- Volume 58 , Number 4
- Page: 641–50
A longitudinal study ot the incidence of leprosy in a hyperendemic area in Zaire, with special reference to PGL-antibody results
ABSTRACT
Between 1984 and 1988, yearly surveys for leprosy were done among the 1500 people living in a previous leprosy segregation village in Zaire. In 1984 lepromin tests and phenolic glycolipid (PGL) antibody tests were done in a significant part of the population. The prevalence of the disease at that time was 16.1 %, the proportion of multibacillary cases was 11.3% overall and 22% among active cases. Prior to 1984, 23% of paucibacillary cases and 56% of multibacillary cases had presented themselves spontaneously to the Leprosy Service. The exposure to the infection is uniform, but there is a suggestion of family clustering of cases. In spite of a rapidly bactericidal treatment of all known cases in 1984 and thereafter, the annual incidence of 0.34% did not decrease during the 4 years of the study. The PGL antibody test did not contribute to the diagnosis, classification or prognosis of the disease.RÉSUMÉ
Entre 1984 et 1988, des enquêtes annuelles pour la lèpre ont été réalisées parmi les 1500 personnes vivant dans un ancien village d'isolement des malades lépreux au Zaïre. En 1984, des tests à la léprominc et de recherche des anticorps contre le glycolipide phénolique (PGL) ont été effectués dans une partie significative de la population. La prevalence de la maladie à cette époque était de 16.1%, la proportion des cas multibacillaires était de 11.3% parmi l'ensemble des cas, et de 22% parmi les cas actifs. Avant 1984, 23% des cas paucibacillaires et 56% des cas multibacillaires s'étaient présentés spontanément au Service de la Lèpre. L'exposition à l'infeciton est uniforme, mais il y a une ébauche de regroupement familial des cas. En dépit d'un traitement rapidement bactéricide de tous les cas connus en 1984 et par la suite, l'incidence annuelle de 0.34% n'a pas diminué au cours des 4 ans de l'étude. Le test de recherche des anticorps anti-PGL n'a pas aidé au diagnostic, a la classification ni au pronostic de la maladie.RESUMEN
Entre 1984 y 1988 se hicieron examenes anuales para detectar lepra entre los 1500 habitantes de un campamento en Zaire, utilizado en el pasado para segregar a los pacientes con esa enfermedad. En 1984 se hicieron pruebas dérmicas de lepromina y pruebas serológicas para anticuerpos contra glicolipido fenólico (PGL) en una gran parte de la población. En ese tiempo la prevalencia de la enfermedad fue del 16.1%, la proporción de casos multibacilarcs fue del 11.3% en general, y del 22% en los casos activos. Antes de 1984, el 23% de los casos paucibacilares y el 56% de los multibacilarcs se habían presentado al Servicio de Lepra de manera espontánea y voluntaria. Actualmente, aunque la exposición a la infección es uniforme, hay evidencias de agolpamiento familiar de los casos. No obstante el tratamiento bactericida de todos los casos en 1984 (y posterior), la incidencia anual del 0.34% no disminuyó durante los 4 años del estudio. La prueba del PGL no contribuyó al diagnóstico, a la clasificación, ni al pronóstico de la enfermedad.Yalisombo (YAL) is an old leprosarium on the left bank of the Zaire River 25 km downstream from Kisangani. Up to 1960, treatment of leprosy patients was assured by the nearby missionary hospital. After independence in 1960, troubled times caused a breakdown of medical services. As a result, the leprosy patients received very irregular dapsone (DDS) treatment, if treatment was given at all. The policy of isolation of the patients in leprosaria was abandoned in 1960, but the local authorities have continued, on their own initiative, to send manifest and suspected leprosy cases to YAL.
The Damien Foundation reactivated leprosy control in the city of Kisangani in September 1982. It soon became evident that YAL constituted a hyperendemic leprosy focus: up to July 1984, 7.4% of the patients registered in Kisangani were living in or had been living in YAL, and 36% of them were multibacillary (MB) compared with a 15% MB proportion elsewhere in the area. In 1984 a total population survey for leprosy was organized at YAL. Thereafter, the population would be re-examined yearly. The results of the annual surveys from 1984 to 1988 are presented here.
MATERIALS AND METHODS
A preliminary demographic survey was undertaken by two students of the Faculty of Psychology, University of Kisangani, during 1 week in 1984. YAL is a cluster of four villages: Yalisombo proper, Yakake (immediately adjoining Yalisombo), Yandjali (2 km from YAL), and Bukukwana (4 km from YAL; can only be reached by boat). Each house was visited and its inhabitants listed on a family record, noting name, sex, date of birth, relation to the head of the family, and date of arrival at YAL.
The initial leprosy survey was carried out during 1 week in August 1984. Each individual was examined clinically by an experienced leprosy worker (complete skin inspection and nerve palpation, and sensory and motor function testing if leprosy was suspected). For all cases suspected of MB leprosy, as well as for all new and old MB cases, skin smears were examined on the spot. A skin biopsy was taken from all suspected cases, all new cases, and all old cases with residual skin lesions. The biopsies, fixed in 10% Formalin, were sent to the Institute of Tropical Medicine, Antwerp, Belgium.
Two thick blood drops were collected on filter paper from all individuals examined. The filter papers were kept at 4ºC and sent to the National Institute for Medical Research, London, where the phenol glycolipid antibody (PGL-A) titers were determined, following the procedure described by Brett, et al. (2). Each blood spot was eluted in 4 ml of phosphate-buffered saline (PBS)-Tween 80 + 3% bovine serum albumin (BSA) (equivalent to an 80-fold dilution), and antibodies against a synthetic antigen were determined. This synthetic antigen consisted of the terminal disaccharide of phenolic glycolipid (3,6-di-O-methyl-β-glucopyranosyl-(l → 4)-2,3-di-O-methyl-α-L-rhamnopyranose) which was coupled to BSA using the allyl aglycone. This antigen was kindly provided by Dr. R. Gigg, Laboratory of Lipid and General Chemistry, National Institute for Medical Research, London. Each sample was tested in triplicate, plus a "no-antigen" control. The results were recorded as the difference in optical density units (ODU) between the test reading and the "no-antigen" control reading (Δ ODU). A Δ ODU of 0.20 or greater was considered to be positive; a Δ ODU of 0.10-0.19 was considered to be doubtful.
A lepromin test (WHO lepromin H containing 4 x 107 bacilli per ml was supplied by the National Institute for Medical Research) was performed on all children under 15 years of age, and on old cases of uncertain classification, by administering 0.1 ml of lepromin intradermally. The tests were read after 28 days, and an induration of 3 mm and more was considered positive.
All leprosy cases received appropriate multidrug therapy.
All results were entered on the family record, and allowed each individual to be classified as to his/her leprosy status: no leprosy, old case (existing record or intake of leprostatics in the past, regardless of regularity), new case (never treated before), paucibacillary (PB) or multibacillary (MB), active or inactive. New cases were classified as MB if a bacterial index (BI) of 2 or more was found at any site. The classification of the old cases was based on whatever information was available: either the smear result (all positive skin smears being considered as MB), the biopsy result, the initial classification or a lepromin result of > 3 mm. The criteria for activity were: all new cases and old PB cases = inflamed skin lesions or painful enlarged nerves with a skin biopsy revealing a tuberculoid granuloma; old MB cases = a positive skin smear.
Follow-up surveys were carried out in September 1985 and in August 1986, 1987, and 1988. Two months prior to each follow-up survey, the village chiefs and elders were contacted, and in 1986 two students from the University of Kisangani visited all of the families at home 1 month prior to the survey in order to stimulate them to participate in the survey. All inhabitants previously known to be free of leprosy, as well as all newly arrived inhabitants, were examined according to the 1984 survey, except that lepromin tests were not performed and blood samples for PGL-antibody determination were not taken.
Statistical analysis included the Student t test for comparing means, the χ2 test with Yates' continuity correction for comparing proportions, and the Mantel-Haenzel χ2 test for comparing rates.
RESULTS
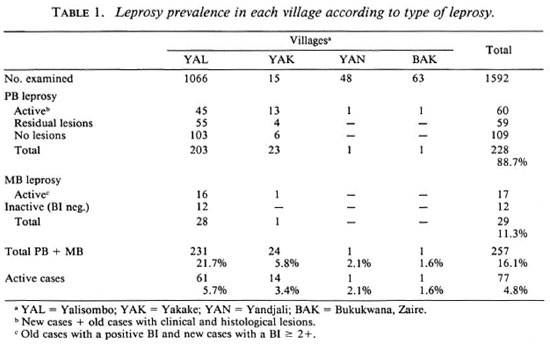
Leprosy prevalence (Table 1). Of the 1768 individuals registered during the preliminary demographical survey, 1394 (78.8%) and 198 new, unregistered individuals were examined; a total of 1592 people from 282 families.
All PB cases were confirmed by histopathology. Three of the 30 newly diagnosed PB cases without signs of leprosy in the biopsy were nevertheless considered as cases on clinical grounds because there was anesthesia and motor function impairment. No misclassifications between PB and MB leprosy have been made in the field.
The overall prevalence as well as the prevalence of active cases is very high, but this is mainly due to the extremely high prevalence in Yalisombo village, the original leprosarium. In the three other villages, which were founded later, the prevalence diminishes as a function of the distance from Yalisombo. Thirty of the PB patients (13.2%) and 1 of the MB patients (3.4%) are newly detected cases (no existing records, no known previous treatment). The other patients had records at the Yalisombo dispensary or claimed to have received DDS in the past. However of these "old" cases only 14 PB (47% of the old active PB cases) and 9 MB cases (56% of the old MB cases) were receiving treatment in Kisangani at the time of the survey.
Leprosy patients are older than the general population (median age general population = 19; leprosy patients = 41). This difference is mainly due to the old cases who have a median age of 44, against 24 for the new cases, while 26% of the new cases are children under 15 years of age. There is a significant (0.005 > p > 0.001) predominance of males in the leprosy population (57%), compared with the nonleprosy population (47%), for PB (57%) as well as for MB (59%) patients.
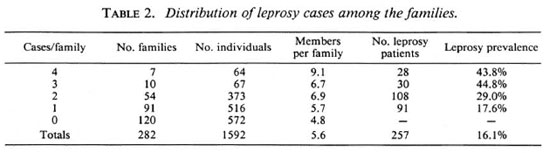
Of the 282 families examined, 162 (57.4%) had at least one case of leprosy: Yalisombo, 79.9%; Yakake, 28.4%; Yandjali, 12.5% and Bakukwana, 38%. Seventy-one (42.5%) of the leprosy families had more than one case of leprosy. The family composition in relation to the number of leprosy cases in the family is given in Table 2. The families with the most cases are also the largest ones. In the 3-case and 4-case families almost half their members have leprosy.
Results of lepromin tests. Seventy-five percent (543) of the 725 lepromin tests were read. Among the leprosy patients, the three MB cases had a lepromin result of 0 mm. Among 48 PB cases, 44 were lepromin positive, with a mean diameter of 5.9 mm. Of the 4 lepromin negative PB cases, 1 had a reading of 2 mm, and 3 had no induration. Two of the latter had a BI of 1 + , and one of these relapsed 2 years later as BL with a BI of 4; the other one was lost to follow-up. The two other lepromin-negative PB cases had a satisfactory evolution.
The lepromin results of the 492 individuals without leprosy are presented in The Figure. Based on this graph, a 3-mm induration was used as the cut-off point for lepromin positivity. Thus, 87.6% of the individuals without leprosy were lepromin positive and 12.4% were lepromin negative. The mean diameter in the lepromin-positive individuals was 5.6 mm; negative results diminish with increasing age, while the mean diameter in lepromin-positive individuals increases.
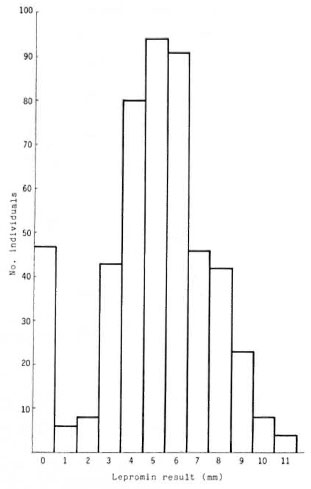
The Figure. Distribution of skin test results.
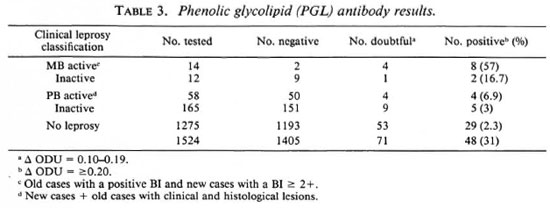
PGL-A results. A total of 1524 blood samples were tested for PGL-A. Table 3 presents the results according to leprosy status. The percent positive corresponds to the sensitivity of the test. If the doubtful results are included among the positives, the sensitivity increases from 51.1% to 87.7% among active MB patients, from 38.5% to 57.7% among all MB patients, and from 7.6% to 14.9% among all leprosy patients.
The specificity of the test, as measured among the YAL inhabitants without leprosy, is 97.7%.
The positive predictive value of the test is 39.6% for discriminating between leprosy patients (all types, prevalence = 16.1%) and healthy controls; 20.8% for discriminating between MB patients (active and inactive, prevalence = 1.7%) and other individuals (PB patients and healthy controls); and 16.7% for discriminating between active MB patients (prevalence = 0.92%) and all other individuals (inactive MB patients and PB patients and healthy controls). For the active MB patients no correlation between the PGL-A result and the BI could be demonstrated.
The age distribution of the PGL-A positives is comparable to that of the PGL-A negatives, among nonleprosy individuals as well as among leprosy patients. The PGLA-positive individuals without leprosy were not preferentially found in the families with leprosy cases, nor had the type of leprosy present in the family any influence (data not shown).
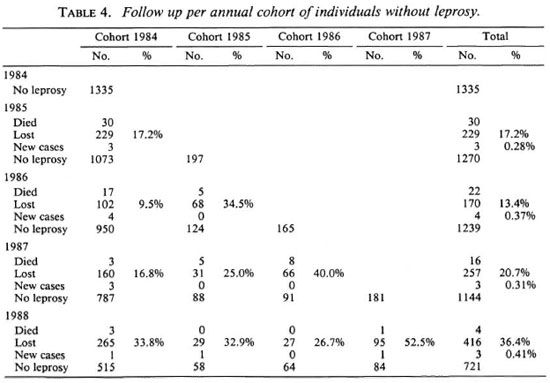
Follow-up surveys. The individuals without leprosy were re-examined annually. Each year individuals not seen before were included in the study. Table 4 presents data on the annual follow-ups. The 1984 cohort has been followed for 3333 person years (py) out of a possible 5340; the 1985 cohort, for 271 py out of a possible 591; the 1986 cohort, for 155 py/330; the 1987 cohort, for 55 py/181; or a total of 3814 py/6442.
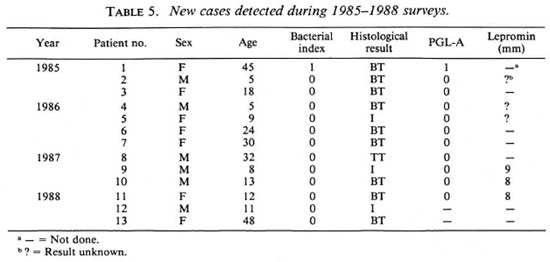
Between 1985 and 1988, no new cases of MB leprosy were detected while the mean yearly incidence rate of PB leprosy was 0.34%-variations in yearly incidence rates (from 0.28 to 0.41%) are not statistically significant-and no new cases from Yalisombo were seen in Kisangani. The particulars of the new cases are given in Table 5: they are young (mean age 20 years), 7 out of 13 (54%) are under 15; 6 are male and 7, female. All are PB cases (one case had a BI of 1): 3 indeterminate (23%), 1 TT (8%), 9 BT (69%). In all three of the new cases in whom a lepromin test was done in 1984, it was strongly positive.
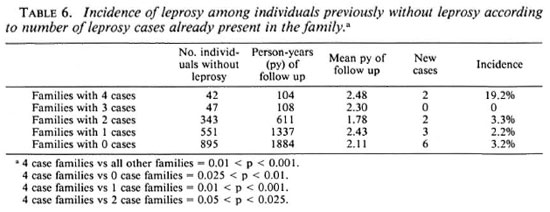
Table 6 presents the new cases according to the number of leprosy cases already present in the family. The incidence in the 4 case families is significantly higher than in the other families (0.01 > p > 0.001). Being a member of a 4-case family in YAL is associated with a relative risk of 6.5 of developing leprosy.
PGL-A had been determined in 1984 for 11 out of the 13 new cases; only one had a doubtful positive result of 1 + . The 82 PGL-A-positive individuals of the 1984 cohort without leprosy have been followed for 189 py out of a possible 328 (mean = 2.31 years), and the 1193 PGL-A-negative individuals for 3018 py out of a possible 4772 (mean = 2.53 years; the difference is slightly significant, 0.05 > p > 0.025. Among the PGL-A positives, one new case (patient 1, Table 5) was diagnosed but with a doubtful positive result of 1 + .
The overall incidence of leprosy among PGL-A positives (if the 1 + results are included) is 1/189 (0.53%) compared to 10/3018 (0.3 3%) among PGL-negati ves; the difference is not statistically significant.
The 37 PGL-A-positive patients diagnosed in 1984 were followed for 106 py out of a possible 148 (mean = 2.86 years. This is significantly longer than the disease-free, PGL-positive persons). Of these 37 patients 6 were never seen again (4 died, 2 disappeared). One patient, classified as old inactive PB with a PGL-A result greater than 1.0 Δ ODU, relapsed as MB in 1985. A second patient, classified as old inactive PB (biopsy = arrested BT lesions) and a PGL-A result of 0.20 Δ ODU, presented a reactivation of his BT lesions in 1987. No other aggravations were observed. The remaining 29 patients showed a satisfactory evolution, 26 being considered cured at their last follow-up examination.
The 212 PGL-A-negative patients of the 1984 cohort were followed for 656 py out of a possible 848 (mean = 3.09 years, comparable to the PGL-A-positive leprosy patients). Seven patients died and 10 disappeared. Six patients showed an unsatisfactory evolution. Three patients presented a PB relapse; they had clinically active PB leprosy in 1984 and a negative biopsy after treatment in 1986, but relapsed in 1987 or 1988 with BT leprosy. Two patients with active PB leprosy in 1984 did not respond to treatment and showed persistent activity with a positive biopsy in 1987. One patient, diagnosed in 1984 as old inactive PB, presented a reactivation of the lesions in 1986. The remaining 189 patients showed a satisfactory evolution and 133 were considered cured at their last follow-up examination.
DISCUSSION
YAL constitutes a hyperendemic leprosy focus. In 1984 the overall prevalence rate was 22% in Yalisombo village, 6% in Yakake, and 2% in both Yandjali and Bakukwana. Many of the patients were old cases no longer in need of antibacterial treatment. Taking into consideration only the active cases who needed such treatment, the prevalence rate was still as high as 6% in Yalisombo village, 3% in Yakake and 2% in both Yandjali and Bakukwana. By comparison the prevalence rate in the adjoining areas is between 0.4% and 0.6% (3). The reason for this extremely high prevalence is the active segregation policy in use until 1960, and even later on when a considerable number of patients were sent to YAL by the civil authorities, or came there on their own initiative. Thus there has been a huge influx of leprosy patients from outside: 146 out of the 257 patients had leprosy when they arrived in YAL. This high concentration of untreated or insufficiently treated cases constituted a potent source of transmission: out of 1446 individuals who showed no signs of leprosy when arriving in YAL, 111 (7.7%) developed the disease. Even if we allow for some of those cases to have contracted the disease before their arrival, transmission in YAL must have been intense.
In spite of the heavy river traffic between YAL and Kisangani, and in spite of the fact that the Kisangani leprosy service was well known in YAL, only 14 out of the 61 active PB cases and 9 out of the 16 active MB cases had sought treatment on their own initiative. Thus, through spontaneous presentation only 23% of the PB cases and 56% of the MB cases were detected. Among the YAL patients treated in Kisangani 36% were MB, but the YAL survey revealed an overall MB proportion of 11.3%, and an MB proportion of 22% among the active cases, comparable to the MB proportion found in the adjoining areas of between 14% and 23% (3). The high number of MB cases observed in Kisangani is thus caused by a presentation bias. The results of the surveys also suggest that the MB rate in a population remains constant, in spite of the high infection pressure.
Among the new cases (never treated before), 26% were children, as compared to a child proportion of 12% (3) in the adjoining areas. This is most probably the result of earlier detection during active case-finding. The male predominance among both PB and MB patients remains unexplained. In the adjoining areas a male predominance is found among MB patients, but among PB cases the sexes are distributed equally.
Sixty-two of the disease-free individuals had a negative lepromin test. There are two explanations for a negative lepromin result in an endemic area: a) either infection with Mycobacterium leprae has not yet occurred, or b) it did occur but the individual does not react and is incubating or at risk of developing a MB form of the disease. It is unlikely that there were many cases incubating a MB form of the disease in this population, since no new cases were detected during the next 4 years. An argument in favor of the first mechanism can also be found in the age and family distributions of the results; negative results decrease with age, while the mean diameter of induration increases. Exposure to M. leprae could be expected to be highest in families with active MB cases and in families with multiple leprosy patients. However, no relation could be found between the prevalence of lepromin negativity and the number of patients in the families. This seems to indicate that the infection pressure in YAL is equal for the whole population, the prevalence of disease being so high that differences between families do not play any role, leaving age as the only limiting factor to exposure (beyond the age of 10 years almost all inhabitants of YAL have a positive lepromin test).
The PGL-A-positivity rate decreases from MB to PB to "no leprosy," whether a Δ ODU of 0.10 or of 0.20 is taken as the cutoff value for positivity. This decrease is most dramatic between active and inactive MB cases. The test managed to pick up 12 out of 14 active MB cases but at a cost of many false-positives, resulting in a low positivepredictive value. This predictive value will be even lower in an area with a lower MB prevalence. For a MB prevalence of0.092%, as in many Central African areas, the positive predictive value for active MB cases would be 1.1 %.
No relation could be found between PGL-A positivity and the bacterial index, age, or the presence of leprosy cases in the family.
The limited value of the PGL-A test as a diagnostic and prognostic tool found in the present study confirms the observations of other studies in the field. Seropositivity is consistently higher in MB patients than in PB patients (1,4), and in leprosy patients than in nonleprosy individuals (1,4,5). Seropositivity in contacts of known leprosy cases is higher than in healthy controls in some studies (1,4) but not in others (5), or it is higher in contacts of more than 1-year duration of lepromatous patients than in other contacts or healthy controls (6). However, the number of false-positives is always considerable and makes interpretation of individual results in the field very difficult. One study (5) actually found that antibodies against M. tuberculosis provide a better discrimination between leprosy patients (all types) and healthy subjects than do IgM antibodies against M. leprae PGL-I. The latter test had a sensitivity of 43% and a specificity of 95%, but this specificity was arbitrarily fixed by the investigators. Two studies (1,4), determining IgM antibodies against the natural disaccharide coupled with an octyl spacer arm to BSA (ND-O-BSA), yielded a sensitivity of 100% for detecting MB patients, and of 44% and 57.4%, respectively, for discriminating between leprosy and normal individuals. The specificity as determined from endemic noncontact persons was 95.5% and 98%, respectively. But in these studies the group sizes were determined by the investigators, and no predictive values can be calculated.
The 0.34% yearly incidence rate of leprosy in YAL is much higher than the detection rates of between 0.03% and 0.06% in the adjoining areas (3). However, the latter figures are based on passive case-finding which may represent ½ or ¼ of the true number. The active case-finding in the YAL surveys also results in early detection; 54% of the new cases were children as compared to 12% in the adjoining areas.
The incidence rates obtained during the 1985-1988 surveys are probably a reflection of the transmission before the 1984 survey. In 1984 all leprosy cases, active as well as inactive, were treated with bactericidal therapy, and all new cases and relapses found thereafter were also treated right away, thus reducing the infection sources considerably. It is therefore thought that almost all new cases found during the follow-up surveys were already infected in 1984 and incubating the disease in 1984 or later. If this is the case, the PGL-A test was not useful at all in detecting subclinical infection: only 1 out of 11 new cases had a doubtful positive result. It may be of interest to note that this patient also had a BI of 1+.
All new cases are PB. If the proportion of MB among newly detected cases is comparable to that in the adjoining areas (between 9% and 12%), one new MB case could be expected. No new MB cases have been detected so far, but further follow-up is indicated.
The family distribution of the new cases suggests clustering of the disease. But, as shown by the lepromin results and the very high overall prevalence of the disease, it seems unlikely that members of 4-case families are more heavily exposed to infection. However, it is possible that there is a family predisposition for the development of disease after infection. Speculations about the nature of this predisposition are beyond the scope of the present paper.
The follow-up of the 1984 cohort in relation to PGL-A results shows very inconclusive results. Although 1 old PB case with a PGL-A result of 10+ relapsed as MB, 7 other leprosy patients with a high positive PGL-A result (between 6+ and 14+) did not relapse, and 6 highly positive (between 6+ and 14+) individuals without leprosy did not develop the disease.
Among the cohort without leprosy, the PGL-A positives (including the doubtful 1 + results) showed a leprosy incidence of 0.53% compared to 0.33% among the PGL-A negatives. This is remarkably comparable to observations in French Polynesia (4), where 3 new cases were observed among 631 seronegative contacts followed for 1262 py (incidence = 0.23%), and 1 new case among 93 seropositive contacts followed for 186 py (incidence = 0.53%). It is of interest to note that the three seronegative contacts who developed leprosy (all of the PB type) remained seronegative after developing the disease.
Among the leprosy cohort, 6.25% of the PGL-A positives, again including the doubtful 1+ results, compared to 3.1% of the PGL-A negatives showed an unsatisfactory evolution, but 81.2% of the PGL-A positives were considered cured by 1988 as compared to 70.4% of the PGL-A negatives. None of the differences between the PGL-A positives and PGL-A negatives are statistically significant. If only the PGL-A results of at least 2+ are considered, the leprosy incidence is 0 among PGL-A positives and 0.35% among PGL-A negatives. Among the PGL-A-positive patients, 9% presented an unsatisfactory evolution while 75% were considered cured by 1988. Among the PGL-A-negative patients, 2.9% presented an unsatisfactory evolution while 71.8% were considered cured by 1988. Again, none of the differences are statistically significant.
In spite of the efforts of the survey team, many people have been lost to follow-up. Of the 1984 cohort only 39.4% were followed for 4 years. This is partly due to the mobility of the population; each year there is about a 15% immigration and emigration. However, quite a few people seem to drop out due to lack of interest in the survey. This was investigated in 1986, when a psychology student at Kisangani University interviewed 100 absentees (7). The main reason for absenteeism seemed to be a disappointment in the survey team; the population expected the survey team to provide general medical care. There was also some dissatisfaction about the timing of the survey and, surprisingly, in view of the very high leprosy prevalence in YAL, many of the interviewees manifested very inadequate knowledge of the disease. The survey team subsequently tried to improve collaboration through health education campaigns, through extensive explanation of the purpose of the study to the village chiefs and elders, and even through individual home visits. The timing of the survey was also rearranged. However, attendance did not improve and, in view of the efforts made, it is probably the best that can be achieved.
From the present study the following conclusions can be drawn: a) In the hyperendemic Yalisombo situation with a leprosy prevalence of 16.1%, exposure to infection is uniform but there is a suggestion of family clustering of cases, b) The annual incidence rate is very high (0.34%) and 54% of the new cases are children, indicating an intense transmission, c) There is no decrease of the incidence during the first 4 years after the elimination of the known infection reservoir by bactericidal treatment, d) The PGL-A test does not contribute to the diagnosis or classification of leprosy; it does not give prognostic indications and does not detect incubating forms of the disease.
REFERENCES
1. AGIS, F., SCHLICH, P., CARTEL, J.-L., GUIDI, C. and BACH , M.-A. Use of anti-M. leprae phenolic glycolipid-1 antibody detection for early diagnosis and prognosis of leprosy. Int. J. Lepr. 56(1988)527-536.
2. BRETT, S. J., DRAPER, P., PAYNE, S. N. and REES, R. J. W. Serological activity of a characteristic phenolic glycolipid from Mycobacterium leprae in sera from patients with leprosy and tuberculosis. Clin. Exp. Immunol. 52(1983)271-279.
3. BUREAU NATIONAL DE LA LÈPRE. Statistiques annuelles. Kinshasa, Zaire: Ministry of Public Health.
4. CHANTEAU, S., CARTEL, J.-L., GUIDI, C, PLICHART, R. AND BACH , M.-A. Seroepidemiological study of 724 household contacts of leprosy patients in French Polynesia using disaccharide-octyl-BSA as antigen. Int. J. Lepr. 55(1987)626-632.
5. CREE, I. A., SMITH, W. C. and BECK, J. S. Serum antibody responses to mycobacteria in leprosy patients and their contacts. Lepr. Rev. 59(1988)317-327.
6. MENZEL, S., HARBOE, M., BERGSVIK, H. and BRENNAN , P. J. Antibodies to a synthetic analog of phenolic glycolipid-I of Mycobacterium leprae in healthy household contacts of patients with leprosy. Int. J. Lepr. 55(1987)617-625.
7. MWANASANGEZI, B. M. and GROENEN, G. Reasons for non-response during an ongoing leprosy survey in northern Zaire. Ann. Soc. Belg. Med. Trop. 67(1987)271-275.
1. M.D., Bureau National de la Lèpre, Kinshasa, Zaire.
2. M.D., Professor of Microbiology, University of Antwerp and Institute of Tropical Medicine, Nationalestraat 155, 2000 Antwerpen, Belgium.
3. M.D., Damien Foundation, Kisangani, Zaire.
4. M.D., University of Kisangani, Zaire.
5. Ph.D., National Institute for Medical Research, Mill Hill, London NW7 1AA, U.K.
6. Mwanasangezi, Mwinyihali (University of Kisangani), E. Nollet, M. Vermander, L. Coussens, J. Verlinden, R. De Raedt, L. Van Laeken, L. Breugelmans (Damien Foundation, Kisangani).
Reprint requests to Professor S. R. Pattyn.
Received for publication on 30 October 1989.
Accepted for publication in revised form on 29 March 1990.