- Volume 58 , Number 4
- Page: 660–5
Sexually transmitted diseases in leprosy patients in north and northeastern India. A futile search for human immunodeficiency virus antibody
ABSTRACT
Three-hundred-eighty-four leprosy patients were clinically examined for sexually transmitted diseases (STD) in north and northeastern India, revealing a high incidence (5.2%) of STD among them. Eighteen males, one female, and one eunuch were found to have chancroid ulcer, gonococcal urethritis, lymphogranuloma inguinale, and primary chancre. Of these patients, only 100, selected randomly, could be screened serologically for STD due to Treponema pallidum, herpes simplex (type 1 and 2), Entamoeba histolytica, hepatitis-associated virus, cytomegalovirus, Chlamydia trachomatis and human immunodeficiency virus (HIV); 100 control sera were included for comparison. In addition, sera f rom another 133 normal subjects and another 176 lepromatous patients were also screened for HIV antibody. Thus, a total of 233 normal sera and 276 leprosy sera were tested for HIV antibody. Although our leprosy patients have shown significantly high incidences of clinical STD and also high seropositivity against T. pallidum, herpes-simplex viruses types 1 and 2, hepatitis-associated virus, and cytomegalovirus, the search for antibody against HIV was negative. Our clinical and serological data suggest promiscuity in our patient population. The absence of HIV antibody in this high-risk population, however, seems to be an enigma.RÉSUMÉ
Trois cent quatre-vingt-quatre malades de la lèpre ont été examinés cliniquement pour la recherche de maladies sexuellement transmissibles (MST) dans le nord et le nord-est de l'Inde, révélant une incidence élevée (5.2%) de MST parmi eux. Dix-huit hommes, une femme et un eunuque ont présenté ulcère chancroide, urétritc gonoccique, lymphogranulome inguinal et chancre primaire. Parmi ces patients, seuls 100, choisis au hasard, ont pu être examinés sérologiquement pour MST due à Treponema pallidum, herpes simplex (types 1 et 2), Entamoeba histolytica, le virus associé à l'hépatite, le cytomegalovirus. Chlamydia trachomatis, et le virus de l'immunodéficience humaine (VIH); 100 sérum-témoins furent inclus pour comparaison. De plus le sérum de 133 autres sujets normaux et 176 autres patients lépromateux furent également examinés pour la recherche d'anticorps anti-VIH. En conséquence, un total de 233 sérums normaux et 276 sérums lépreux ont été testés pour la recherche d'anticorps anti-VIH. Bien que nos patients lépreux aient montré des incidences significativenient élevées de MST cliniques, et également une séropositivité élevée vis-à-vis de T. pallidum, des virus de l'herpès simplex de types 1 et 2, du virus associé à l'hépatite et du cytomegalovirus, la recherche des anticorps vis-à-vis du VIH s'est révélée négative. Nos données cliniques et sérologiques suggèrent la promiscuité dans notre population de patients. L'absence d'anticorps anti-VIH dans cette population à haut risque apparaît cependant comme une énigme.RESUMEN
Se examinaron 384 pacientes con lepra en el norte y noreste de la India para buscar evidencias clínicas de enfermedad de transmisión sexual (ETS). Los resultados revelaron una alta incidencia (5.2%) de ETS en la población estudiada. Diez y ocho hombres, una mujer, y un eunuco tuvieron úlcera chancroide, uretritis gonocócica, linfogranuloma inguinal, o chancro primario. De todos los pacientes, solo 100, seleccionados al azar, pudieron investigarse serológicamente para buscar ETS debidas a Treponema pallidum, herpes simplex (tipos 1 y 2), Entamoeba histolytica, virus asociado a hepatitis, citomcgalovirus. Chlamydia trachomatis y virus de la inmunodeliciencia humana (HIV); se incluyeron 100 sueros control para comparación. Además, los sueros de otros 133 individuos normales y de otros 176 pacientes lepromatosos también se investigaron para anticuerpos contra HIV. Aunque los pacientes con lepra mostraron una elevada incidencia clínica de ETS y también una alta seropositividad contra T. pallidum, virus del herpes simplex (tipos 1 y 2), virus asociados a hepatitis, y citomcgalovirus, la búsqueda de anticuerpos contra HIV fue negativa en los 276 pacientes con lepra estudiados. Los datos clínicos y scrológicos sugieren promiscuidad en la población de pacientes, sin embargo, la ausencia de anticuerpos anti-HIV en esta población de alto riesgo resulta enigmática.A recent editorial (27) has suggested that it may be necessary to do human immunodeficiency virus (HIV) "serology on all subjects that develop leprosy as well as a parallel sample of the surrounding population" because the authors thought that leprosy made a patient immunocompromised and thus susceptible to HIV infection. An association of Mycobacterium leprae and HIV infections was reported in a Brazilian subject (8). A high incidence of syphilis in leprosy patients was reported from The Philippines (4) and the United States of America (11). Treponema pallidum, Neisseria gonorrhea, herpes-simplex virus (HSV), hepatitis-B virus (HBV), Toxoplasma gondii, Entamoeba histolytica, cytomegalovirus (CMV), Chlamydia trachomatis, and HIV are notifiable sexually transmitted disease (STD) agents by the World Health Organization (WHO) (28). Recently, sexually transmitted CMV proctitis has been reported in a woman (17). Only syphilis, gonorrhea, chanchroid, lymphogranuloma inguinale, and lymphogranuloma venerum are common agents of STD in India (12). Shiv Raj, et al. (26) and Malkovsky and Dilger (9) studied leprosy patients and normal healthy individuals for anti-HIV antibody and found all subjects to be negative.
A high incidence of antibodies to T. gondii and the Epstein-Barr virus (EBV) in the sera of lepromatous patients was reported by us earlier (19-22). In this communication, we report a clinical and serological survey for a few common STD agents in Indian leprosy patients.
MATERIALS AND METHODS
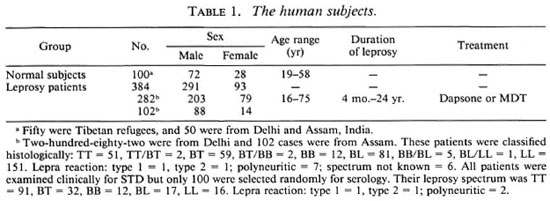
Human subjects. Table 1 shows the details of control subjects and leprosy patients who were included in the present study, all belonging to a low socioeconomic level. One hundred of these patients attended the leprosy clinic of Ram Manohar Lohia Hospital, New Delhi, India, and 182 cases belonged to Faridabad and Raghubir Nagar leprosy colonies of Delhi in northern India. The remaining 102 cases belonged to Assam State in northeastern India. Fifty normal subjects in Delhi belonged to the Tibetan refugee camp where prostitution and drug addiction are common. Fifty males belonging to a low socioeconomic group served as controls. Another 133 sera from normal subjects and 176 sera from lepromatous patients were included only for screening for the HIV antibody.
Clinical examinations were performed by three of the authors (PKT, AKS, and US) by taking each patient's history and performing a physical examination. Serological studies. Only 100 out of the 384 leprosy patients, selected at random, along with 100 controls were included for the following serological tests. Indirect hemagglutination (IHA) tests were performed to detect antibodies against T. pallidum and E. histolytica (Behringwerke, Marburg, West Germany) and against the HSV-1 and HSV-2 antigens (obtained from Vero cells infected with HSV-1 and HSV2) coated on sheep red blood cells (25). A reverse passive hemagglutination test was carried out for screening for HBV (Ortho Diagnostics, India). Antibody of the IgG/IgM class against CMV as well as that of the IgG class against C. trachomatis was detected by an indirect ELISA test (Labline, Finland). Antibody to HIV was screened by a competitive ELISA (Wellcome, Beckenham, England).
A statistical evaluation of significance for comparison among the cases and controls was performed by the chi-squared test.
RESULTS
A clinical survey of leprosy patients in Delhi showed clinical evidence of STD in a total of 9 individuals (7 males, 1 female, 1 eunuch), 7 of whom had lepromatous (LL), 1 had tuberculoid (TT), and 1 had borderline tuberculoid (BT) types of leprosy. Out of 102 leprosy patients from Assam, 11 males had clinical STD and of these, 4 had TT, 3 had BT, 3 had borderline lepromatous (BL), and 1 had LL leprosy (Table 1). The age of these 20 patients varied from 15 to 57 years. One male and one female were married. All except the female patient had a history of extramarital sexual contact; of them, 10 had chancroid ulcer with or without bubo; 5 had primary chancre, 4 including the eunuch had acute gonococcal urethritis; and 1 case had lymphogranuloma venerum with discharging inguinal lymph nodes. The only female LL patient (20 years old) had a history of sexual contact with her husband (TT), and she developed multiple chancroid on the rectal orifice and labia minora. She had an enlarged and tender inguinal lymph node.
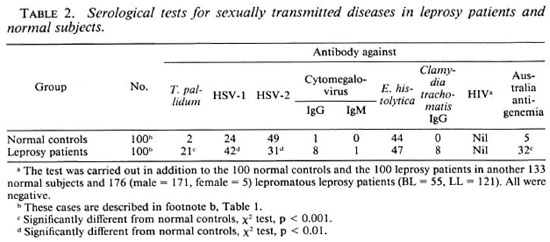
Table 2 shows that the incidences of seropositivities against the common STD agents were significantly more in the lepromatous patients than in the controls. Thus, a high occurrence of T. pallidum, HBV, and HSV1 antibodies along with a high positivity for antibodies of both IgG and IgM classes against C. trachomatis as well as CMV (IgG class) were noted in the leprosy patients. However, the incidence of E. histolytica seropositivity was comparable in the two groups (Table 2). Antibody against HIV could not be detected in any of the serum samples from the 233 normal subjects or from the 276 leprosy patients.
DISCUSSION
At least 20 million people, mostly of low socioeconomic status, suffer from STD in India, resulting in large-scale morbidity and mortality (12). In the past 6 months, 3000 male patients with ailments other than leprosy, mostly from the middle-income group, were clinically examined by one of us (PKT) in a clinic from the area adjoining where our leprosy patients reside. Of these male patients, 420 were found to be suffering from STD. Their sexual contacts were with prostitutes, and the spectrum of STD was as follows: herpes, 30%; gonorrhea, 35%; chancroid, 25%; condylomata acuminata, 10% and a few cases of syphilis. All had penile lesions but no anal lesions were seen, which is compatible with an absence of homosexuality in this society. In another survey by one of us (US) in a STD clinic in north-eastern India, 48 STD cases (47 males and 1 female, age range 16-77 years) were recorded out of 192 cases. Chancroid ulcer was seen in 23; primary chancre, in 12; secondary syphilis, in 2; venereal warts, in 1; herpes balanitis, in 1; gonococcal urethritis, in 9.
Our leprosy patients showed significantly elevated seropositivity against T. pallidum and HBV (2). The increased incidence of seroreactivity against HSV-1 and HSV-2, CMV, and C. trachotnatis among our leprosy cases has not been reported earlier, although infection due to these agents has been described in other clinical groups (15, 24). The higher incidence of HSV-1 seropositivity than that of HSV-2 in our patients (Table 2) indicates recent genital herpes infection, leading to the boosting of HSV-1 antibody during HSV-2 infection. This is due to antigenic crossreactivity of these two viruses (6). The absence of clinical herpes in our patients may be due to the masking of herpes infections by other STD. The incidence of seropositivity against E. histolytica issimilar in leprosy patients and controls (Table 2). A higher incidence of mild-to-moderate undernutrition (18) and pulmonary tuberculosis have been reported in leprosy patients residing in the same area (21). Malaria and chronic parasitic infections, certain viruses, and undernutrition are considered to be important co-factors for HIV infection (5,10,16).
Recently, 6% false-positivity has been reported in 100 Somalian leprosy patients (14). These authors also found a 4% false-positivity in 75 Indonesian leprosy patients, while all 62 Italian patients were constantly HIV negative. This false-positivity may be due to malarial antibody (16) and the presence of circulating serum immune complexes (23) . Also, no relationship was established between HIV infection and immunocompromised patients with sleeping sickness in the Congo (13). In the Sudan, with a high prevalence of HIV infection, Fox, et al. (3) found no evidence of the AIDS virus infection in 11 patients with nasopharyngeal carcinoma, an EBV-related malignancy, despite EBV being known to be a potential co-factor in the pathogenesis of AIDS. Thus, seronegativity toward HIV in leprosy patients in different parts of the globe is an enigma, and needs further exploration. All of these studies showing nonassociation between AIDS and chronoic parasitic and viral diseases in different parts of the world, including Africa where there are also high incidences of both leprosy and AIDS, support our finding of HIV seronegativity in leprosy patients from India. Paradoxically, between AIDS and leprosy there exist several similar immunological dysfunctions (7,20,23). Other similarities between them are the reported co-infection of M. tuberculosis in American AIDS patients (1) and the high incidence of pulmonary tuberculosis in Indian lepromatous leprosy cases (21). We have found a high incidence of Australia antigenemia in our patients but not HIV infection, although their mode of transmission is similar (2). Mycobacterial infections and associated undernutrition leading to immunosuppression may accelerate the progression to AIDS. A probable explanation of our finding is that AIDS cases are rarely found in India (5). The epidemiological data suggest that a few Indian subjects acquired AIDS while they were in the U.S.A., and one had homosexual contact in Germany. These very few nonresident Indian AIDS patients might not have been enough to have resulted in the penetration of the virus into the vast majority of the Indian population. But this does not seem to be the explanation for the HIV seronegativity in the leprosy patients of Africa, where the AIDS infection rate is high.
Our clinical data and serological evidence suggest promiscuity in our patients, although not well documented. A strong correlation was reported between the incidence of genital ulcer and HIV due to predisposing factors such as epithelial disruption, inflammation, and the increase in the number of lymphocytes locally which facilitate the AIDS infection (27). Thus, the absence of serological evidence of HIV infection despite clinically proved STD cases among our leprosy patients seems to be a paradox.
Acknowledgment. We are grateful to the Indian Council of Medical Research, New Delhi, for financial support and to Dr. K. K. Dutta, Assistant Director General, AIDS Cell, Government of India, New Delhi, for providing the HIV test reagents.
REFERENCES
1. CHAISSON, R. E. and S LUTKIN , G. Tuberculosis and human immunodeficiency virus infection. J. Infect. Dis. 159(1989)96-100.
2. DUTTA, R. N. and S AHA , K. Australia antigen and lepromatous leprosy: its incidence, persistence and relation to cell-mediated immunity. Indian J. Med. Res. 61(1973)1758-1765.
3. FOX, E., EL TIGANI, A., G EORGE , J. F., HIDAYATALLA, A., BURANS , J. P. and MORRILL, J. C. Nasopharyngeal carcinoma not associated with HIV in Sudan. Trans. R. Soc. Trop. Med. Hyg. 81(1987)1012-1013.
4. GARNER, M. F., BLACKHOUSE , J. L., DASKALOPOULAS , G. and WALSH , J. L. Treponema pallidum haemagglutination (TPHA) test in biological false positive and leprosy sera. J. Clin. Pathol. 26(1973)258-260.
5. INDIAN COUNCIL OF MEDICAL RESEARCH. Epidemiological features of AIDS-a global public health problem. Bull. Cen. AIDS Res. Control (CARC) 1(1988)4-11.
6. JACOB, M., RAO, R. S. S., SRIDHARAN, G. and JOHN, T. J. Epidemiology & clinical profile of genital herpes. Indian J. Med. Res. 89(1989)4-11.
7. KROWKA , J., STITES, D., MILLS, J., HOLLANDER, H., MCHUGH, T., BUSCH, M., WILHELM, L. and BLACKWOOD , L. Effects of interleukin 2 and large envelope glycoprotein (gp 120) of human immunodeficiency virus (HIV) on lymphocyte proliferative responses to cytomegalovirus. Clin. Exp. Immunol. 72(1988)179-185.
8. Lamfers, E. J. P., Bastiaans, A. H., Mravunac, M. and RAMPEN , F. H. Leprosy in acquired immunodeficiency syndrome. (Letter) Ann. Intern. Med. 107(1987)111-112.
9. MALKOVSKY, M. and DILGER , P. Failure to detect antibodies to HIV-1 in sera from patients with mycobacterial infections. (Letter) Int. J. Lepr. 57(1989)866-867.
10. MARLINK, R. G. and ESSEX, M. Africa and the biology of human immunodeficiency virus. JAMA 257(1987)2632-2633.
11. MURRAY , K. Syphilis in patients with Hansen's disease. Int. J. Lepr. 50(1982)152-158.
12 NATIONAL WORKSHOP FOR COMMUNICATORS AND SOCIAL MOBILIZATION FOR THE CONTROL OF SEXUALLY TRANSMITTED DISEASES. The Madras declaration on sexually transmitted diseases (STDs) 20 September 1987. Swasth Hind 32(1988)114.
13. NOIREAU, F., BRUN -VEZINET, F., LAROUZE, B., NZOUKOUDI , M. Y. and GOUTEUX, J. P. Absence of relationship between human immunodeficiency virus 1 and sleeping sickness. Trans. R. Soc. Trop. Med. Hyg. 81(1987)1000.
14. NUTI, M., DEFELICI, A., VON AXELL CASTELLI , I. and ROSCIGNO, G. False HIV positivity in leprosy. (Abstract) Int. J. Lepr. 57 Suppl.(1989)366.
15. PASS , R. F. Epidemiology and transmission of cytomegalovirus. J. Infect. Dis. 152 (1985) 243-248.
16. QUINN, T. C, PIOT, P., MCCORMICK, J. B., FEINSOD, F. M., TAELMAN, H., KAPITA, B., STEVENS, W. and FAUCI, A. S. Serologic and immunologic studies in patients with AIDS in North American and Africa. The potential role of infectious agents as cofactors in human immunodeficiency virus infection. JAMA 257(1987)2617-2621.
17. RABINOWITZ, M., BASSAN, I. and ROBINSON, M. S. Sexually transmitted cytomegalovirus proctitis in a woman. Am. J. Gastroenterol. 83(1988)885-887.
18. RAO, K. N., LAKSHMI, V. and SAHA, K. Undernutrition in lepromatous leprosy, Part I. Is it associated with poverty or with disease? Lepr. Rev. 57(1986)299-309.
19. RAO, K.. N., SAHA, K., BHATIA, V. N. and GADI, S. Toxoplasma gondii antibody in patients of lepromatous leprosy. Jpn. J. Med. Sei. Biol. 42(1989)163-168.
20. SAHA, K., BHATNAGAR, A., SHARMA, V. K. and CHAKRABARTI, A. K. Enzyme immunoassay of serum B-2-microglobulin levels in various histological forms of leprosy with special reference to its elevation in type 1 and type 2 lepra reaction. J. Clin. Microbiol. 21(1985)658-661.
21. SAHA, K. and RAO , K. N. Undernutrition in lepromatous leprosy. V. Severe nutritional deficit in lepromatous patients co-infected with pulmonary tuberculosis. Eur. J. Clin. Nutr. 43 (1989) 117-128.
22. SAHA, K., SEHGAL, V. N. and SHARMA, V. High incidence of IgG class of Epstein-Barr virus capsid antibody in Indian patients of lepromatous leprosy. Trans. R. Soc. Trop. Med. Hyg. 76(1982)311-313.
23. SAXON, A. and C AMPEN , V. AIDS: State of the art, spring 1988. J. Allergy Clin. Immunol. 81(1988)796-802.
24. SCHACHTER , J. Chlamydia trachomatis infections: epidemiology and disease spectrum. Recent Advances in Sexually Transmitted Diseases. Oriel, J. D. and Harris, J. P. W., eds. New York: Churchill Livingstone, 1986, pp. 39-58.
25. SETH , P., PRAKASH, S. S. and GHOSH, D. Anti-bodies to herpes simplex virus types 1 and 2 in patients with squamous cell carcinoma of uterine cervix in India. Int. J. Cancer 22(1978)708-712.
26. SHIV RAJ, L, PATIL, S. A., GIRDHAR, A., SENGUPTA, U., DESIKAN, K. V. and SRINIVASAN, H. Anti-bodies to HIV-1 in sera from patients with mycobacterial infections. Int. J. Lepr. 54(1989)546-551.
27. TURK , J. L. and REES, R. J. W. AIDS and leprosy. (Editorial) Lepr. Rev. 59(1988)193-194.
28. WHO EXPERT COMMITTEE ON VENERAL DISEASES AND TREPONEMATOSES. Sixth report. Geneva: World Health Organization, 1986. Tech. Rep. Ser.736
1. M.Sc, M.B.B.S., Ph.D., Department of Immunology, Vallabhbhai Patel Chest Institute, University of Delhi, Delhi 110007.
2. M.Sc, Department of Immunology, Vallabhbhai Patel Chest Institute, University of Delhi, Delhi 110007.
3. M.B.B.S., M.D., Division of Microbiology, National Institute of Communicable Diseases, Delhi 110054.
4. M.B.B.S., Department of Medicine, Medical College, Silchar.
5. M.B.B.S., D.V.D., Lotts Carey Baptist Mission, 5 Daryaganj, Delhi 110002.
6. M.V.Sc, D.Sc. (France), Cytology Research Centre, Indian Council of Medical Research, New Delhi 110002.
7. M.Sc, Ph.D., Cytology Research Centre, Indian Council of Medical Research, New Delhi 110002.
8. M.B.B.S., M.D., Department of Dermatology, Ram Manohar Lohia Hospital, New Delhi 110001, India.
Received for publication on 9 November 1989
Accepted for publication in revised form on 18 May 1990.