 4).
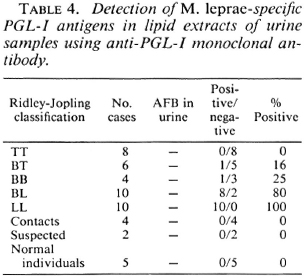
To establish the specificity of the test, anti-PGL-I monoclonal antibody was used in place of the primary antibody with lipid-extracted antigen from the urine samples. No case from TT patients was positive with this test, but 16% of the BT, 25% of the BB, and 80% of the BL cases were positive. All of the LL cases (100%) were positive for PGL-I antigen in the lipid extracts of urine (Table 4). All samples from contacts, suspected cases, and normal individuals were negative (Fig. 3).
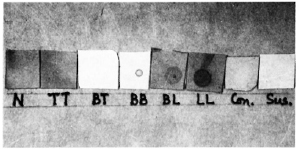
Fig. 3. Detection of PGL-I antigen using anti-PGL-I monoclonal antibody with lipid extracts of urine samples.
The presence of antigen(s) in the urine (lipid extracts) and nasal swabs of these leprosy patients reacting with antituberculosis antibodies was also examined on separate nitrocellulose strips using the dot-ELISA technique. The antituberculosis absorbed sera were unable to bind with lipid-extract-ed M. leprae antigens in the urine samples or with the lyophilized nasal washings in the dot-ELISA. There was no indication of any color development, even in those samples which were positive with pooled and absorbed antileprosy sera.
DISCUSSION
One of the major problems in leprosy control and eradication is the absence of an easy, simple and specific diagnostic test for early case detection. Skin-smear examination fails to confirm the disease in the major part of the leprosy spectrum or the cases are detected at a time when disease has produced full-blown symptoms or after the disease has entered into the multibacillary stages. The specificity of skin smears is subject to error primarily because all AFB, not just M. leprae, are stained and observed in the sample. Therefore, critical evaluation by an experienced observer is required. On several occasions leproma-derived mycobacteria (LDM), which are not just M. leprae, have been isolated and a large number of such bacteria exist in cultures now. Sensitive tests such as the radioimmunoassay (RIA), conventional enzyme-linked immunosorbent assay (ELISA), and histopa-thology are being tried with limitations.
During causation of a disease, the host body experiences the pathogen first, provoking the formation of antibodies at a later date. It is likely that antigen(s) might be excreted in soluble/insoluble forms in the humors through the body orifice even earlier than the formation of detectable antibodies. Diagnosis based on the detection of antigen has superiority over antibody detection since crossreactivity can be largely avoided in the identification of specific antigens. The present investigation has attempted to elucidate the presence of antigens in urine and nasal secretions of leprosy patients. An interesting observation was that none of the urine samples revealed the presence of intact bacilli in smears, whereas the lipid extracts of these urine samples yielded detectable quantities of M. leprae-specific antigens, from almost the entire spectrum of the disease, although to a variable extent.
To enhance the sensitivity of the dot-ELISA, nitrocellulose filter strips of 0.22 μm pore size have been used in place of the usual 0.45 μmpore size to permit better retention of the lipid molecules. The LL patients' sera were absorbed with different mycobacterial antigens (M. phlei, M. tuberculosis, BCG, M. vaccae, M. intracellulare, M. smegmatis, M. scrofulaceum), cardiolipin, and lecithin to make them monospecific. This also reduced the nonspecific bindings and removed group antibodies which increased the specificity and sensitivity of the test. The methods of absorption of the serum samples with different mycobacterial antigens (1) and extraction of lipids from the urine samples (3) are simple and consume little time. The specificity of the test has been further established since M. leprae-specific antigens did not react with antituberculosis sera.
Although the use of LL patients' sera (pooled and observed) as the primary antibody in the dot-ELISA yielded satisfactory sensitivity among paucibacillary and multibacillary cases, the specificity of the test was questionable. To establish the specificity of the test, a small number of samples were tested using anti-PGL-I monoclonal antibody as the primary antibody in the dot-ELISA. PGL-I monoclonal antibody specifically bound with the PGL-I antigen present in the lipid extracts of urine, and the percentage positive among paucibacillary cases declined in comparison with the use of the monospecific polyclonal sera. This possibly may be due to a higher limit of detectable antigen in the lipid extracts of urine for the monoclonal antibody, or that lipids other than PGL-I are being detected by the polyclonal serum.
Goldschmidt (9) was probably the first to observe excretion of AFB in the nasal secretions of leprosy patients, which was also noted by Koch (12) in nasal ulcers. Since then, several investigators have shown the presence of AFB in nasal smears of multibacillary cases. At times these investigators failed to find bacilli in nasal smears, and the excretion of AFB in TT and BT cases is rare.
The presence of soluble antigens may precede the actual shedding of bacilli, hence these antigens are likely to be detected in a dot-ELISA even when the actual smear is negative for AFB. The application of a dot-ELISA with crude nasal secretions is a novel study and has provided satisfactory results. The modifications described here have raised the sensitivity as well as the specificity of the assay, which has been improved with the use of PGL-I-specific monoclonal antibody. The contacts, all of whom were found negative, are being monitored for the development of actual disease, and their nasal and/or urine positivity for the antigen in ELISA is being monitored for future guidance.
Acknowledgment. The authors are grateful to Dr. B. N. Dhawan, Director, for his keen interest in the work. The kind cooperation and help provided by Dr. Riazul Hasan, Medical Officer-In-Charge, Leprosy Control Unit, Chandar Nagar, Lucknow, India, is greatly acknowledged. The technical assistance of Shri Suni Chakraborty and Hori Lai has always been greatly appreciated. One of the authors (AC) is obliged to CSIR for financial assistance.
REFERENCES
1. Ahe, M., Minayawa, F., Yoshino, Y., Ozawa, T., Saikawa, K. and Saito, T. Fluorescent leprosy antibody absorption (FLA-ABS) test for detecting subclinical infection with M. leprae. Int. J. Lepr. 48(1980)109-119.
2. Aguando Sanchez, G., Malik, A., Tougne, C, Lambert, P. H. and Engers, H. D. Simplification and standardization of sérodiagnostic tests for leprosy based on phenolic glycolipid-I (PG-I) antigen. Lepr. Rev. 57 Suppl. 2(1986)83-93.
3. Bligii, E. G. and Dyer, W. J. A rapid method of total lipid extraction and purification. Can. J. Bio-chem. Physiol. 37(1959)911-917.
4. Brennan, P. J. The carbohydrate containing antigens of M. leprae. Lepr. Rev. 57 Suppl. 2(1986)39-51.
5. Cno, S.-N., Yanagihara, D. L., Hunter, S. W., Gelber, R. H. and Brennan, P. J. Serological specificity of phenolic glycolipid-I from Mycobacterium leprae. Infect. Immun. 41(1983)10771083.
6. Davey, T. F. and Barton, R. P. E. Multiple nasal smears in early lepromatous leprosy. Lepr. India 45(1973)54-62.
7. Davey, T. F. and Rees, R. J. W. The nasal discharge in leprosy- clinical and bacteriological aspects. Lepr. Rev. 45(1974)121 -134.
8. Desikan, K. V. and Job, C. K. A review of postmortem findings in 37 cases of leprosy. Int. J. Lepr. 36(1968)32-44.
9. Goldschmidt, J. Die Lepra-auf Madeira. Leipzig: F. C. W. Fogcl, 1891. Quoted in Deutsche Med. Wchnschr. 25(1899)200.
10. Kaldany, R.-R. J., Maasiio, K., Oiiman, R., Reitz-Vick, D., Britton, S. and Lefford, M. J. Methods for the detection of a specific Mycobacterium leprae antigen in the urine of leprosy patients. Scand. J. Immunol. 25(1987)37-43.
11. Kaldany, R.-R. J. and Nurlign, A. Development of a dot-ELISA for detection of leprosy an-tigenuria under field conditions. Lepr. Rev. 57 Suppl. 2(1986)95-100.
12. Koch, R. Die Lepra Erkrankungen imkreise Me-mcl. Klin. Jahrbuch 6 (1897). Abstract in Baumgartens Jahresbericht 14(1897)428.
13. Mehta, L., Ridley, M. J. and Antia, N. H. Immunological factors in nasal mucosa of patients with leprosy - immunoperoxidase study. Indian J. Lepr. 57(1985)31 1-317.
14. Olcen, P., Harboe, M., Warndorff, T. and Be-lehu, A. Antigens of M. leprae and anti-.U. leprae antibodies in the urine of leprosy patients. Lepr. Rev. 54(1983)203-216.
15. Peter, K. S., Vijaykumar, T., Vasudevan, D. M., Leena Devi, K. R., Mathew, M. T. and Gopi-nath, T. Renal involvement in leprosy. Lepr. India 53(1981)163-178.
16. Ridley, D. S. and Jopling, W. H. Classification of leprosy according to immunity; a five-group system. Int. J. Lepr. 34(1966)255-273.
17. Runyon, E. H. Anonymous mycobacteria in pulmonary disease. Med. Clin. N. Am. 43(1959)273-290.
18. Singh, N. B. and Choudhary, A. Detection of leprosy antigenuria through dot-ELISA. Indian J. Lepr. 60(1988)526-529.
1. Ph.D., Scientist; Division of Microbiology, Central Drug Research Institute, Lucknow 226001, India.
2. M.Sc, Research Fellow (CSTR); Division of Microbiology, Central Drug Research Institute, Lucknow 226001, India.
3. M.Sc, Research Assistant, Division of Microbiology, Central Drug Research Institute, Lucknow 226001, India.
Received for publication on 30 June 1989.
Accepted for publication in revised form on 5 March 1991.