- Volume 60 , Number 3
- Page: 390–6
Maxillary antrum involvement in multibacillary leprosy: a radiologic, sinuscopic, and histologic assessment
ABSTRACT
Thirty patients having lepromatous leprosy (22 males, 8 females) and showing radiological involvement of the maxillary antrum were subjected to sinuscopy, biopsy, and histopathological examination. Radiological observations showed diffuse opacity in 33.3% of the sinuses, localized mucosal thickening in 28.6%, and generalized thickened mucosa in 38.1%. Sinuscopy revealed inflamed mucosa as the most common finding (40%), followed by ulcerative (26.7%) and granulomatous ( 10%) lesions of the mucosal lining. The mucosal thickening (localized or generalized) evident on radiology was always associated with granuloma formation and acid-fast bacilli in the histology. The presence of an external nasal deformity indicated a statistically significant chance of encountering mucosal involvement on sinuscopy and histopathology (p < 0.05). There was more chance of finding positive sinuscopic lesions in those patients with a bacterial index above 3 +.RÉSUMÉ
Trente patients présentant une lèpre lépromateuse (22 hommes et 8 femmes) et montrant une atteinte radiologique de l'antre maxillaire ont subi une sinuscopie, une biopsie, et un examen histopathologique. Les observations radiologiques ont montré une opacité diffuse dans 33.3% des sinus, un épaississement localisé de la muqueuse dans 28.6%, et un épaississement généralisé de la muqueuse dans 38.1%. La sinuscopie a montré une inflammation de la muqueuse comme observation la plus fréquence (40%), suivie par des lésions ulcéreuses (26.7%), et granulomateuses (10%) du revêtement muqueux. L'épaississement muqueux (localisé ou généralisé) évident à la radiologie était toujours associé à une formation granulomateuse et des bacilles acido-résistants à l'histologie. La présence d'une déformation nasale externe indiquait une probabilité statistiquement significative de rencontrer un envahissement muqueux à la sinuscopie et à l'histopathologie (p < 0.05). Il y avait plus de chances de trouver des lésions sinuscopiques positives chez les patients présent un index bactérien supérieur à 3 +.RESUMEN
Treinta pacientes con lepra lepromatosa (22 hombres y 8 mujeres) que mostraron alteraciones radiológicas del antrum maxilar, se sometieron a senoscopía, biopsia y examen histopathológico. Las observaciones radiológicas mostraron opacidad difusa en el 33.3% de los senos, engrosamiento mucosal localizado en el 28.6%, y engrosamiento mucosal generalizado en el 38.1%. La senoscopia reveló una mucosa inflamada en el 40% de los casos, lesiones ulcerativas en mucosa en el 26.7%, y lesiones granulomatosas en el 10%. El engrosamiento mucosal, localizado o generalizado, evidente por radiologia, estuvo siempre asociado con la formación de granulomas y la presencia de bacilos ácido resistentes en la histología. La presencia de alguna deformación nasal externa indicó una probabilidad estadísticamente significativa de encontrar alteraciones mucosales en la senoscopia y en la histopatología (p < 0.05). Hubieron más probabilidades de encontrar lesiones senoscopicas en aquellos pacientes con un índice bacteriano mayor de 3 +.Leprosy primarily aflccts the peripheral nerves and skin. The other tissues afected are the mucous membrane of the upper respiratory tract, the anterior chamber of the eye and the testis, especially in the multibacillary forms of the disease. Involvement of the upper respiratory tract has been well documented in various autopsy series (8,9) and during life (5). Leprosy affects the mucosa of the nose, nasopharynx, and larynx. Leprous infiltration of the mucosa is characterized by the accumulation of histiocytes containing large numbers of leprosy bacilli.
Inadequate and ill-planned studies have been carried out regarding the involvement of the paranasal sinuses in leprosy. A detailed study of this aspect of leprosy is important since involvement of the paranasal sinuses may act as a reservoir of infection, as is known to occur in other forms of rhinitis, and this is of immense epidemiological importance. Involvement of the paranasal sinuses and the ensuing destruction contributes to unsightly deformities of the nose and part of the face in leprosy leading to social stigma and is important from a rehabilitation point of view. The present study was undertaken to ascertain involvement of the maxillary antrum in multibacillary leprosy by radiology, sinuscopy and histology, and to correlate the clinical, radiological and histological findings with direct sinuscopy.
MATERIALS AND METHODS
Seventy consecutive lepromatous leprosy patients attending the Leprosy Clinic of the Department of Dermatology attached to the Nehru Hospital, Postgraduate Institute of Medical Education and Research, Chandigarh, India, were recruited for this study. Diagnosis was based on clinical examination, slit-skin smear for Mycobacterium leprae from six sites, and a skin biopsy. The Ridley-Jopling classification (10) of leprosy was followed.
All patients had X-rays of the paranasal sinuses (Water's view) to look for involvement of the maxillary antrum in the form of haziness, fluid level, or thickened antral mucosa. Thirty patients with radiological abnormalities were subjected to complete otorhinolaryngological examination and maxillary antrum sinuscopy after obtaining informed consent.
The maxillary antrum was approached by the canine fossa route. The procedure was performed with the patient in a semirecumbent position. A biopsy was taken from the maxillary sinus mucosa by sinus endoscopy. The sinuscopic examination was performed using 70º and 30º Storz sinuscopes. The biopsy was taken from apparently abnormal mucosa showing ulceration, nodularity, and granuloma. The biopsy material was subjected to histopathological examination following hematoxylin and eosin (H&E) and Ziehl-Neelsen (ZN) staining for acid-fact bacilli (AFB).
RESULTS
The present report is confined to data from 30 patients with radiological abnormality in the maxillary antrum who were subjected to sinus endoscopy and histopathology; 22 (73.3%) males, 8 (26.7%) females. All of the patients had lepromatous leprosy (LL) with a mean bacterial index (BI) of 4+ and a morphological index (MI) of 4%. At the time of recruitment into the study, the symptoms were of 2-3 years' duration; most patients (50%) had symptoms of more than 3 years' duration. The commonest nasal complaint was crusting in 23 patients (76.7%) followed by obstruction in 16 patients (53.5%), epistaxis in 12 patients (40%), and anosmia in 11 (36.7%) patients.
Twenty patients (66.7%) had external nasal pyramid deformity. The nasal cavity findings are summarized in Table 1. The commonest finding was mucosal ulceration in 18 (60%) patients. Septal perforation was present in 6 (20%) patients.
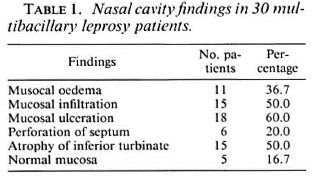
Eighteen patients (60%) had unilateral radiological involvement of the maxillary antrum, while 12 patients (40%) had bilateral involvement. The most common radiological change was mucosal thickening in 28 (66.7%) patients (Fig. 1) followed by diffuse opacity in 14 (33.3%) patients (Fig. 2).The mucosal thickening was localized in 12 (28.6%) patients, and generalized in 16 (38.1%) patients (Table 2).

Fig 1. Right side localized opacity of maxillary antrum.

Fig 2. Bilateral haziness of maxillary antra.
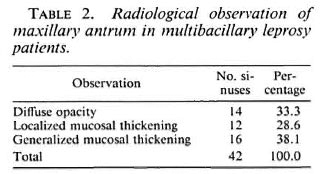
The Sinus endoscopy showed inflamed mucosa in 40%, frank mucosa ulceration in 26.7%, and granular mucosa in 10% of the patients. However, in 23.3% the mucosa was normal (Fig. 3 A, B, C). The biopsy material showed involvement of the antral mucosa in 21 patient (70%), with diffuse infiltration of mucosa by foam cells and AFB (Fig. 4). Similar changes were seen in the nasal biopsies in 90% of the patients. There was close correlation in the sinuscopic observations of antral mucosa and histopathological findings (Table 3).
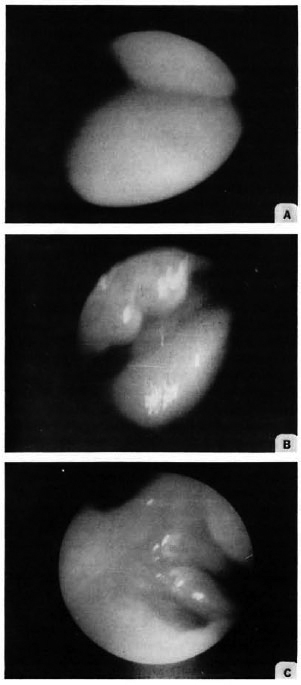
Fig. 3. Appearance of antral mucosa at maxillary sinuscopy. A = normal mucosa; B = granular mucosa; C = mucosal ulceration.
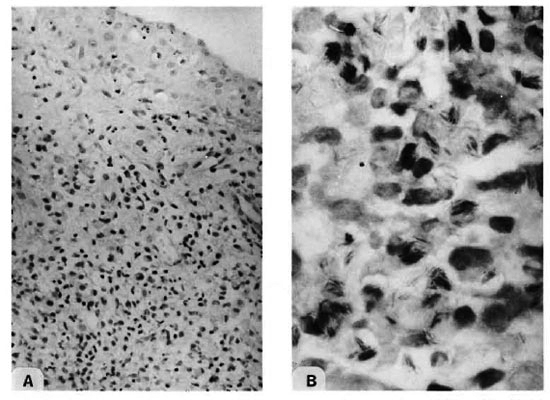
Fig. 4. Photomicrographs of antral mucosa showing (A) macrophage granuloma (H&E × 100) with (B) acid-fast bacilli (Fite-Faraco × 1000).
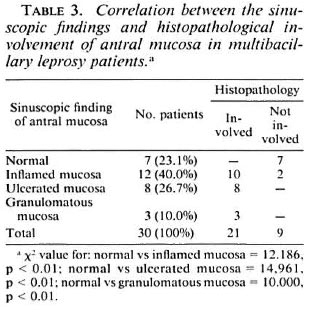
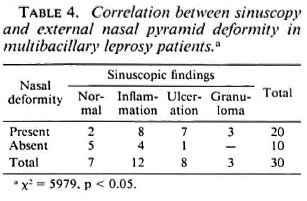
Good correlation was seen in sinuscopic abnormalities and external nasal deformity. All patients with evidence of granuloma in the sinus had nasal deformity (p < 0.05) (Table 4).
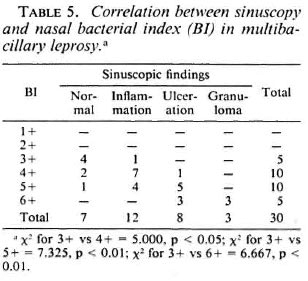
Patients having an average BI above 3 + invariably had sinuscopic involvement of the antral mucosa (Table 5).
DISCUSSION
Involvement of the upper respiratory tract in multibacillary leprosy is well known. Leprosy affects the mucosa of the nose, turbinates, nasopharynx, and larynx (12). AFB have occasionally been demonstrated from bronchial secretions and involvement of the buccal mucosa, palate, tongue, and gums has been demonstrated (5,6). Involvement of the paranasal sinuses, especially the maxillary antrum, is expected because of its continuity with the nasal mucosa, but this has been scantily documented (4,11,12).
In our study, a male preponderance (73.3%) (22) over female patients (26.7%) (8) was noted. Miller (7) also reported similar findings (male: female ratio = 2:1).
Around three fourths (86.7%) of our patients were between the ages of 20 and 40 years (13.3% of our patients were in their twenties). Soni (12) also reported similar findings. Miller (7) found 20% of his cases occurring in children under 10 years of age.
Mucosal ulceration was the most common finding (60%) in the nasal cavity, followed by mucosal infiltration (50%), and mucosal edema (36.7%). Atrophic changes were seen in 50% of the patients; septal perforation was noted in 20%. Normal mucosa was found in 16.7% of the cases. Barton (1,2) found that over 95% of the patients with lepromatous leprosy have involvement of the nasal mucosa, and all of the features noted in the present study have been documented by him.
Soni (11), in a radiological study of the paranasal sinuses in lepromatous leprosy, showed that 18 (60%) out of 30 patients had involvement of the maxillary sinus of which 7 (38.9%) were bilateral and 11 (61.1%) were unilateral. However, Barton (3), in a study of 16 patients with untreated lepromatous leprosy, found radiological abnormality in 100% of the cases.
We found that mucosal thickening was the commonest radiological abnormality (66.7%) with 16 sinuses showing generalized mucosal thickening and 12 others showing localized mucosal thickening in the form of patchy opacity. Diffuse opacity was observed in the remaining sinuses (33.3%). Barton and McDougall (4) also reported mucosal thickening of the maxillary antrum as the most constant radiological abnormality.
Maxillary sinuscopy revealed inflamed mucosa to be the most common abnormality (40%), while in 26.7% the mucosa showed ulceration and in 10% the mucosa was granulomatous. Normal mucosa was encountered in 7 cases (23.3%). Soni (12), in an antroscopic study of the maxillary antrum in 12 lepromatous leprosy patients, observed similar findings.
The mucosa biopsies at sinuscopy subjected to histopathological examination were positive for AFB in 21 cases (70%) in the present study, while in the remaining 9 (30%) patients sinus mucosa biopsies were negative for AFB and granuloma. Soni (12) performed sinus mucosal biopsy at antroscopy only in patients whose mucosa was visibly abnormal and found a positive biopsy in all nine cases. Barton (3) performed sinus mucosal biopsy in two patients and found histopathological involvement with AFB.
We noted that 66.6% (20) of the patients had a deformed external nasal pyramid; whereas Barton (2) observed nasal deformity in 47.4% of the patients in his series. The presence of clinical nasal deformity was associated with a significant chance of encountering abnormal sinus mucosa [90% in patients with nasal deformity as compared to 50% in those with external nasal deformity (p < 0.05)].
The nasal mucous membrane is involved in over 95% of lepromatous leprosy patients. In view of such high incidence associated with a highly infectious discharge, there is an increased possibility of the spread of leprosy from the maxillary antrum with the maxillary sinuses being frequently affected (70% in the present study). The surface area of the antral mucous membrane is estimated to be between 67 and 200 sq. cm. (4) and a constant flow of secretion may contribute significantly to the shedding of Mycobacterium leprae into the nose and thence into the environment. The involvement of paranasal sinuses in leprosy patients may take a long time to respond to antileprosy therapy, and a constant re-infection of the nose from the maxillary antrum may occur. It would be interesting to further observe the paranasal sinuses and noses of those patients in our present study after completion of their antileprosy treatment.
REFERENCES
1. BARTON, R. P. E. A clinical study of the nose in lepromatous leprosy. Lepr. Rev. 45(1974)135-144.
2. BARTON, R. P. E. Clinical manifestations of leprous rhinitis. Ann. Otol. Rhinol. Laryngol. 85(1976)74-82.
3. BARTON. R. P. E. Radiological changes in the paranasal sinus in lepromatous leprosy. J. Laryngol. Otol. 93(1979)597-600.
4. BARTON, R. P. E. and MCDOUGALL, A. C. The paranasal sinuses in lepromatous leprosy. Lepr. India 51(1979)481-485.
5. KAUR. S., KUMAR, B., MALIK, S. K., SINGH, M. P. and CHAKRAVARTY, R. N. Respiratory system involvement in leprosy. Int. J. Lepr. 47(1978)18-24.
6. KUMAR, B., YANDE, R., KAUR, I., MANN, S. B. S. and KAUR. S. Involvement of palate and cheek in leprosy. Indian J. Lepr. 60(1988)280-284.
7. MILLER, R. A. Leprosy (Hansen's disease). In: Harrison's Principles of Internal Medicine. Braunwald, E., Isselbacker, K. J., Petersdorf, R. G., Wilson, J. D., Martin, J. B. and Fauci, A. A., eds. 11th edn. New York: McGraw-Hill Book Company, 1987. p. 633.
8. MITSUDA. K. and OGAWA, M. A study of 150 autopsies of cases of leprosy. Int. J. Lepr. 5(1937)53-60.
9. POWELL, C. and SURANIN. L. Pathological changes observed in 50 necropsies. Am. J. Pathol. 31(1955)1131-1 147.
10. RIDLEY, D. S. and JOPLING, W. H. Classification of leprosy according to immunity; a five-group system. Int. J. Lepr. 34(1966)255-273.
11. SONI. N. K. Radiological study of the paranasal sinus in lepromatous leprosy. Indian J. Lepr. 60(1988)285-289.
12. SONI, N. K. Antroscopic study of the maxillary antrum in lepromatous leprosy. J. Laryngol. Otol. 103(1989)502-503.
1. M.S., Senior Resident.
2. M.S., M.N.A.M.S., Additional Professor.
5. M.S., Dip. N.B.E., Pool Officer, Department of Otorhinolaryngology.
3. M.D., Assistant Professor;
4. M.D., F.A.M.S., Professor and Head, Department of Dermatology.
6. M.D., Assistant Professor, Department of Pathology,
Postgraduate Institute of Medical Education and Research, Chandigarh 160012, India.
Reprint requests to Dr. Sharma.
Received for publication on 20 Mareh 1992.
Accepted for publication on 8 May 1992.