- Volume 59 , Number 1
- Page: 120–1
Vitiligo and lepromatous leprosy
This department is for the publication of informal communications that are of interest because they are informative and stimulating, and for the discussion of controversial matters. The mand ate of this JOURNAL is to disseminate information relating to leprosy in particular and also other mycobacterial diseases. Dissident comment or interpretation on published research is of course valid, but personality attacks on individuals would seem unnecessary. Political comments, valid or not, also are unwelcome. They might result in interference with the distribution of the JOURNALand thus interfere with its prime purpose.
To the Editor:
Vitiligo is an acquired pigmentary disorder of the skin characterized by the development of circumscribed, depigmented macules of variable sizes. It is often extremely disfiguring in dark-skinned individuals. It affects all races and occurs in 1% to 3% of a population. Frequent observation of vitiligo in patients with lepromatous leprosy prompted us to study the prevalence of vitiligo in these patients.
Among 400 patients (240 males, 160 females) with lepromatous leprosy seen by the author during the last 12 years, 48 were found to have vitiligo (Figs. 1 and 2), thus making a prevalence of 12%. Their ages varied from 12 years to 66 years (mean age 38 years). Vitiligo was present in 16 patients when the diagnosis of leprosy was made, and in the remaining patients it developed along with the signs and symptoms of type 2 lepra reaction following specific treatment. None of them gave a family history of vitiligo or other autoimmune disorders. The diagnosis of lepromatous leprosy was confirmed in all cases by demonstration of acid-fast bacilli in slit-skin and earlobe smears. Detailed clinical examinations and laboratory tests were done for all of these patients to exclude diabetes mellitus, collagen vascular diseases, thyroid disease, and Addison's disease; all were found to be normal. Among 1600 patients with nonlepromatous leprosy seen during the same period, only 32 had associated vitiligo, its prevalence being 2%. When 4000 (2000 males, 2000 females) healthy volunteers, who represented the general population in this area, were examined, vitiligo was observed in 88, making a prevalence of 2. 2%.
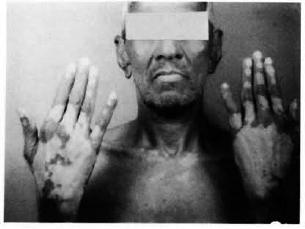
Fig. 1. Note depigmented macule of vitiligo in a patient with lepromatous leprosy. He has early clawing of medial fingers.
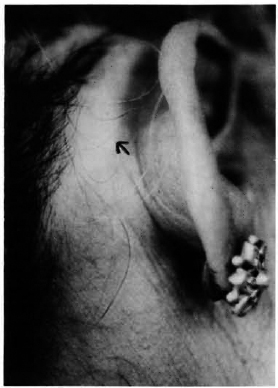
Fig. 2. Vitiligo of the scalp of a female patient. Note thickening of the rim of the earlobe due to Iepromatous leprosy.
The above study indicates that the prevalence of vitiligo is significantly more in lepromatous leprosy patients than in the general population and in patients with nonlepromatous leprosy. The clinical features of vitiligo are so characteristic that elaborate laboratory tests are seldom required for its diagnosis. The exact etiopathogenesis of vitiligo is still not well understood. At present, the most prepossessing theory as to the nature of vitiligo relates to autoimmunity. It has been reported in association with many diseases in which autoimmunity plays an important role in their pathogeneses, including diabetes mellitus, pernicious anemia, systemic lupus erythematosus, scleroderma, alopecia areata, and Hashimoto's thyroiditis.
Although hypopigmcntation of the skin is a common occurrence in leprosy, depigmentation is quite unusual. Jopling in 1978 observed a 7% prevalence of vitiligo in patients under treatment for lepromatous leprosy (3). Development of vitiligo following type 2 lepra reaction has recently been reported from India (5). The exact mechanism of development of vitiligo in lepromatous leprosy is not known. The clinical features of type 2 lepra reaction often resemble au toaggressive connective tissue diseases (1). Thirteen of 50 patients with lepromatous leprosy studied by Malaviya, et al. had an tinuclear antibodies in their serum (4). Antithyroid antibody (2) and antibody against testicular germinal cells (6) also have been detected in the serum of these patients. All of these reports indicate that autoimmunity plays a major role in the pathogenesis of vitiligo as well as lepromatous leprosy, particularly when it is in reaction. Therefore, the association of vitiligo and lepromatous leprosy, as observed in our patients, appears to be more than fortuitous and suggests that the development of vitiligo in these patients is the result of some immunologic alteration that led to the phenomenon of autoimmunity. The exact cause of this autoimmunity is not known. It is probably caused by the stimulation of B cells by antigen complexes of Mycobacerium leprae plus autologous tissue, along with dysfunction of T-suppressor lymphocytes (1).
- K. Pavithran, M. D., D. V. D.
Associate Professor
Department of Dermatology and Venereology
Medical College Hospital
Kottayam 686008, India
REFERENCES
1. AZULAY, R. D. Autoaggressive hanseniasis. J. Am. Acad. Dermatol. 17(1987)1042-1046.
2. BONOMO, L. ,DAMMACCO, F. ,PINTO, L. and BARBIERI, G. Thyroglobulin antibodies in leprosy. Lancet 2(1963)807-809.
3. JOPLING, W. H. Vitiligo and leprosy. (Letter) Lepr. Rev. 49(1978)88.
4. MALAVIYA, A. M., PASRICH, J. S. and MEHTA, J. S. Significance of serologic abnormalities in lepromatous leprosy. Int. J. Lepr. 40(1972)361-365.
5. PAVITHRAN, K. Vitiligo following type II lepra reaction. IndianJ. Lepr. 61(1989)44-48.
6. WALL, J. R. and WRIGHT, D. J. M. Antibodies against testicular germinal cells in lepromatous leprosy. Clin. Exp. Immunol. 17(1974)51-59.