- Volume 57 , Number 4
- Page: 834–43
Prospects for new generation vaccines for leprosy: progress, barriers, and future strategies
The First Vaccilep Workshop on the Immunology of Leprosy was held in Anan-daban, Nepal, 29-31 March 1989. Despite the availability of effective chemotherapy for the past three decades, leprosy remains a major public health problem in many areas of the world. An antileprosy vaccine is considered a compelling alternative to interrupt transmission and lead to the eventual eradication of the disease. Many individuals can mount a protective immune response to infection by Mycobacterium leprae, and do not develop disease. Individuals in whom mycobacteria evade the protective host response in various ways are at risk in terms of clinical leprosy. These individuals pose a particular problem when considering vaccine development since they may not respond adequately to simple vaccines. This question and other issues were debated by the 38 participants who reviewed recent progress in understanding the immunology of leprosy and considered future strategies to overcome the barriers to developing new vaccines for prophylactic and therapeutic use.
Progress in basic knowledge
Antigens of M. leprae. The cloning of the genome of M. leprae as a λgt11 expression library 1 has had a major impact on leprosy research since it has led to the identification of a number of recombinant proteins which react with monoclonal antibodies developed using sonicates of whole M. leprae.1 A series of proteins known by their Mr values, the 70, 65, 36, 30/31, 28 and 18-kDa antigens, have been identified and their B and T epitopes are now being determined with a view to examining their potential as diagnostic and vaccine candidates. A summary of the structure and function of these protein antigens that emerged from the First Vaccilep Workshop can be found elsewhere.3 Attention was focussed on identifying epitopes for two reasons. First, M. leprae-specific B-cell epitopes may offer diagnostic potential, particularly for early infection. Second, T-cell epitopes cross-reactive to a number of mycobacteria may have a wider role in the development of a general anti-mycobacterial vaccine. In this regard, the crossreactive epitopes of the 70-kDa and 65-kDa protein antigens would appear to be the prime candidates.4,5
T-cell-mediated immunity is the basis of protection against M. leprae, but the above proteins were initially defined by murine monoclonal antibodies. Therefore, it is important to continue to search for other protein antigens. Three strategics have recently been developed. Three groups6-8 have fractionated protein antigens from sonicated M. leprae on the basis of molecular weight and tested them for cellular reactivity in leprosy patients and their contacts. This approach has defined additional putative T-cell antigens which were not previously recognized. Although there is considerable individual variation in the antigens recognized, M. leprae antigens of Mr 19-22, 35-40 and 65-kDa8 and 11-16 and 22-26-kDa7 were important in two studies. A common finding was that some lepromatous leprosy patients or contacts who were unresponsive to whole soluble sonicate responded to particular fractions, suggesting that a "suppressor" constituent of the soluble leprosy antigen had been removed. A second approach is to purify protein antigens from large quantities of M. leprae by chemical means. Recently, Hunter, Mehra, and co-workers9,10 have defined a cell-wall-associated protein complex which is highly immunoreactive with human T-cell clones. This complex appears to contain proteins of Mr 7, 16, and 28 kDa in addition to traces of the 65-kDa protein. A third approach is to use M. leprae-reactive T-cell clones to screen the M. leprae DNA library and by these means, one new antigen has been identified.11
Understanding T-cell function. T cells in the periphery bear the CD3 marker and most bind to antigenic peptides in the context of major histocompatibility complex (MHC)-encoded molecules.12 These T cells segregate into two nonoverlapping T-cell sets of reciprocal phenotype. CD4 T cells recognize antigenic peptides plus MHC class II molecules, whereas CD8 T cells are specific for peptides plus MHC class I molecules. Antigen recognition is a function of a specific T-cell receptor (TcR) which in both cell types is composed of an alpha (α) and a beta (β) chain.13 There is growing interest in a small percentage of peripheral T cells which lack both the CD4 and CD8 markers and use a different TcR composed of a gamma (γ) and delta (δ) chain, which is normally lost in most T cells early during development in the thymus.13,14 These γ/δ T cells are less stringent in their antigen specific ity and genetic restriction than the more common αβreceptor-bearing T cells. These γ/δ T cells appear to bind some mycobacterial antigens which belong to the conserved family of heat-shock proteins, but their role in immunity is unclear.14
The two major effector functions of α/β cells are T-cell help (both for antibody production and the activation of macrophages by cytokines) and direct cytolysis. Helper-T cells (Th cells) secrete a variety of cytokines including (interleukin-2) IL-2, IL-3, IL-4, IL-5, IL-6, and (gamma-interferon ) IFN-γ.13 In most cases Th cells are CD4, although some CD8 T cells can also provide help. Cytolytic-T cells (CTL), which are mostly CD8, lyse their target cells by direct cell contact.14 Some CD4 T cells can express cytolytic function as can CD8 γ/δ T cells.
Murine helper-T cells have been divided into two subpopulations, Th1 and Th2, based on cytokine secretion patterns,15-16 but this separation is not so clear cut in human T cells. The functional significance of these observations appears to lie in two directions: the ability of Th cells to both promote and inhibit cell-mediated and humoral immunity, and the biological activities of cytokines. Areas of importance to leprosy lie in analyzing the effects of cytokines on macrophages, leading to increased killing of intracellular parasites, and in enhancing cytotoxicity of killer-T cells.
Until recently, the CD4 Th cells have been considered the major T-cell type mediating protective immunity against mycobacteria. In vitro studies using human lymphocytes demonstrated that M. leprae-specific CD4 T cells released IL-2 and IFN-γ which activated anti-mycobacterial functions in infected macrophages.16 This has now been complemented by elegant immunohisto-chemical studies showing the predominance of activated CD4 cells in tuberculoid skin lesions and their paucity in lepromatous lesions.17 However, experimental studies in mice infected with M. tuberculosis and M. lepraemurium suggest that both CD4 and CD8 T cells may have a role in protection.16 These studies highlight the contribution that accessible laboratory models using other mycobacteria make to our understanding of leprosy. Mice selectively depleted of CD8 T cells are more susceptible to mycobacterial infection. Thus, CD8 cells which lyse infected host macrophages can also be regarded potentially as both protective and harmful. Lysis of the infected host cells may reduce bacterial growth by destruction of the cellular habitat of the obligate intracellular pathogen, but this benefit could be at the cost of damaging host tissue, such as the infected Schwann cell. Thus, both responses, while protective, may lead to inflammatory reactions which aggravate the pathway of clinical disease.
The importance of cytolytic responses has been supported by the recent demonstration of M. leprae-specific CTL in man, but these were of the CD4 phenotye.18,19 Further, in studies of the effects of intralesional IFN and IL-2 in lepromatous leprosy patients, a prominent feature was the influx of cytolytic CD4 T cells which lysed the infected macrophages. Liberated bacilli were apparently phagocytosed and then destroyed by freshly recruited monocytes.20,21
The relevance of these findings to vaccine development is that any subunit or recombinant vaccine must be presented in a form capable of activating the correct T-cell subset or subsets that mediate protective immunity.
HLA and the immune response. A major function of the HLA class I and II molecules encoded by MHC genes is to present processed antigens to T cells and so activate them.22 Class I antigens, which are present on virtually all nucleated cells, bind to CD8 T cells. Class II antigens are restricted to cells of the immune system, especially dendritic cells and Langerhans' cells, macrophages and B cells and bind CD4 cells. For most protein antigens "processing" involves unfolding and/or cleavage of the protein into peptides which then bind to the highly polymorphic HLA class I and II molecules. This complex is then expressed on the surface of the cell and can react with the antigen receptor of the T cell. Binding of the peptides to HLA molecules shows a degree of specific ity in that certain peptides bind more strongly to certain alleles. This differential binding may explain the HLA-con-trolled differences in antigen-specific reactivity among different individuals.23
Because binding to HLA molecules is necessary for antigen recognition by T cells, the quantitative expression of HLA molecules may also exert a regulatory influence on immune responses. Schwann cells which normally express only class I HLA molecules can be induced to express class II HLA antigens on their surface. They could then act as antigen-presenting cells to the CD4 Th cells leading to immunopathology.
Susceptibility to and expression of leprosy is controlled by host genetic factors. Evidence for this comes from twin studies, pedigree analysis and genetic marker studies (particularly HLA) (reviewed in 23). Whereas the influence of HLA-linked genes appears to be predominantly on the type of leprosy developing in susceptible individuals, a marker for the hypothetical susceptibility gcnc(s) has not yet been identified. The molecular basis of HLA control of the immune response has been demonstrated using the 65-kDa mycobacterial protein. The response of human T-cell clones to nine separate epitopes on the protein was controlled by a single HLA-DR haplotype in each case.23 Subjects with different DR haplo-types respond to a different subset on epitopes of the protein. The implication for vaccine development is that proteins with a range of epitopes must be included in a vaccine to ensure that individuals with varying HLA phenotypes can respond to at least one epitope on the protein.
Nature of the immunological defect in lep-romatous leprosy. It is now apparent that there may be multiple reasons for the unresponsiveness to the antigens of M, leprae in lepromatous leprosy:24-26 a) The macrophages of some individuals may lack the ability to process the antigens of M. leprae. b) Peptides from the processed antigen may not bind to HLA molecules in the host cell, which are then unable to present the antigen to T cells, c) An individual may lack T cells that recognize key "protective" epitopes of M. leprae proteins, leading to a "hole" in the T-cell repertoire, d) Antigen processing may result in "inappropriate" antigen presentation leading to a T-cell-dcpendent inhibition of the anti-M. leprae response. At present the exact nature of suppressive phenomena in M. leprae infection is unclear, as are the epitopes and cells responsible. However, the interaction of Th 1 and Th 2 cells 15 must also be taken into account.
Suppressor-T cells have been difficult to demonstrate in the majority of lepromatous patients, although clones have been isolated from some leprosy patients.23,24 These clones inhibit M. leprae-specific T cells only, and their effects are restricted by HLA-DR molecules but not related to the CD4 or CD8 status of the cells involved. This antigen-specific suppression contrasts with the nonspecific inhibitory effects of mycobacterial lipoarabinomannan on T-cell responses.27
Issues in vaccine design
Unresponsiveness to vaccine. Subjects in an endemic region may fail to respond to vaccines for any of the mechanisms underlying hyporesponsiveness in lepromatous disease mentioned in the previous section. Therefore in the construction of a vaccine these potential problems must be considered to ensure that "susceptible" individuals are adequately immunized. Approaches to this include ensuring that a) each protein has a range of epitopes with a range of DR-restriction patterns, b) that putative suppressor epitopes be deleted from proteins, and c) a range of proteins is included so that subjects who lack responsive T cells for one protein are able to respond to other proteins. This emphasizes the need for extensive study of T-cell antigens in endemic populations before the inclusion of such proteins or epitopes in a molecularly defined vaccine.
Vaccine delivery. A number of delivery systems, including vaccinia and recombinant Salmonella, are being tested in other vaccine programs. Such vaccines expressing M. leprae antigens may be relevant to leprosy vaccine development by providing carriers for immunization rather than using recombinant proteins alone. Recent attention has focussed on the possibility that live attenuated BCG expressing "protective" M. leprae antigens may be a suitable carrier for human use. For example, Jacobs and coworkers have developed a shuttle plasmid which enables foreign DNA to be incorporated into a rapidly growing mycobac-terium 28 which will allow this possibility to be tested.
Goals of a new-generation vaccine. Because of the long incubation period of leprosy, the goals are: a) to elicit long-lasting protection from the leprosy bacillus in individuals prior to the transmission of M. leprae (prophylactic vaccine); b) to prevent the development of clinical leprosy in individuals already infected with M. leprae who may develop the disease (stabilizing vaccine); and c) to reverse the effects of the disease and accelerate self-healing in subjects with undiagnosed clinical disease (therapeutic vaccine).
These are different goals and may well require separate vaccines with distinct properties. However, in assessing the impact of a candidate vaccine in a community, these various effects must be considered. Vaccination in subjects with subclinical infection or undiagnosed disease may potentiate T-cell-mediated responses against infected host cells, resulting in immuno-pathology. This may precipitate clinical symptoms so that in the early years after vaccination there could be an increased incidence of clinical lesions. In the longer term, as susceptible subjects are protected from infection, the incidence of new cases should fall.
Assessing efficacy of new vaccines
Identifying new assays as predictors of subclinical or early infection. A persisting problem in assessing the effect of a vaccine is the ability to distinguish cases of subclinical infection from those who have been exposed and become immune. Initial assays for antibody to M. leprae did not attain the desired specific ity to detect the low bacillary load in tuberculoid leprosy.29 The development of M. leprae-specific antibody assays followed the purification of a novel phenolic glycolipid (PGL-I)30 and synthesis of the immunodominant terminal sugars.31 Although these antigens can be synthesized in pure form and reasonable amounts, there is still a need to develop synthetic peptide antigens for M. leprae-specific epitopes of known protein antigens to complement inhibition assays which detect antibodies to specific epitopes, for example, on the 35-and 36-kDa proteins.32 In this way, it is hoped that better diagnostic tests will become available for patients at the tuberculoid end of the clinical system.
Thus far, investigations using synthetic antigens to detect early infections have been conducted in three endemic regions, Malawi,33 Ethiopia,34 and French Polynesia.35
The results of these emphasize the need to standardize methodology and internal standards among investigators before the predictive value of serological responses in subclinical disease can be assessed.
The lymphocyte transformation test has been the main in vitro assay of T-cell immunity in leprosy. The response strengthens with lymphocytes from tuberculoid patients and diminishes with cells from those toward the lepromatous end of the spectrum.16 In general, occupational leprosy contacts have a frequency of response higher than that of unexposed control groups, and this increases with duration of exposure.17 Crude leprosy antigens contain many proteins including the immunodominant heat-shock proteins of 65- and 70-kDa.3-5 Therefore, a positive cellular immune response may be due to previous BCG vaccination or to exposure to environmental mycobacteria. Although it is likely that an individual with strong lymphocyte proliferation would develop tuberculoid rather than lepromatous leprosy, it is not possible at present to distinguish the T-cell response of a fully immune contact from that of a person with tuberculoid leprosy.
The study of contacts using individually purified antigens is increasing. The MLW1 cell-wall fraction from M. leprae, containing antigen 7, stimulated strong responses in both tuberculoid patients and healthy contacts, but not in lepromatous patients or nonexposed controls.18 Recombinant protein antigens are now being used in assays with T-cell clones but the results are complicated by the extent of reactivity at the T-cell level. For example, although M. leprae-specific clones reactive with the 18-kDa antigen have been isolated, it is now clear that the antigen shares an epitope with Mycobacterium w and elicits a response in BCG-vaccinatcd European donors.19 The 70-kDa protein shows extensive sequence homology between M. leprae, M. tuberculosis and M. bovis (BCG),3,4 and the 65-kDa protein from M. leprae 3,5 also has extensive sequence homology with similar proteins from other mycobacteria. The next step will be to evaluate synthetic peptides containing M. leprae-specific epitopes from these and other antigens as T-cell antigens in leprosy patients and their contacts.
Epidemiological evaluation of vaccines. A thorough understanding of the epidemiology of leprosy in trial areas is vital to the planning for and performance of vaccine levels. It is important that precise definitions of diagnostic criteria and survey methodology for case detection be standardized. Much of the confusion in the literature over the effects of vaccines, especially BCG, is because of methodological issues. The prevalence rates of leprosy vary considerably within a country and districts, and even between villages only short distances apart. The confounding effects of such clustering, which could be due to genetic or environmental factors, must be considered in the trial design. The prolonged incubation period of leprosy means that the vaccine's protective effects will, if given to all age groups, only be seen in successive age cohorts. The stabilizing or therapeutic effect on already infected individuals will be more immediate and may include the precipitation of self-healing lesions. The vaccine's effect may also be diluted if multiple infections rather than a single infection are necessary to produce disease. The role of subjects with subclinical infection in furthering the spread of infection is unclear, but may have implications for assessing vaccine efficacy.
In light of these considerations, Dr. Engers (WHO, Geneva) presented the characteristics of the two WHO-sponsored trials of heat-killed armadillo-derived M. leprae with BCG, compared to BCG alone. The Venezuelan trial is a double-blind trial in a population of close contacts of known leprosy patients; the Karonga trial in Malawi is a randomized, controlled trial in a general population. Preliminary results from these studies are expected in 1991 and 1995, respectively.
New animal models for testing new leprosy vaccines. The evaluation of efficacy of these and second-generation vaccines in humans requires 10 or more years with populations of 80,000-100,000 people, and are very expensive. It is worth evaluating the results of existing trials before new formulations are embarked upon. Although the final efficacy of a vaccine must be determined in man, candidate vaccines or antigens should first be evaluated in an animal model which reflects some of the characteristics of human leprosy. Assays for T-cell reactivity, such as lymphocyte proliferation or delayed-type hypersensitivity, are not necessarily related to protection. The mouse foot-pad protection model described by Shepard 40 and Rees 41 is currently the best characterized system for studying protection, although it has the drawback that the infection is minimal and self-limiting. However, the protective effect of vaccination with armadillo-derived M. leprae was first demonstrated in this system, and other candidate vaccines have recently been tested with it.42-44 The 65-kDa protein of M. leprae was the first recombinant molecule to be tested as a single protein and was not found to be protective.43 The cell-wall complex recently isolated has been shown to be protective against foot-pad infection by Gelber and co-workers,44 raising the possibility that protective molecules may eventually be dissected out from this mycobacterium complex.
The immunodeficient, athymic nude mouse provides another host for M. leprae growth and can be developed as a model for defining the relevance of antigens for immunotherapy and, possibly, vaccines.45 Low-dose infection of the foot pad with M. leprae increases exponentially until saturation of the developing macrophage granuloma is reached at approximately 6 months. Since the nude mouse is thymus-deficient, M. leprae infections proceed unchecked. Accordingly, adoptive transfer of T cells derived from syngeneic, normal mice should provide a model to study recognition, killing and clearance of M. leprae on a defined cellular and antigen-specific basis. The recent demonstration that human hematopoietic and lymphoid cells can develop in mice with a severe immunodeficiency disorder, SCID,46 could lead to development of an alternative model for evaluating protective antigens. Such approaches, combined with available transgenic models, may lead to the construction of better systems for testing potential leprosy vaccines.
Ultimately, however, vaccine candidates need to be assayed in immunologically intact animal models that develop multibacillary leprosy. Only two such species are currently documented -the nine-banded armadillo and the mangabey monkey. Armadillos are more susceptible to leprosy than humans, and up to 90% of armadillos inoculated with M. leprae develop leproma-tous leprosy. The manifestations of the disease in armadillos also suggest hypersus-ceptibility and, unlike humans where the disease is confined primarily to the skin and peripheral nerves, virtually all major tissues and organs of armadillos are invaded by M. leprae.47,48 The high count of infected tissues has made armadillos the primary source of leprosy bacilli for the preparation of experimental vaccines and related studies. However, there have been no sustained attempts to develop the armadillo as a model for the evaluation of vaccines or, for that matter, for testing the efficacy of new drugs proposed for use in leprosy.
Most armadillos are lepromin skin-test negative but the 9% which are lepromin positive show a reduced susceptibility to infection with M. leprae.49 One approach to the testing of vaccines in armadillos could be to attempt to induce skin-test reactivity in lepromin-negative animals and, subsequently, to test these preparations for their ability to protect against, or at least significantly delay, development of infection in inoculated armadillos.
Objections to the use of the armadillo as a model for evaluation of vaccines are that they are expensive to maintain, difficult to manage in captivity, and can be naturally infected with M. leprae in the wild prior to capture. The cost of maintaining armadillos is greater than the cost of most conventional laboratory animal species, but much less expensive than trials in humans. Also, from the standpoint of time, armadillos could provide information in 3 years or less on the efficacy of a preparation and enhance the likelihood of success in humans. The natural disease in armadillos has been extensively studied,50-52 and appropriate quarantine measures can minimize the risk of using armadillos already naturally infected with M. leprae.
Nonhuman primates constitute the other model for assessing the efficacy of vaccines because of their close phylogenetic relationship to humans. The first successful attempt to infect monkeys was in 1980, and was based on the discovery of naturally acquired leprosy in a mangabcy monkey.53,54 In related studies, rhesus and African green monkeys have shown a certain degree of susceptibility to leprosy but neither appear to be as suitable as the mangabey for vaccine studies. Approximately 70% of mangabeys inoculated with M. leprae develop disseminated lepromatous leprosy, the manifestations of which in mangabeys are similar to those in humans. Mangabeys can be either lepromin positive or negative, and it is conceivable that, like armadillos, vaccine preparations could first be assessed for their ability to induce lepromin skin test reactivity in mangabeys followed by attempts to assess the ability of effective preparations to delay or prevent the development of leprosy in M. leprae-inoculated mangabeys.
Application of immunology to screen vaccine candidates. In 1989, it is appropriate to ask what developments in immunology should be utilized in the screening of new-generation candidate vaccines. Clearly the emphasis today is directed toward T-cell function. Therefore, in vitro tests employed following immunization in animal models will focus on T-cell reactivity, and will be used to compare responses of T cells from peripheral blood of humans from contacts, tuberculoid, and lepromatous patients. The following might be envisaged in such screening: a) T-cell proliferation assays using known proteins and peptides. Since this assay appears to measure proliferation of Th cells, it is important to determine the range of Th responsiveness and whether there are different functional subpopulations, such as Th1 and Th2.15 b) The profile of cytokines released by Th cells following their response to vaccine epitopes. Heterogeneity of cytokine secretion patterns is beginning to have greater significance as the effects of IL-2, IL-4, IL-5, and IL-6 on B- and T-cell responses are beginning to emerge, c) The effect of adoptive transfer of T cells in animal models where mycobacterial disease can be studied. This may allow a direct analysis of specific T-cell function in the disease process, d) The construction of viral vectors containing vaccine epitopes will allow the development of cells where such epitopes may be associated with the expression of class I MHC molecules. Such cells are the targets needed to reveal peptides associated with class I MHC to measure, quantitatively, the activity of cytotoxic T cells. It is important to now use recombinant technology to delineate helper and cytotoxic T-cell function in protective immunity, e) Antibody response patterns should not be forgotten. As B-cell epitopes are defined on proteins from M. leprae, it remains important to screen them to determine whether they have a predictive value in the development of clinical disease.
Finally, it is worth stressing that the problems of new-generation vaccine development are not unique to leprosy. There is considerable use of similar knowledge and technology in the study of immunity to malaria, leishmania, and AIDS. It is important for research workers in leprosy to be aware and make use of knowledge and solutions to problems in other fields. It is this combined effort that will bring new, effective vaccines to infectious diseases.
- James D. Watson, Ph.D.
Department of Immunobiology
School of Medicine
The University of Auckland
Private Bag
Auckland, New Zealand
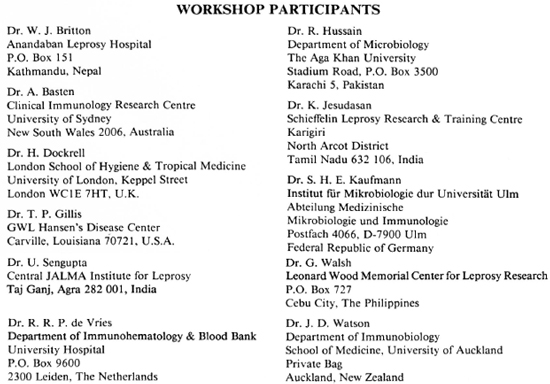
Acknowledgments. We thank the Leprosy Trust Board of New Zealand and the Public Health Service of Nepal for sponsoring the First Vaccilep Workshop. We thank all particpants of the First Vaccilep Workshop for their views and discussion which we have used in the development of this editorial. We appreciate their interaction and support.
1. Young, R. A., Mehra, V., Sweetser, D., Buchanan, T. M, Clark-Curtiss, J., Davis, R. W. and Bloom, B. R. Genes for the major protein antigens of the leprosy parasite Mycobacterium leprae. Nature 316(1985) 450-452.
2. Engers, H. D., Abe, M., Bloom, B. R., Mehra, V., Britton, W., Buchanan, T. M., Khalolkar, S. K., Young, D. B., Closs, O., Gillis, T., Harboe, M., Ivanyi, J., Kolk, A. H. J. and Shepard, C. C. Workshop: results of a World Health Organization-sponsored workshop on monoclonal antibodies to Mycobacterium leprae. Infect. Immun. 48 (1985) 603-605.
3. Watson, J. D. Leprosy: understanding protective immunity. Immunol. Today 10 (1989) 218-221.
4. Garsia, R. J., Hellqvist, L., Booth, R. J., Radford, A. J., Britton, W. J., Astbury, L., Trent, R. J. and Basten, A. Homology of the 70-kilodalton antigens from Mycobacterium leprae and Mycobacterium bovis with the Mycobacterium tuberculosis 71-kilodalton antigen and with the conserved heat shock protein 70 of cu-caryotes. Infect. Immun. 57 (1989) 204-212.
5. Shinnick, T. M., Sweetser, D., Thole, J. E. R., van Embdcn, J. D. A. and Young, R. A. The etiologic agents of leprosy and tuberculosis share an immunoreactivc protein antigen with the vaccine strain Mycobacterium bovis BCG. Infect. Immun. 55 (1987) 1932-1935.
6. Abou-Zeid, C, Filley, E., Steele, J. and Rook, G. A. W. A simple new method for using antigens separated by polyacrylamidc gel electrophoresis to stimulate lymphocytes in vitro by converting lines cut from Western blots into antigen bearing particles. J. Immunol. Methods 98 (1987) 5-10.
7. Converse, P. J., Ottenhoff, T. H. M., Gebre, N., Ehrenberg, J. P. and Kiessling. R. Cellular, humoral, and gamma interferon responses to Mycobacterium leprae and BCG antigens in healthy individuals exposed to leprosy. Scan. J. Immunol. 27 (1988) 515525.
8. Mendez-Samperio, P., Lamb, J., Bothamley, G., Stanley, P., Ellis, C. and Ivanyi, J. Molecular study of the T cell repertoire in family contacts and patients with leprosy. J. Immunol. 142 (1989) 3599-3604.
9. Hunter, S. W., McNeil, M., Modlin, R. L., Mehra, V., Bloom, B. R. and Brcnnan, P. J. Isolation and characterization of the highly immunogenic cell wall-associated protein ofM. leprae.}. Immunol. 142 (1989) 2864-2872.
10. Mehra, V., Bloom, B. R., Torigian, V. K., Mandich, D., Reichal, M., Young. S. M. M., Salgamc, P., Convit, J., Hunter, S. W., McNeil, M., Brennan, P. J., Rea, T. H. and Modlin, R. L. Characterization of Mycobacterium leprae cell wall-associated proteins with the use ofT lymphocyte clones. J. Immunol. 142 (1989) 2873-2878.
11. Mustafa, A. S., Oftung, F., Deggerdal, A., Gill, H. K., Young, R. A. and Godai, T. Gene isolation with human T lymphocyte probes. J. Immunol. 141 (1988) 2729-2733.
12. Marrack, P. and Kappler, J. The T cell receptor. Science 238 (1987) 1073-1079.
13. Janis, E. M., Kaufmann, S. H. E., Schwartz, R. H. and Pardoll, D. M. Activation of γδ T cells in the primary' immune response to Mycobacterium tuberculosis. Science 244 (1989) 713-716.
14. Raulet, D. H. Antigens for γ/δ T cells. Nature 339 (1989) 342-343.
15. Mossmann. T. R. and Coffman, R. L. Heterogeneity of cytokine secretion patterns and functions of helper T cells. Adv. Immunol. 46 (1989) 111.
16. Kaufmann, S. H. E. Immunity against intracellular bacteria: biological effector functions and antigen specific ity of T lymphocytes. Curr. Topics Micro. Immunol. 138 (1988) 141.
17. van Voorhis, W. C, Kaplan, G., Sarno, E. N., Horowitz, M. A., Steinman, R., Levis, W. R., No-gueira, N., Hair, L. S., Gattass, C. R., Arrick, B. A. and Cohn, Z. A. The cutaneous infiltrates of leprosy; cellular characteristics and the predominant T-cell phe-notvpe. N. Engl. J. Med. 307 (1982) 1593-1597.
18. Ottenhoff, T. H. M., Kale, B., van Embden, J. D. A., Thole, J. E. R. and Kiessling, R. The recombinant 65-kD heat shock protein of Mycobacterium bovis bacillus Calmette Guérin/.U. tuberculosis is a target molecule for CD4+ cytotoxic T lvmphocytes that lyse human monocytes. J. Exp. Med. 168 (1988) 1947-1952.
19. Hancock, G. E., Cohn, Z. A. and Kaplan, G. The generation of antigen-specific , major histocompatibility complex-restricted cytotoxic T lymphocytes of the CD4+ phenotype; enhancement by the cutaneous administration of interleukin 2. J. Exp. Med. 169 (1989) 909-919.
20. Kaplan, G., Sarno, E. N., Job, C. K., McElrath, J., Proto, J. A., Nathan, C. F. and Cohn, Z. A. Cellular responses to the intradermal injection of recombinant human gamma-interfcron in lepromatous leprosy patients. Am. J. Pathol. 128 (1987) 345-353.
21. Kaplan. G., Kiessling, R., Teklemariam, S., Hancock, G., Sheftel, G., Job, C. K., Converse, P., Ottcn-hoff, T. H. M., Becx-Bleumink, M., Dietz, M. and Cohn, Z. A. The reconstitution of cell-mediated immunity in the cutaneous lesions of lepromatous leprosy by recombinant interleukin 2. J. Exp. Med. 169(1989)893-907.
22. Bjorkman, P. J., Saper, M. A., Samraoui, B., Bennett, W. S., Strominger, J. L. and Wiley, D. C. The foreign antigen binding site and T cell recognition regions of class I histocompatibility antigens. Nature 329 (1987) 512-518.
23. de Vries, R. R. P., Ottenhoff, T. H. M. and van Schooten, W. C. A. Human leukocyte antigens (HLA) and mycobacterial disease. Springer Semin. Immu-nopathol. 10 (1988) 305-318.
24. Bloom, B. R. and Mehra, V. Immunological unresponsiveness in leprosy. Immunol. Rev. 80 (1984) 5-28.
25. Modlin, R. L., Kato, H., Mehra, V., Nelson, E. E., Fan, X.-D., Rea, T. H., Pattengale, P. K. and Bloom, B. R. Genetically restricted suppressor T-cell clones derived from lepromatous leprosy lesions. Nature 322 (1986) 459-161.
26. Ottenhoff, T. H. M., Elfcrink, D. G., Klatser, P. R. and de Vries, R. R. P. Cloned suppressor T cells from a lepromatous leprosy patient suppress Mycobacterium leprae reactive helper T cells. Nature 322 (1986) 462-464.
27. Kaplan, G., Gandhi, R. R., Weinstein, D. E., Levis, W. R., Patarroyo, M. E., Brennan, P. J. and Cohn, Z. A. Mycobacterium leprae antigen-induced suppression of T cell proliferation in vitro. J. Immunol. 138 (1987) 3028-3034.
28. Jacobs, W. R., Jr., Tuckman, M. and Bloom, B. R. Introduction of foreign DNA into mycobacteria using a shuttle phasmid. Nature 327 (1987) 532-535.
29. Sinha, S., Sengupta, U., Ramu, G. and Ivanyi, J. Serological survey of leprosy and control subjects by a monoclonal antibody-based immunoassay. Int. J. Lepr. 53 (1985) 33-38.
30. Hunter. S. W. and Brennan. P. J. A novel phenolic glycolipid from Mycobacterium leprae possibly involved in immunogenicity and pathogenicity. J. Bac-tcriol. 147 (1981) 728-735.
31. Fujiwara, T., Hunter, S. W., Cho, S.-N., Aspinall, G. O. and Brennan, P. J. Chemical synthesis and serology of disaccharides and trisaccharides of the phenolic glycolipid antigens from the leprosy bacillus and preparation of a disaccharidc protein conjugate for se-rodiagnosis of leprosv. Infect. Immun. 43 (1984) 245252.
32. Klatser, P. R., de Wit, M. Y. L. and Kolk, A. H. J. An ELISA-inhibition test using monoclonal anti-bodv for the serology of leprosy. Clin. Exp. Immunol. 62 ('1985) 468-473.
33. Burgess, P. J., Fine, P. E. M., Ponnighaus, J. M and Draper, C. Serological tests in leprosy. The sensitivity, specific ity and predictive value of ELISA tests based on phenolic glycolipid antigens, and the implications for their use in epidemiological studies. Epidemiol. Infect. 101 (1988) 159-171.
34. Menzel, S., Harboe, M., Bcrgsvik, H. and Brennan, P. J. Antibodies to a synthetic analog of phenolic glycolipid-1 of Mycobacterium leprae in healthy house-hold contacts of patients with leprosy. Int. J. Lepr. 55 (1987) 617-625.
35. Chanteau, S., Cartel, J.-L., Roux, J., Plichart, R. and Uach, M.-A. Comparison of synthetic antigens for detecting antibodies to phenolic glycolipid I in patients with leprosy and their household contacts. J. Infect. Dis. 157 (1988) 770-776.
36. Godal, T. Immunological aspects of leprosy-present status. Prog. Allergy 25 (1978) 211-242.
37. Godal, T., Lofgren, M. and Negassi, K. Immune response to M. leprae of healthy leprosy contacts. Int. J. Lepr. 40 (1972) 243-250.
38. Closs, O., Reitan, L. J., Negassi, K., Harboe, M. and Helchu, A. In vitro stimulation of lymphocytes in leprosy patients, healthy contacts of leprosy patients, and subjects not exposed to leprosy. Scand. J. Immunol. 16 (1982) 103-115.
39. Mustafa, A. S. Identification of T-cell-activating recombinant antigens shared among three candidate anti-leprosy vaccines, killed M. leprae, M. bovis BCG and Mycobacterium w. Int. J. Lepr. 56 (1988) 265-273.
40. Shepard, C. C. The experimental disease that follows the injection of human leprosy bacilli into footpads of mice. J. Exp. Med. 112 (1960) 445-454.
41. Rees, R. J. W. Limited multiplication of acid-fast bacilli in the foot-pads of mice inoculated with Mycobacterium leprae. Br. J. Exp. Pathol. 45 (1964) 207218.
42. Singh, N. B., Lowe. A. C. R. E., Rees, R. J. W. and Colston, M. J. Vaccination of mice against Mycobacterium leprae infection. Infect. Immun. 57 (1989) 653-655.
43. Lamb. F. I., Kingston, A. E., Estrada-G., I. and Colston, M. J. Heterologous expression of the 65 kilodalton antigen of Mycobacterium leprae and murine T-cell responses to the gene product. Infect. Immun. 56 (1988) 1237-1241.
44. Gelber. R. H., Hunter. S. W., Mohagheghpour, N., Murray, L., Siu, P., Tsang, M., Brennan, P. J. Protection of mice by vaccines from cell walls of Mycobacterium leprae. In: Proceedings of the 28th Iuterscience Conference on Antimicrobial Agents and Chemotherapy (ICAAC). October 1988. Los Angeles. Washington, D.C.: ASM Publications, abstract no. 1038.
45. Colston, M. J. and Hilson, G. R. F. Growth of Mycobacterium lepraeandM. marinum in congenitally athymic (nude) mice. Nature 262 (1976) 399-401.
46. McCune, J. M. Namikawa, R., Kaneshima, H., Shultz, L. D., Lieberman, M. and Weissman, I. L. The SCID-hu mouse: murine model for the analysis of human hematolymphoid differentiation and function. Science 241 (1988) 1632-1639.
47. Binford, C. H., Storrs, E. E. and Walsh, G. P. Disseminated infection in the nine-banded armadillo (Dasypus novemcinctus) resulting from inoculation with M. leprae; observations made on 15 animals studied at autopsy. Int. J. Lepr. 44 (1976) 80-83.
48. Walsh. G. P. Experimental leprosy in the nine-banded armadillo (Dasypus novemcinctus). In: The Armadillo as an Experimental Model in Biomedical Research. Washington. D.C.: Pan American Health Organization. 1978. pp. 57-61. PAHO Sci. Pub. No. 366.
49. Job. C. K., Sanchez, R. M., Hunt. R. and Hastings, R. C. Prevalence and significance of positive Mitsuda reaction in the nine-banded armadillo (Dasypus novemcinctus). Int. J. Lepr. 55 (1987) 685-688.
50. Walsh. G. P., Meyers, W. M. and Binford. C. H. Naturally acquired leprosy in the nine-banded armadillo: a decade of experience-1975-1985. J. Leukocyte Biol. 40 (1986) 645-656.
51. Job, C. K., Harris, E. B, Allen, J. and Hastings, R. C. A random survey of leprosy in wild nine-banded armadillos in Louisiana. Int. J. Lepr. 54 (1986) 453457.
52. Truman, R. W., Shannon, E. J., Hagstad, H. V., Hugh-Jones. M. E., Wolff. A. and Hastings, R. C. Evaluation of the origin of Mycobacterium leprae infections in the wild armadillo, Dasypus novemcinctus. Am. J. Trop. Med. Hyg. 35 (1986) 588-593.
53. Meyers, W. M., Walsh, G. P., Brown, H. L., Binford, C. H., Imcs. G. D., Jr., Hadfield, T. L., Schlagel, C. J., Fukunishi. Y., Geronc. P. J., Wolf, R. H., Gormus, B. J., Martin. L. N., Harboe, M. and Imaeda, T. Leprosy in a mangabcy monkey -naturally acquired infection. Int. J. Lepr. 53 (1985) 1-14.
54. Meyers, W. M., Walsh, G. P., Brown, H. L., Fukunishi, Y., Binford. C. H., Gerone, P. J. and Wolf, R. H. Naturally acquired leprosy in a mangabcy monkey (Cercocebus sp.).Abstract in Int. J. Lepr. 48 (1980) 495.
In order not to delay publication of this issue, the Board of Directors of the JOURNAL has given its permission for the Index to Volume 57 to be published in the March 1990 issue of the JOURNAL. We hope this will not duly inconvenience readers who wish to bind their volumes promptly. -RCH