- Volume 57 , Number 4
- Page: 794–800
Specific anti-M. leprae PGL-I antibodies and mitsuda reactions in the management of household contacts in New Caledonia
ABSTRACT
Household contacts of leprosy patients have been tested for anti-phenolic glyco-lipid-I IgM antibodies (anti-PGL-I IgM) by an ELISA using the natural disaccharide (NDO) and natural trisaccharide (NTO) synthetic antigens. A group of healthy subjects without known exposure to Mycobacterium leprae served as controls. The percentages of positivity observed in multibacillary patients, paucibacillary patients, and household contacts were significantly higher than those of the negative controls. The absorbancc values using NDO and NTO correlated well (range 0.59-0.91) when analysis of each subject group was performed. As reported here, NDO and NTO antigens seem to be equal in detecting leprosy cases; 100% of multibacillary and 21.43% of paucibacillary cases were detected as seropositive. For the screening of household contacts, NDO appears to be more sensitive and NTO more specific . There were more seropositive cases in the young age groups of household contacts, suggesting a higher rate of transmission of M. leprae infection in those age groups. Lepromin and anti-PGL-I IgG tests were also performed in contacts who were followed. The 2 paucibacillary subjects (1 borderline tuberculoid, 1 indeterminate) were Mitsuda negative. At diagnosis, their anti-PGL-I IgM levels were much higher than those of previous results; their anti-PGL-I IgG levels showed an increase in one and a decrease in the other. However, for lhe entire group anti-PGL-I IgM and anti-PGL-I IgG leveis were posi-tively correlated. The data reported here suggest that an increase in specific anti-M. leprae IgM leveis in Mitsuda-negative household contaets could revcal the devel-opment of overt disease.RÉSUMÉ
On a eu recours à des épreuves ELISA utilisant des antigènes synthétiques du disaccharide naturel (NDO) et du trisaccharide naturel (NTO) pour étudier les anticorps anti-phenoglycolipidiques-I (Anti-PGL-I IgM) chez des contacts domiciliaires de malades de la lèpre. Des individus sains sans exposition connue à Mycobacterium leprae ont servi de témoins. Les proportions de réactions positives observées chez des malades respectivement multibacillaires. paucibacillaires, et domiciliaires, étaient significativement plus élevées que celles relevées chez les témoins négatifs. Les valeurs d'absorption avec NDO et NTO présentaient une bonne corrélation (de 0.59 à 0,91), lorsqu'on procédait à l'analyse de chaque groupe. Les antigènes NDO et NTO paraissent avoir la même valeur pour déceler les malades de la lèpre; 100% des cas multibacillaires et 21,43% des cas paucibacillaires étaient délectés comme séropositifs. En vue d'étudier les contacts domiciliaires, le NDO parait plus sensible et le NTO plus spécifique. On a noté davantage de cas séropositifs dans les groupes d'âge jeune parmi les contacts domiciliaires, ce qui suggère un taux beaucoup plus élevé de transmission de M. leprae dans ce groupe. On a également procédé à des épreuves anti-PGL-I IgG chez des contacts, dont on a suivi ensuite l'évolutionn. Les deux sujets paucibacillaires (1 malade tuberculoïde dimorphe et un malade atteint de forme intermédiaire) étaient négatifs à l'épreuve Mitsuda. Lors du diagnostic, leurs taux d'anti-PGL-I IgM étaient beaucoup plus élevés que ceux relevés lors d'observations antérieures. Les taux d'anticorps anti-PGL-I IgG présentaient une augmentation chez l'un et une diminution chez l'autre. Néanmoins, les taux d'anticorps anti-PGL-1 IgM et anti-PGL-I IgG montraient chez ces malades une corrélation positive. Les données relatées ici suggèrent qu'une augmentation des taux spécifiques anti-M. leprae chezdes contacts domiciliaires négatifs à l'épreuve Mitsuda, pourraient révéler le développement clinique de la maladie.RESUMEN
Se buscaron anticuerpos IgM anti-glicolipido fenó-lico-I (IgM anti PGL-I) en el suero de convivientes de pacientes con lepra, usando un inmunoensayo enzimático (ELISA) con los antígenos sintéticos correspondientes al disacárido natural (NDO) y al trisacái-do natural (NTO). Como control se usó un grupo de individuos sin exposición conocida al Myeobacterium leprae. Los porcentajes de positividad observados en los pacientes multibacilares, en los paucibacilares y en los convivientes, fueron significativamente mayores que aquellos de los controles negativos. Cuando se hizo el análisis de cada grupo de sujetos, los valores de ab-sorbancia usando NDO y NTO mostraron una buena correlación (rango 0.59-0.91). Los antígenos NDO y NTO parecen funcionar igual en la detección de casos de lepra; 100% de los casos multibacilares y 21.43% de los casos paucibacilares fueron detectados como seropositivos. Para el tamizaje de los contactos convivientes, NDO parece ser más sensible y NTO más específico. Hubieron más casos seropositivos en los grupos de convivientes jóvenes, sugiriendo un mayor grado de transmisión de la infección por M. leprae en esos grupos. También se hicieron la prueba de la le-promina y la búsqueda de anticuerpos IgG anti-PGL-I en los contactos estudiados. Los dos sujetos paucibacilares (uno intermedia tuberculoide y el otro intermedio) fueron Mitsuda negativos. Cuando se hizo el diagnóstico, sus niveles de anticuerpo IgM anti-PGL-I fueron mucho mayores que los de resultados previos mientras que sus niveles de IgG anti-PGL-I mostraron un incremento en uno y una disminución en el otro. Sin embargo, para el grupo total, los niveles de anticuerpos IgM e IgG anti-PGL-I estuvieron positivamente correlacionados. Los datos reportados aquí, sugieren que el incremento en los niveles de IgM específicos contra M. leprae en los convivientes Mitsuda negativos, podría revelar el desarrollo de la enfermedad abierta.Serological assays in leprosy research are very important, particularly for early diagnosis (3,6,7,12,13). Several tests, using different antigens, have been carried out to detect specific anti-Mycobacterium leprae antibodies (1,2,5,7,15,16); the most widely studied has been phenolic glycolipid-I (PGL-I). The antigenicity is determined by the terminal glycosides (trisaccharide and di-saccharide) (10,11). More recently, the following antigens-natural disaccharide oc-tyl-bovine serum albumin (BSA) (NDO), natural trisaccharide octyl-BSA (NTO), natural trisaccharide phenyl-BSA (NTP)- have been synthesized (9). Several studies testing these neoglycoproteins have revealed that all are highly sensitive and specific for the detection of IgM antibodies in multibacillary (MB) patients (7,9,10). Some authors have shown that the trisaccharide antigens (NTO, NTP) are better for 'detection of IgM antibodies in paucibacillary (PB) patients (7,10). But, whatever the antigen used, IgM antibodies are detected in only 30%-50% of PB cases. Nevertheless, serological tests could be useful to detect the population at risk of developing a lepro-matous form of leprosy in the household contact population.
In New Caledonia, Hansen's disease is endemic with a prevalence rate of 3.51/1000, an incidence rate of 0.15/1000, and a lep-romatous index of 2.38%. Leprosy affects mainly the Melanesian people, and longitudinal studies in Melanesian household contact populations are essential to define populations at risk. This study reports on results of anti-PGL-I detection by an ELISA using NDO and NTO antigens in 309 Melanesian household contacts.
MATERIALS AND METHODS
Patients. This study included five subject groups: a) 309 Melanesian household contacts; b) 14 Melanesian untreated PB patients classified as tuberculoid (TT), borderline tuberculoid (BT), indeterminate (I) according to the criteria of Ridley and Jop-ling (15); c) 13 Melanesian untreated MB patients classified as borderline leproma-tous, lepromatous (BL-LL) according to the same criteria; d) 104 negative controls belonging to the same ethnic group but without known exposure to M. leprae (from an area with no leprosy cases); and e) 23 active pulmonary tuberculosis patients. Seventeen household contacts were tested several times and had a lepromin test performed.
Lepromin test. A lepromin test (Mitsuda reaction) was conducted using lepromin A provided by the World Health Organization (Dr. Robert Hastings, GWL Hansen's Disease Center, Carville, Louisiana, U.S.A.). The test was considered as positive when the diameter of the papule was > 4 mm.
ELISA. The ELISA method described by Cho, et al. (8) was used with minor modifications: Flat-bottom micro-ELISA plates (Immulon; Dynatech, Cambridge, Massachusetts, U.S.A.) were coated overnight at 37ºC in a moist chamber with NDO and NTO antigens. Concentrations of antigens (NDO, NTO) and peroxidase-labeled goat anti-human μ-chain antibodies were determined by titration against a pool of lepromatous sera giving an absorbance value of 1.700 at 492 nm. The sera were diluted 1:250 in phosphate buffered saline-Tween 20-bovine serum albumin (PBS-T-BSA; 94.9:0.1:5) and tested in duplicate against each antigen and against control wells coated with BSA alone.
Pools of sera from untreated lepromatous patients and sera from healthy subjects without known contacts with leprosy patients were included as controls in each series. The optical density (OD) was read at 492 nm in a Titertek Multiskan reader. Anti-PGL-I IgM was expressed as ΔOD (ΔOD = NDO OD or NTO OD minus BSA OD). The threshold of positivity was determined as the mean ΔOD obtained from negative controls plus two standard deviations (S.D.).
Specific anti-PGL-I IgG detection was carried out using a similar method for the 17 household contacts who have been followed.
Statistical analysis. The means and standard deviations were calculated for each group (household contacts, MB patients, PB patients, tuberculosis patients, and negative controls). Percentages of positive results were established for each method of testing (NDO, NTO) and compared by a chi-squared test. For each subject group, a comparison of results obtained with NDO and NTO was also performed by a chi-squarcd test. Correlation coefficients (r) and regression lines for IgM levels between the NTO and the NDO assays were determined using the least-square method in the household contacts, MB patients, and PB patients groups.
The levels of anti-PGL-I IgM and anti-PGL-I IgG seropositivity in the household contacts who were tested multiple times were compared using a two-tailed chi-squared test. The relationship between the anti-PGL-I IgM and anti-PGL-I IgG levels was assessed by the calculation of a correlation coefficient.
RESULTS
Serological activity of different groups tested. As shown in Table 1, MB patients displayed a higher antibody activity than did the other groups. Detectable IgM antibodies were found in 100% of MB cases and 21.4% of PB cases with NDO or NTO antigens. In the other groups, smaller percentages of positivity were found using NTO antigen as compared to NDO antigen, but they were not significantly different.
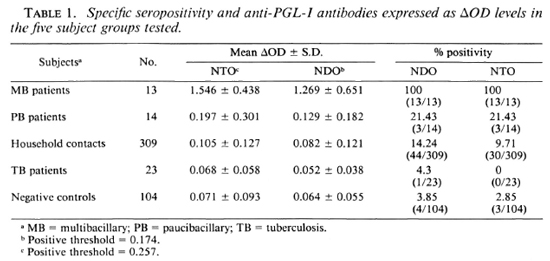
For each method of testing, the distribution of seropositive subjects was significantly higher in MB patients than in PB patients (p < 0.001). Multibacillary patients showed very high levels of positivity compared to negative controls (p < 10-9). The percentages observed in PB patients and household contacts were significantly different from that of negative controls (p < 0.05). There was no significant difference between tuberculosis patients and negative controls.
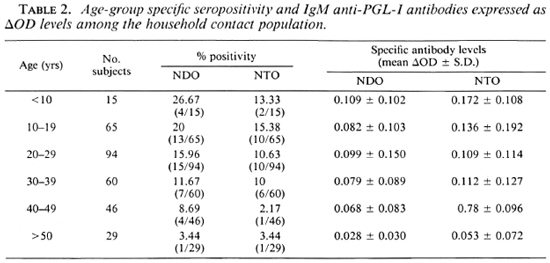
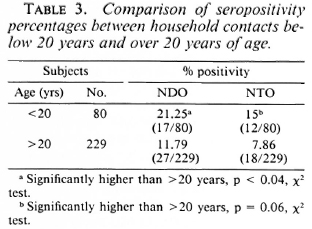
Percentages of seropositivity were higher among the young household contact age groups. The mean specific antibody levels and seropositivity declined slowly with an increase in age (Table 2). There were significantly higher percentages of positivity among young people when household contacts were grouped as contacts below 20 years and contacts over 20 years of age (Table 3).
Correlation between NTO/NDO antigens. The correlation of the absorbance values between the NTO and the NDO antigens and regression lines were calculated in 309 household contacts, 14 MB patients, and 13 PB patients. The correlation coefficient was lower in the household contacts (r = 0.57, y = 0.593x + 0.057) than in leprosy patients (PB patients: r = 0.91, y = 1.510x + 0.003; MB patients: r = 0.85, y = 0.570x + 0.822). However, all of the correlations were highly significant (p < 0.001).
Follow up of contacts. Among the contact population, 17 subjects were followed for detection of anti-PGL-I IgM and anti-PGL-I IgG using the NTO antigen (anti-NTO IgM, anti-NTO IgG), and tested for the Mitsuda reaction at the second sample. They were bled intermittently during the 3 years following the first sample. The mean interval between two samples was 25 months (range 3-36 months). Details are reported in Table 4. As shown in The Figure, 11 contacts had a positive lepromin test. In this group, 5 subjects were seronegative for anti-NTO IgM at the first sample: at the second sample, 4 had remained seronegative and 1 had become seropositive (with low antibody levels). The 6 other subjects were seropositive at the first test; 5 of them were seronegative at the second test, 1 remained seropositive. None of these subjects developed overt leprosy during the study period.

The Figure. Follow up of anti-NTO IgM and Mit-suda reaction in 17 Melanesian household contacts; (---) = seropositivity threshold (ΔOD = 0.298).
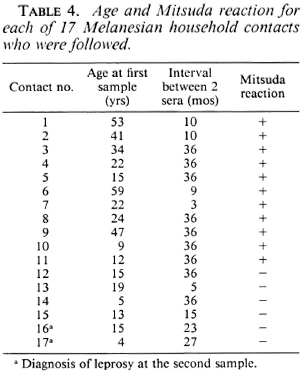
The six other subjects were found to be lepromin negative at the second sample. In this small group, four subjects were seropositive at the first sample, two of them with high antibody levels (ΔOD - 1). At the second sample, three were still seropositive and one of them had developed an indeterminate form of leprosy. Among the two subjects who were initially seronegative, one remained seronegative and healthy, the second became strongly seropositive and developed BT leprosy.
The results observed with the anti-NTO IgG screening showed a significant positive correlation with the anti-NTO IgM levels (r = 0.49, p < 0.01). However, smaller percentages of detectable specific IgG antibodies (11.76%) were found compared to percentages of detectable specific IgM antibodies (47.06%) (p < 0.001).
During the study, two subjects developed a clinical form of leprosy: one showed an increase in anti-NTO IgG and IgM (patient no. 17, indeterminate), the other a decrease in anti-NTO IgG levels and an increase in anti-NTO IgM (patient no. 16, BT).
DISCUSSION
Leprosy remains a public health problem in the South Pacific. High prevalences are found in Papua New Guinea (3) and in the northern latitudes of Australia (4). Some islands such as New Caledonia and French Polynesia (6) do not have as many cases (incidence rate = 0.15/1000 in New Caledonia, 0.08/1000 in French Polynesia).
Synthetic antigens and deacylated PGL-I are very useful for detecting MB patients (5-7), but in the PB forms detection is not so efficient. Buchanan, et al. (5) have found 50% seropositive PB cases using the ELISA procedure for IgM antibodies to deacylated PGL-I. Chanteau, et al. (6) found only 5% seropositive PB cases with NDO antigen in Polynesian patients. The results of the present study are intermediate with a detection rate of 100% in MB and of only 21.4% in PB cases.
Among the contact populations, only a small proportion of those exposed to M. leprae will go on to develop the disease, so serological tests are particularly recommended for screening populations at risk. In New Caledonia 14.2% (using NDO antigen) and 9.7% (using NTO antigen) of the tested household contacts had detectable anti-PGL-I IgM antibodies. This is lower than in Papua New Guinea, where 32% of contacts were positive (3) when tested against the whole PGL-I. The results in New Caledonia are similar to those in French Polynesia (19.5% seropositive contacts with NDO and 10.2% seropositive contacts with NTO). Asworth, et al. (1), using a competition radioimmunoassay test with a monoclonal antibody to the 35-kDa protein of M. leprae, have found 6% positivity among the contact population of an endemic area in India, with a prevalence rate of 8/1000. They did not show correlation between antibody positivity of contacts and exposure to a MB case. In the present study, relation to the index case was not studied because of the Melanesian people's way of life. Their tribal system does not allow the differentiation between contacts related to MB and PB cases.
The results in Tables 2 and 3 show that the transmission of M. leprae infection is taking place mostly among the young age groups of household contacts.
As reported here, NDO and NTO antigens seem to be equally effective in detecting leprosy cases. For screening of household contacts, NDO appears to be more sensitive (higher percentages of positivity) and NTO more specific (lower percentages of positivity observed in negative controls). The correlations observed between the NTO and the NDO antigens were highly significant in all groups tested. The correlation coefficients (ranging from 0.85 to 0.91) in leprosy patients are similar to those observed in French Polynesia (7). In household contacts, the correlation coefficient is lower than in French Polynesia, perhaps due to the very low levels of absorbance values observed in Melanesian contacts as compared to Polynesian contacts.
One of the purposes of this study was to attempt to define populations at risk of developing leprosy in household contacts. The method used is the screening of high-risk contacts by specific serology and the evaluation of cell-mediated immunity. Assessment of cellular immunity was realized by the Mitsuda test. As observed here, the majority of household contacts were Mitsuda positive. Among the Mitsuda-negative subjects, two have developed the disease. It seems that a negative Mitsuda response indicates an individual at risk of developing clinical leprosy.
The presence of significant antibody levels is not predictive of the clinical outcome (the prevalence rate of leprosy in the contact population was less than the seropositivity rate in the contact population). Seropositivity was often transient, especially in subjects who developed cellular immunity. This is in line with the notion developed by Reich (14). The leprosy bacillus is not difficult to transmit and the majority of the population incubate subclinical infection at various levels. Regarding specific anti-M. leprae IgM and IgG detection, it was shown that IgM specific antibodies are more often detected than IgG specific antibodies. Similar results on leprosy patients have also been reported (11). In the course of the study, two patients have developed a clinical form of leprosy. They each had an increase in their IgM anti-PGL-I levels. On the other hand, anti-PGL-I IgG increased in one case and decreased in the other case. Levis, et al. (12) have reported that anti-PGL-I IgG detection may be indicative of an increased cell-mediated immune response in leprosy patients. The results observed here did not allow any conclusion regarding this hypothesis.
In short, a negative Mitsuda response among contacts puts them at increased risk of developing clinical leprosy. For them, it would be of interest to study the variation of specific anti-M. leprae IgM levels in a long-time follow up (in addition to a clinical survey) in order to define the critical threshold related to the development of the clinical disease.
Acknowledgments. The authors are grateful to Professor P. J. Brennan, Colorado State University, Fort Collins, Colorado, U.S.A., and the National Institute of Allergy and Infectious Diseases. National Institutes of Health, Contract no. 1A1 -52582. for providing NTO and NDO antigens, and to L. Massenet for her technical assistance.
REFERENCES
1. Asworth, M., Sinha. S., Patil. S. A., Ramu, G. and Sengupta. U. The detection of subclinical leprosy using a monoclonal antibody based radioimmunoassay. Lepr. Rev. 57(1986)237-242.
2. Bach, M. A. Anticorps anti-M. leprae et sérologie de la lèpre. Acta Leprol. (Genève) 4(1986)331-341.
3. Baumgart. K., Britton, W., Basten, A. and Bagshawe, A. Useofphenolicglycolipid forsero-diagnosis of leprosy in a high prevalence village in Papua New Guinea. Trans. R. Soc. Trop. Med. Hyg. 81(1987)1030-1032.
4. Boughton, C. R. and Lloyd, A. R. The management of leprosy. Med. J. Aust. 146(1987)593-599.
5. Buchanan, T. M., Young, D. B., Miller, R. A. and Khanolkar. S. R. Serodiagnosis of infection with Mycobacterium leprae. Int. J. Lepr. 51(1983)524-530.
6. Chanteau, S., Cartel, J. L., Guidi, C, Plichart, R. and Bach, M. A. Seroepidemiological study on 724 household contacts of leprosy patients in French Polynesia using disaccharidc-octyl-BSA as antigen. Int. J. Lepr. 55(1987)626-632.
7. Chanteau, S., Cartel, J. L., Roux, J., Plichart, R. and Bach, M. A. Comparison of synthetic antigens for detecting antibodies to phenolic gly-colipid I in patients with leprosy and their household contacts. J. Infect. Dis. 157(1988)770-776.
8. Cho, S.-N., Yanagihara, D. L., Hunter, S. W., Gelber, R. H. and Brennan, P. J. Serological specific ity of phenolic glycolipid-I from Mycobacterium leprae and use in serodiagnosis of leprosy. Infect. Immun. 41(1983)1077-1083.
9. Fujiwara, T., Hunter, S. W., Cho, S.-N., Aspin-all, G. O. and Brennan, P. J. Chemical synthesis and serology of disaccharides and trisaccharides of phenolic glycolipid antigens from leprosy bacillus and preparation of a disaccharide protein conjugate for serodiagnosis of leprosy. Infect. Immun. 43(1984)245-252.
10. Gaylord, H. and Brennan, P. J. Leprosy and the leprosy bacillus: recent developments in characterization of antigens and immunology of the disease. Ann. Rev. Microbiol. 41(1987)645-675.
11. Koster, F. T., Scollard, D. M., Umland, E. T., Fishuein, D. B., Hanly, W. C, Brennan, J. P. and Nelson, K. E. Cellular and humoral immune response to a phenolic glycolipid antigen (PhenGL-I) in patients with leprosy. J. Clin. Microbiol. 25(1987)551-556.
12. Levis, W. R., Meeker, H. C, Schuller-Levis, G. B., Gillis, T. P., Marino, L. J. and Zauriskie, J. Serodiagnosis of leprosy: relationships between antibodies to Mycobacterium leprae phenolic gly-colipid-I and protein antigens. J. Clin. Microbiol. 24(1986)917-921.
13. Menzel, S., Harboe, M., Bergsvik, H. and Brennan, P. J. Antibodies to synthetic analog of phenolic glycolipid-I of Mycobacterium leprae in healthy household contacts of patients with leprosy. Int. J. Lepr. 55(1987)617-625.
14. Reich, C. V. Leprosy: cause, transmission, and a new theory of pathogenesis. Rev. Infect. Dis. 9(1987)590-594.
15. Ridley, D. S. and Jopling, W. H. Classification of leprosy according to immunity; a five-group system. Int. J. Lepr. 34(1966)255-273.
16. Roy, A. Serological study of leprosy employing ELISA with arabinogalactan of Mycobacterium smegmatis as antigen. Lepr. Rev. 57(1986)137-145.
1. Biological Pharmacist; Institut Pasteur de Nouméa, B.P. 61, Nouméa, New Caledonia.
2. M.D.; Institut Pasteur de Nouméa, B.P. 61, Nouméa, New Caledonia.
3. M.D.; Institut Pasteur de Nouméa, B.P. 61, Nouméa, New Caledonia.
4. M.D., Institut Pasteur de Nouméa, B.P. 61, Nouméa, New Caledonia.
5. M.D., Dispensaire anti-Hansénicn, Nouméa, New Caledonia.
6. M.D.Sci., Unité de Pathologie de l'Immunité, Institut Pasteur de Paris, Paris, France.
Reprint requests to S. Desforges.
Received for publication on 27 February 1989.
Accepted for publication in revised form on 30 June 1989.