- Volume 58 , Number 4
- Page: 724–5
Trichosporon beigelii infection in Hansen's disease
To The Editor:
Fungi of the genus Trichosporon are known to cause superficial mycetic infections (white piedra) characterized by the presence of hard nodules along the hair. White piedra is reported to be present mostly in temperate and tropical regions, and one case has been reported from India (1,3). We report isolation of Trichosporon beigelii from a long-standing ulcer over an anesthetic Hansen's lesion.
A 60-year-old male with lepromatous leprosy of 20 years duration presented with a nonhealing ulcer of 3 years duration over the anterior aspect of the right ankle. The ulcer was present over the anesthetic skin. Measuring 3 cm in diameter with necrotic debris in the floor, with an indurated base and raised hyperkeratetic margins, the ulcer was biopsied to rule out fungal infection or malignancy. A culture of scrapings from the margin of the ulcer grew Trichosporon beigelii. The yeast phase of this organism is seen in the dermis (Fig. 1). The fungus grew on Sabouraud dextrose agar (SDA) without antibiotics (Fig. 2), microscopically showing blastospores and arthrospores (Fig. 3) (4).
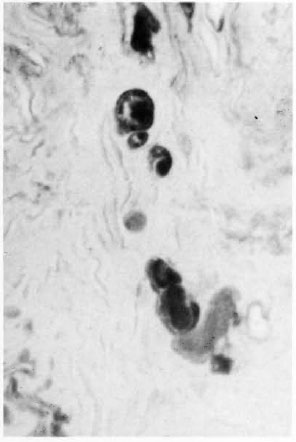
Fig. 1. Skin biopsy showing yeast phase of T. beigelii in the dermis (hematoxylin and eosin, × 400).
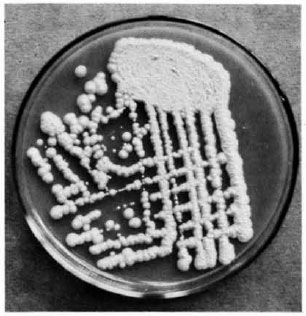
Fig. 2. T. beigelii, soft, wrinkled, off-white colonies on Sabouraud dextrose agar without antibiotics.

Fig. 3. Arthrospores and blastospores (Gram stain, × 400).
Trichosporon beigelii, formerly known as Trichosporon cutaneus, is an inhabitant of the soil and is occasionally found on normal human skin. Twelve cases of invasive disease, either localized or disseminated, have been reported (4). The infections involved are almost all opportunistic and occur as the result of a barrier break or in patients with some degree of immunodeficiency, physiologic imbalance, or disruption of the normal resident fungal and bacterial flora (4). Eradication of this cutaneous infection is difficult although amphotericin B, 5-fluorocytesine, and ketoconazole have been advocated for treatment for their possible synergistic effect (2). Spontaneous remission may occur in many cases once the underlying systemic disease is controlled, as in our patient.
- Rama Ramani, M.D.
Chakravarthy R. Srinivas, M.D.
Ambarish Padhee, M.D.
P. G. Shivananda, M.D., Ph.D.
Departments of Microbiology, Dermatology and Venereology, and Pathology
Kasturba Medical College
Manipal 576119
Karnataka, India
REFERENCES
1. BASU, N., SANYAL, M., BANERJEE, A. K. and THAMMAYYA, A. White piedra in India, case report. Indian J. Dermatol. Venercol. 36(1970)154-155.
2. KALTER, D. C, TSCHEN, J. A., CERNOCH, P. L., MCBRIDE, M. E., SPERBER, J., BRUCE, S. and WOLF, J. E., JR. Genital white piedra: epidemiology, microbiology and therapy. J. Am. Acad. Dermatol. 14(1986)982-993.
3. MOHAPATRA, L. N. Study of medical mycology in India; an overview. Indian J. Med. Res. 89(1989)351-361.
4. RIPPON, J. W. Medical Mycology: The Pathogenic Fungi and The Pathogenic Actinomycctcs. Philadelphia: W. B. Saunders Co., 1982, pp. 151-152, 559-563.