- Volume 60 , Number 1
- Page: 1–7
Assessment of the diagnostic value of the native PGLTB1, its synthetic neoglycoconjugate PGLTB0 and the sulfolipid iv antigens for the serodiagnosis of tuberculosis
ABSTRACT
A major phenolic glycolipid (PGLTB1) f rom Mycobacterium tuberculosis, that resembles the phenolic glycolipid-I (PGL-I) f rom M. leprae, and its synthetic terminal diglycosyl conjugate (PGLTB0) were reported and raised the prospects of a specific sérodiagnostic test for tuberculosis (TB). The diagnostic use of a sulfolipid, namely the SLIV, was also reported. The objective of this investigation was to assess the relative sensitivity, specificity, and predictive values of three ELISAs using the PGLTB1, the PGLTB0, and the SLIV as antigens for the serodiagnosis of TB. Similarly to leprosy patients for the PGL-I antigen, the TB patients responded preferentially in IgM against the phenolic glycolipid. We screened the sera f rom 191 active tuberculous patients, 29 healthy subjects living in France, 102 healthy Polynesian blood donors, 82 contacts of new TB patients, and 20 leprosy patients before treatment for IgG anti-SLIV, and for IgM anti-PGLTB1 and IgM anti-PGLTB0. TB patients showed significantly higher activity than did healthy Polynesians when tested against SLIV and PGLTB0, and the smear-positive group gave higher activity than did the smear-negative but culturepositive group, especially for IgG anti-SLIV. The leprosy patients did not show higher activity than the Polynesian controls. Respectively, for SLIV, PGLTB1 and PGLTB0 antigens, the specificities were of 95%, 85%, and 89%; the sensitivities of 36%, 16% and 15%; the efficiencies of 58%, 40% and 39%; the predictive values for a positive result, assuming a prevalence of 15% among patients with respiratory symptoms, were of 30%, 16% and 19%.RÉSUMÉ
Un glycolipide phénolique majeur (PGLTB1) de Mycobacterium tuberculosis, qui ressemble au glycolipide phénolique-I (PGL-I) de M. leprae, et son conjugué diglycosyl terminal synthétique (PGLTB0) ont été mis en évidence et ont fait naître l'espoir de voir développer un test spécifique pour le sérodiagnostic de la tuberculose (TB). L'utilité diagnostique d'un sulfolipide, le SLIV, a également été rapportée. L'objectif de cette recherche était d'évaluer les sensibilité, spécificité et valeur prédictive de 3 ELISA utilisant le PGLTB1, le PGLTB0, et le SLIV comme antigènes pour le sérodiagnostic de la tuberculose. De même que l'antigène PGL-I pour les patients lépreux, les patients tuberculeux répondent de manière préférentielle par des IgM vis-à-vis du glycolipide phénolique. Nous avons testé les sérums en provenance de 191 patients présentant une tuberculose active, 29 personnes en bonne santé vivant en France, 102 donneurs de sang polynésiens en bonne santé, 82 contacts de nouveaux patients tuberculeux, et 20 patients lépreux avant traitement, pour la présence d'IgG vis-à-vis du SLIV, et pour la présence d'IgM vis-à-vis du PGLTB1 et du PGLTB0. Les patients tuberculeux ont montré une activité significativement plus importante que les polynésiens quand ils furent testés vis-à-vis du SLIV et du PGLTB0, et le groupe des personnes positives à l'examen direct montra une activité plus importante que les personnes négatives à l'examen direct mais positives à la culture, surtout pour les IgG anti-SLIV. Les patients lépreux n'ont pas montré une activité plus importante que les témoins polynésiens. Les spécificités étaient respectivement de 95%, 85%, et 89% visà-vis des antigènes SLIV, PGLTB1 et PGLTB0; les sensibilités étaient de 36%, 16% et 15%; les efficiences étaient de 58%, 40% et 39%; les valeurs prédictives pour un test positif, en supposant une prévalence de 15% parmi les patients présentant des symptômes respiratoires, étaient de 30%, 16% et 19%.RESUMEN
Previamente se ha reportado la existencia de un glicolípido fenólico del Mycobacterium tuberculosis (PGLTB1) y la preparación de un conjugado con su residuo glicosilico terminal sintético (PGLTB0). El PGLTB1 se semeja al glicolipido fenólico-I del .1/. leprae (PGL-I). También se ha reportado el uso del sulfolipido SLIV del .M. tuberculosis para el diagnóstico de la tuberculosis (TB). El objetivo de esta investigación fue el establecer la sensibilidad relativa, la especificidad y el valor predictive de tres ELISAs para el serodiagnóstico de TB. usando como antígenos el PGLTB1, el PGLTB0. y el SLIV. Al igual que los pacientes con lepra con el PGL-I, los pacientes con TB respondieron preferentemente con anticuerpos IgM contra el glicolipido fenólico. Se analizaron los sueros de 191 pacientes con TB activa, de 29 sujetos sanos habitantes de Francia, de 102 donadores de sangre polinesios, de 82 contactos de nuevos pacientes con TB. y de 20 pacientes con lepra sin tratamiento. Se buscaron las respuestas de IgG anti-SLIV. de IgM anti-PGLTB1. y de IgM ant-PGLTB0. Los pacientes TB mostraron una actividad significativamente mayor que los controles polinésios sanos cuando se probaron contra SLIV y contra PGLTB0. El grupo con baciloscopías positivas dio mayor reactividad que los pacientes con baciloscopías negativas pero con cultivos positivos, especialmente para IgG anti-SLIV. Los pacientes con lepra no mostraron mayor reactividad que los controles polinésios. Las especificidades respectivas para losanígenos SLIV, PGLTB1 y PGLTB0, fueron: 95%, 85%, y 89%; las sensibilidades: 36%, 16%, y 15%. y las eficiências: 58%, 40%, y 39%. Los valores predictivos de un resultado positivo, suponiendo una prevalência del 15% entre los pacientes con sintomas respiratórios, fueron del 30%, 16% y 19%, respectivamente.Despite effective treatment, tuberculosis (TB) remains a major scourge in the world. Mycobacterium tuberculosis is responsible for some ten million new cases and three million deaths per year. The situation is getting worse in most countries since the acquired immune deficiency syndrome (AIDS) is an important risk factor(13). For an effective control of this disease, a rapid, sensitive and low-cost diagnostic method to identify the new cases is still needed.
There are a large number of reports showing that antibody levels are significantly higher in patients as a group than in a control population. The report of a major triglycosyl phenol phthiocerol glycolipid in some strains of M. tuberculosis (7,8) that resembles the phenolic glycolipid-I (PGL-I) of M. leprae (11) raised the prospect of a specific serodiagnosis for tuberculosis, at least for the smear-positive patients, by analogy to what was known for multibacillary leprosy patients (3). In some preliminary studies, this PGLTB1 and a sulfolipid IV (SLIV) (5,10) were found to be reactive against a large proportion of the sera from tuberculosis (TB) patients (14,15). The synthesis of the terminal disaccharide of PGLTB1, namely, PGLTB0, was undertaken and this product was converted to a water-soluble neoglycoconjugate for use in ELISA (6).
The purpose of our study was to assess the relative sensitivity, specificity, efficiency, and predictive values of three ELISAs using PGLTB1, PGLTB0, or SLIV as antigen for the serodiagnosis of TB patients.
METHODS
Populations studied. The different groups of sera tested were: a) 191 Polynesian TB patients before treatment of whom 119 were smear-positive and 72 were smear-negative but culture-positive; b) 29 healthy subjects living in France and 102 healthy Polynesian blood donors as negative controls; c) 82 contacts of new TB patients; and d) 20 leprosy patients before treatment (11 multibacillary and 9 paucibacillary).
Antigens tested. The native PGLTB1 and the sulfolipid SLIV were kindly supplied by Professor H. L. David (Institut Pasteur, Paris, France) and the synthetic PGLTB0 conjugate, by Professor P. Brennan (Colorado State University, Fort Collins, Colorado, U.S.A.). The SLIV was coated at 250 ng/ well (ELISA microplate; CML, France) in hcxanc. The PGLTB1 was used at 100 ng/ well in hexane, and the PGLTB0 at 1 ng carbohydrate/well in carbonate buffer, pH 9.6. The plates were incubated overnight at 4ºC, and washed four times with PBS/BSA 0.1 % (1 % Tween 20 was added for the ELISA PGLTB0).
ELISA technique. The conventional indirect ELISA procedure for the detection of human IgG and IgM has been described elsewhere (2). After a preliminary study to define the optimum conditions to obtain the best discriminative results, the sera diluted in PBS with 10% normal goat serum were screened for IgG anti-SLIV at a 1/250 dilution; IgM anti-PGLTB1 and IgM anti-PGLTB0 each at a 1/100 dilution. Peroxidase-conjugated goat anti-human IgG (Biosys) or IgM (Cappel) was then added and incubated, and the substrate solution was H202-0-phenylenediamine. The reactions were stopped with H2SO4 2.5 N, and the optical density (OD) was read at 492 nm using an automatic ELISA reader (Titertek) connected to an IBM-compatible computer (Goupil G5). The specific activity expressed in OD was the difference in mean OD between the antigen-coated wells and the noncoated wells for each sera.
Statistical analysis. Statistical analysis was performed with the PCSM statistical package (Deltasoft) on an IBM-PC-compatible microcomputer. We used variance analysis and Student's / test to compare the OD among the difFercnt groups and standard regression analyses for the correlations between antigens.
The sensitivity in the proportion of patients with the disease who have a positive test and the specificity is the proportion of the nondiseased individuals with a negative test. The efficiency of the test is the percentage of individuals (diseased and nondiseased) correctly classified. The receiver operating curve (ROC), which is the trend of the couple sensitivity/specificity according to the cut-off defined, was represented for each antigen. The predictive value for a positive result (PVP) and the predictive value for a negative result (PVN) were calculated according to the Bayes' theorem.
RESULTS
Comparison of antibody activity among different groups of sera tested. The IgG anti-SLIV, IgM anti-PGLTB1, and IgM anti-PGLTB0 activity for the group of Polynesian negative controls and for the TB patients are shown in Figure 1. The mean values and respective standard deviations of the ELISA results for each group of sera tested are given in Table 1.
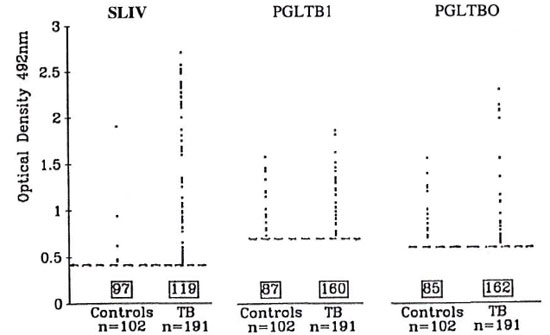
Fig. 1. Scattergrams of individual seroreactivity in controls and TB patients. Cut-offs were OD = 0.400 for SLIV; 0.700 for PGLTB1; 0.600 for PGLTB0.
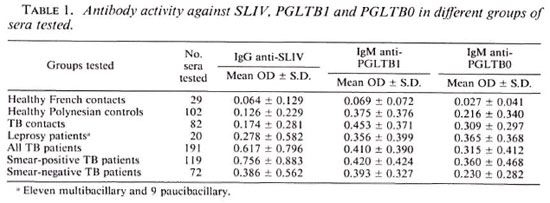
In order to assess the differences in mean ODs among groups for each antigen tested, we performed an analysis of variance which showed significant differences among groups for SLIV (F = 17.095, p < 10-4), PGLTB1 (F = 6.09, p < 10-4), and PGLTB0 (F = 5.014, p < 10-4). These findings allowed us to compare groups two by two, using the t test with residual variances. The results of this comparison for each of the three antigens tested are given in Table 2. Healthy Polynesians displayed significantly higher IgM anti-PGLTB1 and IgM anti-PGLTB0 than did healthy subjects living in France, and no correlation for a linear trend with age was found. The contacts of TB patients were not significantly different from healthy Polynesians for any of the three antigens tested. There was no difference between multibacillary and paucibacillary leprosy patients and, overall, leprosy patients did not display higher activity than healthy Polynesian controls.
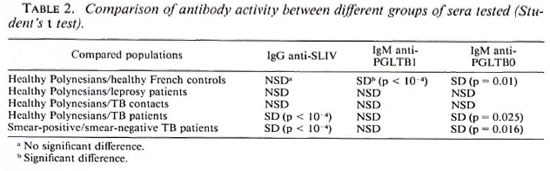
TB patients showed significantly higher activity than healthy Polynesians when tested against SLIV and PGLTB0. In those patients, the activity of the smear-positive group was significantly higher than the smear-negative group, especially for IgG anti-SLIV. The correlation between antibody titers in tuberculous patients was found to be significant between PGLTB1 and its synthetic analog PGLTB0 (r = 0.67, p < 10-4). On the other hand, IgG anti-SLIV titers were not correlated with IgM anti-PGLTB1 nor with IgM anti-PGLTB0.
Sensitivity, specificity, and predictive values. The diagnostic value of each test was assessed by the sensitivity, the specificity, and the predictive value of a positive result (PVP) and the predictive value of a negative result (PVN). These parameters depend on the cut-off chosen, which generally results from a compromise between desired sensitivity and specificity. Figure 2 shows the trend of sensitivity and specificity according to different cut-off points of the ELISA for each of the three antigens tested (ROC), using healthy Polynesians as a control group.

Fig. 2. Receiver operating curve representation for serodiagnosis of tuberculosis; trend of sensitivity and specificity for each antigen used according to cut-off of ELISA reaction. ■ = SLIV; ○ = PGLTB0; ● = PGLTB1 .
In order to reach an acceptable specificity, the cut-offs we retained were: OD = 0.400 for SLIV (specificity = 95%, sensitivity = 36%); OD = 0.700 for PGLTB1 (specificity = 85%, sensitivity = 16%) and OD = 0.600 for PGLTB0 (specificity = 89%, sensitivity = 15%). The efficiencies calculated respectively for SLIV, PGLTB1, and PGLTB0 were 58%, 40%, and 39%.
For each antigen, the predictive values for a positive or a negative result were calculated for an overall prevalence of TB in Polynesia (50/100,000) and for a prevalence of TB among individuals with respiratory symptoms (15%). The PVP and PVN for each antigen are shown in Table 3.
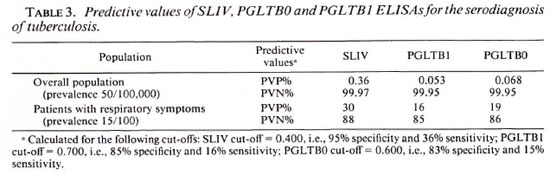
To improve the sensitivity of this serology, two tests-SLIV and PGLTB0-were combined because they are not correlated and PGLTB0 seems to be better than PGLTB1. A positive result was defined as a positive response to at least one of the two antigens. The sensitivity of the two tests combined increased to 47%, but the specificity decreased to 84%.
DISCUSSION
This work was conducted to evaluate the sensitivity, specificity, efficiency, predictive values, and correlations among three antigens (SLIV, PGLTB1, and PGLTB0) for the serodiagnosis of tuberculosis. Tuberculosis patients responded preferentially in IgM against PGLTB1 or its synthetic analog, similar to leprosy patients against M. leprae PGL-I (16). We found a good correlation between the native PGLTB1 and its synthetic analog (r = 0.67, p < 10-4), as previously reported by Daffe, et al. (6).
It is noteworthy that healthy Polynesian subjects gave higher ODs for PGLTB1 and PGLTB0 than did healthy subjects living in France. Such an observation was already noticed for the response to M. leprae PGL-I (1). This forced us to use Polynesian negative controls rather than French controls to establish the cut-offs and the specificities of the three tests for the diagnosis of Polynesian patients.
Most of the diagnostic tests overlap between results in those individuals with and without disease. This overlap is shown clearly in Figure 1 and by the mean OD values in Table 1. The smear-positive TB patients showed statistically higher antibody activity than did the smear-negative patients with SLIV and PGLTB0; this difference was not significant with native PGLTB1. Conversely to the big difference in seroreactivity between multibacillary and paucibacillary leprosy patients against the PGL-I antigen (3), the difference between smear-positive and smear-negative TB patients, although statistically significant, is small and this may explain the disagreement between the phenolic glycolipid and its synthetic glycoconjugate.
Each user has to define the appropriate cut-off point of the test according to the specificity and sensitivity needed. The trend of the ROC curves as seen in Figure 2 do not portend a future for any of the three tests for the serodiagnosis of tuberculosis. A cut-off was chosen however for each test and gave specificities of 95%, 85% and 89%, respectively, for SLIV, PGLTB1, and PGLTB0. The corresponding sensitivities were low: 36% for SLIV, 16% for PGLTB1, and 15% for PGLTB0. The proportion of well-categorized individuals for each test was not high enough for any of them to be considered a valuable diagnostic test (58% to 39%). Of the three ELISAs, the IgG anti-SLIV test has shown the best specificity and sensitivity. A previous report described a slightly better performance for the ELISA IgG anti-SLIV (sensitivity = 51%, specificity = 100%). Our results on the phenolic glycolipid do not support previous optimistic studies reporting excellent (> 90%) sensitivity and specificity (12,14). Other authors found similar disappointing results (sensitivity = 20%) (6). Some experimental findings may explain the difference in anti-PGLTB1 activity from patient to patient. The M. tuberculosis isolates from different parts of the world may or may not contain the specific PGLTB1, and this would affect the level of anti-glycolipid in the sera of patients. A further study to phenotype the M. tuberculosis isolates from Polynesia would be helpful to confirming this hypothesis.
For any preselected sensitivity and specificity, the significance of a positive or negative result is critically dependent on the prevalence of the disease in the population under study. With indiscriminate screening, even in very highly endemic areas, the predictive value for a positive result (PVP) would be very low for all three tests (< 1% for a prevalence of 50/100,000 in Polynesia). Thus, to achieve higher PVP values it is necessary to target the screening to the high-risk populations such as contacts or those with clinical symptoms. Assuming a prevalence of 15% among this latter group, the calculated PVP was 30% for SLIV, 16% for PGLTB1, and 19% for PGLTB0. To be of use in the diagnosis of tuberculosis, serological methods have to be accurate when microscopic examination shows no bacilli or in extra-pulmonary tuberculosis. In our study, the smear-negative patients displayed significantly lower IgG anti-SLIV than smear-positive patients; the sensitivity in diagnosing the smear-negative patients was still very low (27%). We attempted to improve the quality of the serodiagnosis with the association of SLIV and PGLTB0. This association yielded a sensitivity of 50%.
In unusual clinical cases such as HIV- seropositive patients, this serology has to be evaluated since tuberculosis occurs very early in the course of AIDS when antibody responses are still intact or are only slightly reduced (9).
In conclusion, in contrast to the PGL-I antigen for the serodiagnosis of multibacillary leprosy patients, PGLTB1 or its synthetic analog were not effective for the serodiagnosis of TB patients. Among the three antigens tested, SLIV was found to be better than PGLTB1 and PGLTB0. However, despite a higher antibody response in TB patients than in controls, neither of these tests has potential value for clinical practice. Further research is still needed to identify new antigens which may provide a more specific and sensitive test for the serodiagnosis of TB.
Acknowledgment. We are most gratcful to Professor Hugo David and to Professor Patrick Brennan for providing the antigens for this study. We acknowledge Patrick Luquiaud and Catherine Plichart for their technical assistance.
REFERENCES
1. CHANTEAU. S., CARTEL, J. L., GUIDI, C, PLICHART, R. and BACH, M.-A. Seroepidemiological study on 724 household contacts of leprosy patients in French Polynesia using disaccharide-octyl-BSA as antigen. Int. J. Lepr. 55(1987)626-632.
2. CHANTEAU, S., CARTEL, J. L., Roux, J., PLICHART, R. and BACH, M.-A. Comparison of synthetic antigens for detecting antibodies to phenolic glycolipid I in patients with leprosy and their household contacts. J. Infect. Dis. 157(1988)770-776.
3. CHANTEAU, S.. CARTEL. J. L.. SPIEGEL. A., PLICHART, R. and Roux, J. [Detection of IgM anti-PGL-I for the serodiagnosis of leprosy and for the follow up of contact population in Polynesia. A 5 year situation.] Bull. Soc. Pathol. Exot. Filiales 83(1990)649-657.
4. CRUAUD. P., BERLIE. C, TORGAL-GARCIA. J.. PAPA. F. and DAVID, H. L. Human IgG antibodies immunoreacting with specific sulpholipids from Mycobacterium tuberculosis. Zentralbl. Bakteriol. 271(1989)481-485.
5. CRUAUD, P., YAMASHITA, J. T., MARTIN-CASABONA. N., PAPA, F. and DAVID, H. L. Evaluation of a novel 2,3-diacyltrehalose-2'-sulfate (SL-IV) antigen for case finding and diagnosis of leprosy and tuberculosis. Res. Microbiol. 141(1990)679-694.
6. DAFFÉ, M., CHO, S.-N., CHATTERJEE, D. and BRENNAN , P. Chemical synthesis and seroreactivity of a neoantigen containing the oligosaccharide hapten of the Mycobacterium tuberculosis specific phenolic glycolipid. J. Infect. Dis. 163(1991)161-168.
7. DAFFÉ, M., LACAVE, C, LANÉELLE, M. A. and LANÉELLE, G. Structure of major triglycosylphcnolphtioccrol of Mycobacterium tuberculosis (strain Canetti). Eur. J. Biochem. 167(1987)155-160.
8. DAFFÉ. M.. PAPA, F., LASZLO, A. and DAVID. H. L. Glycolipids of recent clinical isolates of Mycobacterium tuberculosis: clinical characterization and immunoreactivity. J. Gen. Microbiol. 135(1989)2759-2766.
9. DANIEL, T. M. Rapid diagnosis of tuberculosis; laboratory techniques applicable in developing countries. Rev. Infect. Dis. 11(1989)S471-S478.
10. GOREN. M. B., BROKE, O., ROLLER, P., FALES, H. M. and DAS. B. S. Sulfatides of Mycobacterium tuberculosis: the structure of the principal sulfatide (SLI). Biochemistry 15(1976)2728-2735.
11. HUNTER. S. W.. FUJIWARA, T. and BRENNAN, P. J. Structure and antigenicity of the major specific glycolipid antigen of M. leprae. J. Biol. Chem. 257(1982)15072-15078.
12. MARTIN-CASABONA. N., GONZALES-FUENTE, T., ARCALIS ARCE, L., OTAL ENTRAIGAS, J. and VIDAL PLA, R. Evaluation of a phenolglycolipid antigen (PGL-Tb 1) from M. tuberculosis in the serodiagnosis of tuberculosis: comparison with PPD antigen. Acta Leprol. (Geneve) 7 Suppl. 1(1989)89-93.
13. STYBLO, K. Overview and epidemiologic assessment of the current global tuberculosis situation with an emphasis on control in developing countries. Rev. Infect. Dis. 11(1989)S338-S346.
14. TORGAL-GARCIA. J., DAVID, H. L. and PAPA, F. Preliminary evaluation of Mycobacterium tuberculosis phenolglycolipid antigen in the serologic diagnosis of tuberculosis. Ann. Inst. Pasteur Microbiol. 139(1988)289-294.
15. TORGAL-GARCIA, J., PAPA. F. and DAVID, H. L. Immunological response to homologous and heterologous phenolic glycolipid antigens in tuberculosis and leprosy. Acta Leprol. (Geneve) 7 Suppl. 1(1989)102-106.
16. YOUNG, D. B., DISSANAYAKE, S., MILLER, R. A., KANOLKAR, S. R. and BUCHANAN, T. M. Humans respond predominantly with IgM immunoglobulin to the species-specific glycolipid of M. leprae .J. Infect. Dis. 149(1984)870-873.
1. Ph.D., Institut Territorial de Recherches Medicales Louis Malardé. B. P. 30, Papeete. French Polynesia.
2. M.D., Institut Territorial de Recherches Medicales Louis Malardé. B. P. 30, Papeete. French Polynesia.
3. M.D., Centre Hospitalier Territorial Mamao. Papeete. French Polynesia.
Received for publication on 13 May 1991.
Accepted for publication on 30 October 1991.