- Volume 60 , Number 3
- Page: 416–20
Chemoprophylaxis of leprosy with a single dose of 25 mg per kg rifampin in the southern marquesas; results after four years
ABSTRACT
In January-February 1988, a program of chemoprophylaxis for leprosy, using a single 25 mg/kg dose of rifampin, was conducted among 2786 (98.7%) inhabitants of the Southern Marquesas and 3144 South Marqucsan "emigrants" and their families. Among the treated population, during the 4 years which followed the implementation of the program, two leprosy patients were detected, one of whom can be considered as a failure of chemoprophylaxis because she was not known by the leprosy control unit. During the same period (1988-1991), a decrease in detection rates for leprosy in the entire French Polynesian population has been observed, an event which makes the interpretation of these findings very difficult. Nevertheless, according to presently available data, the effectiveness of chemoprophylaxis with a single dose of 25 mg/kg rifampin is estimated to be about 40% to 50%. When considering not only the results of the present study but also the financial and logistic constraints raised by such a program, one is led to the conclusion that chemoprophylaxis, even with a single dose of rifampin, is not likely to become an effective component of leprosy control programs.RÉSUMÉ
En janvier-février 1988, un programme de chimioprophylaxie de la lèpre, utilisant une dose unique de rifampicine de 25 mg/kg, a été réalisée parmi 2786 (98.7%) habitants des îles Marquises du Sud, et 3144 emigrants des Marquises du Sud et leur famille. Parmi la population traitée, 2 malades de la lèpre ont été détectés durant les 4 ans qui ont suivi la réalisation du programme; parmi ceux-ci l'un peut être considéré comme un échec de la chimioprophylaxic paree que la patiente n'était pas connue de l'unité de lutte contre la lèpre. Durant la même période (1988-1991), une diminution des taux de détection de la lèpre a été observée dans l'ensemble de la population de la Polynésie Française, ce qui rend très difficile l'interprétation de ces observations. Néanmoins, en se basant sur les données disponibles actuellement, l'efficacité de la chimioprophylaxic avec une dose unique de rifampicine à 25 mg/ kg est estimée à environ 40 à 50%. En considérant non seulement les résultats de l'étude présente mais aussi les implications financières et logistiques d'un tel programme, on arrive à la conclusion que la chimioprophylaxic. même avec une dose unique de rifampicine, est peu susceptible de devenir un composant effectif des programmes de lutte contre la lèpre.RESUMEN
En enero-febrero de 1988 se efectuó un programa de quimioprofilaxis de la lepra, usando una sola dosis de 25 mg/kg de rifampina, en 2786 (98.7%) habitantes de las islas Marquesas del Sur y en 3144 emigrantes de esas islas. Durante los 4 años siguientes a la implementación de programa, se detectaron 2 casos de lepra entre la población tratada, uno de los cuales podría considerarse como una falla del programa de quimioprofilaxis ya que este caso no era conocido en la unidad de control. Por otro lado, durante el mismo periodo (1988-1991) también se había observado una disminución en los índices de detección de la lepra en toda la Polinesia francesa, evento que hace difícil la interpretación de los resultados. No obstante, de acuerdo a los datos actualmente existentes, se calcula que la efectividad de la quimioprofilaxis con una sola dosis de rifampina (25 mg/kg) es del 40 al 50%. Considerando no solo los resultados del estudio, sino también las dificultades logísticas y financieras del programa, se llega a la conclusión de que este programa de quimioprofilaxis, con una sola dosis de rifampina, tiene pocas posibilidades de llegar a ser un componente efectivo de los programas de control de la lepra.Since the early 1950s, when dapsonc became the first available and uniquely active drug against Mycobacterium leprae, the question of the efficacy of chemoprophylaxis and of its possible role in leprosy control has remained a critical issue. The results of several studies conducted in India and Micronesia(7,8,11,12) have indicated that chemoprophylaxis with dapsone, given over long periods of time, would not likely result in a reduction in the incidence of leprosy, unless it could be administered to entire populations in endemic areas, and combined with adequate treatment of all known leprosy patients. Because rifampin has been demonstrated to be very active against M. leprae (5,6,10,13-16) , a chemoprophylaxis program for leprosy, utilizing a supervised single dose of 25 mg/kg of rifampin, was conducted in January-February 1988 (2) in the Southern Marquesas islands, a remote area of French Polynesia where the population is of limited size and where detection rates for leprosy have been very high for several decades (1). The aim of this paper is to report the results of the program 4 years after its implementation, and to assess whether any conclusion(s) may be drawn concerning the possible use of such a chemoprophylactic strategy.
MATERIALS AND METHODS
Material. The Marquesas arehipelago is located some 1500 kms northwest of Tahiti, the main island of French Polynesia (2). The three southernmost islands of that arehipelago are called the Southern Marquesas, the population of which was determined to be 2786 inhabitants in 1988. In such a small population, between 1967 and 1987, the average annual detection rate for leprosy was 48.9 per 100,000 (nearly two patients per year), while it was 8.6 for all of French Polynesia (1).
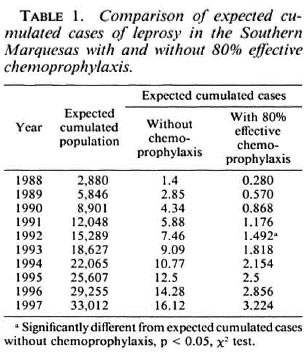
Methods. In 1987, an epidemiomctric projection model based on cases of leprosy detected during the preceding 20 years was established; it indicated what could be expected, in the Southern Marquesas, from a chemoprophylaxis program with cither 80%, 90% or 99% effectiveness. As reported below, one case of leprosy was discovered in the treated population between 1988 and 1991, and the effectiveness of the chemoprophylaxis program was lower than 90%. Therefore, in the present paper, the reduction in the number of expected cases with 80% effective chemoprophylaxis only is shown in Table 1.
Between January 18 and February 20, 1988, two teams (each with one medical doctor, one nurse, and one health worker from the leprosy control unit, supplemented with a South Marquesan health worker) carried out the program using a pre-established, computerized list of the South Marquesan population. The list was edited by island, valley, and village and also provided for every person the family name, given names, sex, and date of birth. Each inhabitant was identified by the local health worker, then weighed and given a supervised dose of 25 mg/kg of rifampin (capsules for adults and syrup for children).
During the 4-year post-chemoprophylaxis period (1988-1991), the follow up of the treated population was insured by the staff of the leprosy control unit in Tahiti, in collaboration with the personnel of the Public Health Service in the Southern Marquesas. Each treated person suspected to be a possible new leprosy patient by the local Marquesan health worker living in the village, valley, or island was referred for initial examination to the Public Health medical doctor responsible for the Southern Marquesas. Subsequently, if necessary, the patient was sent to Tahiti, where at the Institut Malarde a complete assessment was performed which included clinical examination of the skin and large nerve trunks, supplemented by the following biological tests: the seareh for acid-fast bacilli (AFB) in the nasal mucosa and the skin (carlobes and skin lesions), and biopsy for histopathological examination.
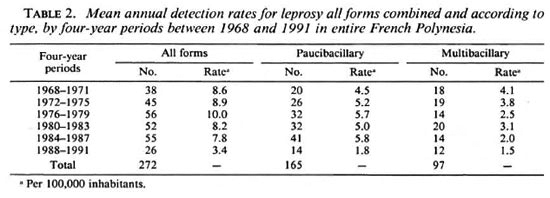
Detection rates for all forms of leprosy, according to type, were also calculated for the entire population of French Polynesia between 1968 and 1991 by 4-year periods (Table 2).
RESULTS
Coverage of the program. Between January and February 1988, the entire chemoprophylaxis program was implemented in 4 weeks: of the 2786 inhabitants, 2751 (98.7%) participated in the program and were given a single supervised dose of 25 mg/kg rifampin. In addition, 3144 persons were also given chemoprophylaxis, mainly in the Northern Marquesas and Society arehipelago because they were born in the Southern Marquesas (678) or were members of a family from the Southern Marquesas (2466).
Incidence of leprosy in treated population. By June 1988, a skin lesion was observed in an 11-year-old boy, the son of a South Marquesan living in Tahiti, who had been given chemoprophylaxis in February 1988. The lesion was a large, infiltrated patch located on the back part of the right arm. The seareh for AFB was positive in the lesion (4 + ) and in the nasal mucosa (4 + ) and negative in the carlobes; no solid-staining bacilli were found. The conclusions of the histological examination were: borderline (BB-BL) leprosy, presence of AFI3 (2+).
In October 1989, a skin lesion was discovered in a 7-year-old girl, living in one of the Southern Marquesas islands, who had been given chemoprophylaxis 21 months before (in January 1988). The lesion was a large, discolored, noninfiltrated patch located on the back part of the left leg. A slight sensory loss was noted at the site of the lesion. The seareh for AFB was negative in the skin lesion, in the nasal mucosa, and in the earlobes. Conclusions of the histological examination were: nonspecific dermatitis, compatible with indeterminate leprosy. Then, a nerve biopsy (external saphenous) was performed, and the findings of the histological examination were tuberculoid leprosy neuritis.
Incidence of leprosy in nontreated population. In Mareh 1990, lepromatous (LL) leprosy was detected in a 24-year-old woman who was born in the Southern Marquesas but who had been living in Tahiti for more than 10 years. During that period, she had been frequently in contact with her South Marquesan family who stayed at her home when coming to Tahiti. Because she was not known as a South Marquesan "emigrant," she had not been given chemoprophylaxis.
As shown in Table 2, the mean annual detection rate for leprosy in the entire French Polynesia, which had remained stable between 1968 and 1987 (about 8 per 100,000), decreased some 4% during the 4-year period 1988-1991. This decrease, which could be due, among other factors, to the implementation of multidrug therapy for all known leprosy patients in 1982 (3), was observed in a population not given chemoprophylaxis.
DISCUSSION
The onset of two cases of leprosy among the treated population raises the question of the effectiveness of the prophylaxis with 25 mg/kg rifampin. As previously discussed (2), the discovery in the 11-year-old boy of a borderline leprosy lesion located at the very same site as a preceding discolored patch, which appeared 9 months and disappeared 6 months before chemoprophylaxis, led us to the assumption that the boy was a missed case of leprosy and not a failure of chemoprophylaxis. With respect to the young girl, in whom a lesion of tuberculoid leprosy was discovered 21 months after the intake of the single dose of 25 mg/ kg rifampin, the data obtained by questioning the family did not permit us to determine with certainty whether a lesion was present at the moment she was given chemoprophylaxis. Nevertheless, from what is known about the incubation time of leprosy (9), one may assume that when she was treated the girl was very likely already infected by M. leprae. Therefore, at least in this one case, the intake of a single dose of 25 mg/ kg of rifampin was not capable of preventing the multiplication of M. leprae, nor the evolution toward overt disease. Finally, the detection of lepromatous leprosy in a young South Marqucsan woman who was not known by the leprosy control unit and, thus, was not given chemoprophylaxis, demonstrates clearly that even when important financial resources are available (the cost of the trial and follow up was over US$60,000) and a carefully designed and prepared program of chemoprophylaxis is applied, treatment of the entire eligible population cannot be guaranteed.
From the findings reported above, 4 years after the implementation of the program (February 1992), one single case of leprosy (7-year-old girl) has to be considered as a failure of chemoprophylaxis. When looking at Table 1, one may think that no significant result can be expected before 1992 since, by the end of 1991, a theoretical 1.176 cases of leprosy are expected (with 80% effective chemoprophylaxis), a number not significantly different from the theoretical 5.88 cases expected without chemoprophylaxis. In fact, we observed only one case, a number significantly lower (p < 0.05) than 5.88. Therefore, it could be estimated that the effectiveness of our program was at least 80%. This would be true if the assumption, made before the implementation of the trial, that no change in detection rates for leprosy would occur without chemoprophylaxis, were also true. This was not the case, and the interpretation of our findings has become much more difficult, if not impossible. Since the decrease in detection rates for leprosy was about 50% in the population not treated (with a single dose of rifampin), one may infer that, for at least one half, the decrease in detection rates observed in the South Marquesan population was not due to our chemoprophylaxis program. Hence, at best, in the present epidemiological situation, the effectiveness of chemoprophylaxis with 25 mg/kg of rifampin might be estimated to be 40% to 50%. If no new cases of leprosy are detected in the South Marqucsan population during the next 2 years (1992 and 1993), then the effectiveness of chemoprophylaxis will possibly be higher than 50%.
Our present results are preliminary and do not permit definitive conclusions. Nevertheless, some clear statements may be made at this time. Firstly, it should be kept in mind that, to date, the effectiveness of chemoprophylaxis for leprosy (with cither rifampin or dapsone) is still under investigation. Secondly, a most important point is that there is no justification to use chemoprophylaxis if all of the known leprosy patients are not receiving the most effective treatment. Thirdly, to be effective, a chemoprophylaxis program needs to be applied on a mass scale, and what we know about prophylactic mass treatments, either for leprosy or other mycobacterial diseases (4), suggests that chemoprophylaxis programs never provide entirely satisfactory results because of their high cost, the poor cooperation from the population, and the possible reinfection due to "old" relapsing patients (11,12). Finally, when considering the possible impact of multidrug therapy (given to all patients with active disease, but also to those considered as inactive and still under dapsone monotherapy) on the evolution of the leprosy situation (3), there is even less justification for considering chemoprophylaxis as an effective component of leprosy control programs.
Acknowledgment. This investigation received financial support from the UNDP/World Bank/WHO Special Programme for Research and Training in Tropical diseases and from the following II.EP organizations: Fondations Raoul Follereau (France), Leprosy Trust Board (New Zealand), and Oeuvres Hospitalières Françaises de l'Ordre de Malte (France). We are indebted to the stall" of the Public Health Service in the Marquesas Islands for their assistance in the field, especially Dr. J.-C. Genetic, P. Richez and D. Hebral; Mrs. V. Matuaiti, D. Schlegel, and M. L. Tetahiotupa, and Mr. F. Vaatete and D. Ah Lo.
REFERENCES
1. CARTEL, J-L., BOUTIN, J-P., PLICHART, R., ROUX, J. and GROSSET, J-H. La lèpre dans les arehipels de Polynésie Française de 1967 à 1987. Bull. Soc. Pathol. Exot. Filiales 81(1988)819-826.
2. CARTEL, J-L., CHANTEAU, S., BOUTIN, J-P., PLICHART, R., Roux, J. and GROSSET, J-H. The implementation of chemoprophylaxis of leprosy in Southern Marquesas with a single dose of 25 mg per kg rifampin. Int. J. Lepr. 57(1989)810-816.
3. CARTEL, J-L., SPIEGEL, A., NGUYEN NGOC, L., MOULIA-PELAT. J-P. and GROSSET, J-H. Leprosy in French Polynesia; The possible impact of multidrug therapy on epidemiological trends. Lepr. Rev. (1992).
4. FEREBEE, S. H. Controlled chemoprophylaxis trials in tuberculosis, a general review. Adv. Tuberc. Res. 17(1969)28-106.
5. GROSSET, J-H. Recent developments in the field of multidrug therapy and future Research in chemotherapy of leprosy. Lepr. Rev. 57 Suppl. 3(1986)223-234.
6. LEVY, L., SHEPARD, C. C. and FASAL, P. The bactericidal effect of rifampicin on M. leprae in man: a) single doses of 600, 900 and 1200 mg; and b) daily doses of 300 mg. Int. J. Lepr. 44(1976)183-187.
7. NOORDEEN, S. K. Chemoprophylaxis in leprosy. Lepr. India 40(1968)115-119.
8. NOORDEEN, S. K. Long-term effects of chemoprophylaxis among contacts of lepromatous cases. Lepr. India 49(1977)504-509.
9. NOORDEEN, S. K. The epidemiology of leprosy. In: Leprosy. Hastings, R. C., ed. London: Churchill Livingstone, 1985, pp. 15-30.
10. REE.S, R. W. J. The contribution of Charles C. Shepard to leprosy Research: from the mouse footpad model to new DNA technology. Symposium on the immunology of leprosy, Oslo. Norway, 1986. Lepr. Rev. 57 Suppl. 2(1986)1-14.
11. RUSSELL, D. A.. WORTH, R. M., JANO, B., FASAL, P. and SHEPARD, C. C. Acedapsone in the prevention of leprosy; field trial in three high prevalence villages in Micronesia. Am. J. Trop. Med. Hyg. 28(1979)559-563.
12. RUSSELL, D. A., WORTH, R. M., SCOTTE, G. C, VINCIN, D. R., JANO, B., FASAL, P. and SHEPARD, C. C. Experience with accdapsone (DADDS) in the therapeutic trial in New Guinea and the chemoprophylactic trial in Micronesia. Int. J. Lepr. 44(1976)170-176.
13. SHEPARD, C. C. A survey of the drugs with activity against M. leprae in mice. Int. J. Lepr. 39(1971) 340-346.
14. SHEPARD, C. C. Recent developments in the chemotherapy and chemoprophylaxis of leprosy. Leprologica (Argent.) 19(1974)230-236.
15. SHEPARD. C. C. LEVY. L. and FASAL, P. Further experience with the rapid bactericidal effect of rifampin on Mycobacterium leprae. Am. J. Trop. Med. Hyg. 23(1974)1120-1124.
16. SUBCOMMITTEE ON CLINICAL TRIALS OF THE CHEMOTHERAPY OF LEPROSY (THELEP) SCIENTIFIC WORKING GROUP OF THE UNDP/WORLD BANK/ WHO SPECIAL PROGRAMME FOR Research AND TRAINING IN TROPICAL DISEASES. Thelep controlled trials in lepromatous leprosy. Lepr. Rev. 54(1983)167-173.
1. M.D.; Institut Territorial de Recherches Médicales Louis Malarde, B. P. 30, Papeete, Tahiti, Polynésie Francaise. 2. S. Chanteau, Ph.D.; Institut Territorial de Recherches Medicales Louis Malarde, B. P. 30, Papeete, Tahiti, Polynesie Francaise.
3. M. D.; Institut Territorial de Recherches Medicales Louis Malarde, B. P. 30, Papeete, Tahiti, Polynesie Francaise.
4. Computer Scientist; Institut Territorial de Recherches Medicales Louis Malarde, B. P. 30, Papeete, Tahiti, Polynesie Francaise.
5. M.D.; Institut Territorial de Recherches Medicales Louis Malarde, B. P. 30, Papeete, Tahiti, Polynesie Francaise.
6. M.D.; Institut Territorial de Recherches Medicales Louis Malarde, B. P. 30, Papeete, Tahiti, Polynesie Francaise.
7. M.D., Professor, Institut Territorial de Recherches Medicales Louis Malarde, B. P. 30, Papeete, Tahiti, Polynesie Francaise.
8. M.D., Professor, Faculte de Medecine Pitie-Salpetriere, 91 Blvd. de l'Hopital, 75634 Paris 13, France.
Reprint requests to Dr. J.-L. Cartel, Director, Institut de Leprologie Appliquée, B.P. 11023, Dakar CD, Senegal.
Received for publication on 19 February 1992.
Accepted for publication on 12 May 1992.