- Volume 57 , Number 4
- Page: 844–6
Application of a health education model to obtain early and regular treatment of leprosy patients*
Editor's Note: In an effort to increase the utility of the Journal in continuing medical education, it has been suggested that a new feature of the Journal he added on a trial basis to the Editorial Section-Clinical Notes. In this section, we welcome contributions dealing with practical problems in leprosy work. Submissions to this section will undergo minimal editorial changes and may well contain controversial points. Letters to the Editor pointing out other viewpoints are welcome.- RCH
The Leprosy SET Unit at Christian Fellowship Community Health Centre, Am-bilikkai. South India, covers a population of 122,000. There are six leprosy inspectors and one nonmedical supervisor. The medical aspects are supervised by Dr. Jacob Cherian, Director and Founder, and the field work, health education and statistics by Dr. C. M. E. Matthews, Field Director. There are also 24 mini health centers (MHCs) for community health work and primary health care, covering a population of 124,000. This area is not quite the same as that for the SET unit. For six MHCs government workers are doing the leprosy work. In another area there is leprosy work but no MHCs. The MHCs are run mainly by community health workers who have been trained for 2 years in preventive health work as well as curative work. Most cases can be treated by them. They can also refer cases to the doctors who visit each center three times a week. The community health workers are assisted by village-level workers, who are nearly always from that community and usually do not have any formal training but are given practical training by the community health workers. The leprosy inspectors are responsible for the leprosy work, but are assisted by the community health workers who help to motivate and bring patients for treatment.
The prevalence of leprosy in the SET area is 9/1000 and the incidence is 1.7/1000. The lepromatous rate is 25%; the deformity rate, 25%. In new cases these rales are only 4% and 1.6%, respectively. Monthly statistics are collected and consolidated using a computer.
Health education. In 1982 only 43% of all known cases were taking treatment, all taking dapsone (DDS) only. Because of the low attendance for treatment, we started an intensive health education program to improve the level of treatment. This program was based on behavioral science theory, and was similar to a plan tried on a smaller scale at Christian Medical College, Vellore, India.1 The behavorial science theory is based on a combination of Cartwright's theory2 and Lionberger's diffusion theory.3 Table 1 shows the steps involved.
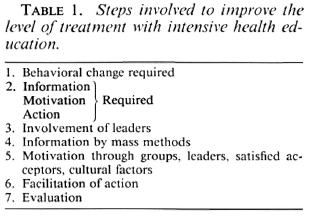
First, the precise behavior change required must be known. The objective of the health education program is to bring about this behavior change. The two most important behavior changes required for leprosy at that time were: a) known cases must take early and regular treatment, and b) suspected cases must come forward early for diagnosis.
Next, the informational, motivational and action structures required in the minds of the target group for them to take the required action must be known. Information alone is not enough, and all three stages must be carefully considered. Also, the information given must be appropriate and what is necessary to take action. If too much information is given too quickly people will not remember even the essential things.
Table 2 is a brief summary of the minimum requirements. With regard to cause, there are many wrong beliefs about leprosy. Some think it is due to sins, or that it is hereditary or linked with venereal diseases. The patients must know that the treatment will take a long time. Otherwise, when no immediate effect is seen, they will feel discouraged and may give up taking treatment. The patients must also know that leprosy can be cured, so that the effort of taking tablets for so long seems worthwhile. It is also important for the early symptoms to be known. Often people think that leprosy means only the advanced disease or disease with deformities.
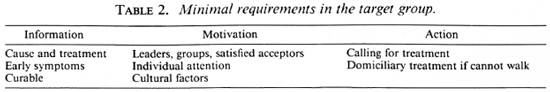
For motivation, it is not enough only to communicate directly with the patient. Others, such as community leaders, may have more influence. Those from the community who have taken treatment for a long time and are cured may also have more source credibility for other patients than the health staff. Group methods are also important for motivation since many studies have shown the important influence of groups on human behavior. If the group as a whole decides to take some action, it is much easier for them to carry it out than if one individual decides by himself. Consideration of cultural factors is also very important for motivation. These will include people's beliefs about the cause of leprosy and also the stigma attached to it.
At the action stage people may need cues, such as reminders that treatment is due. Those who have real difficulty in coming to the clinic, for example, those who cannot walk, should be given treatment at home.
Application of theory and results. The application of the theory for steps 3 to 7 in Table 2 was carried out as follows. First, the influential leaders were contacted and their participation and help was sought. Group meetings of leaders were held, the problem was discussed, and information about leprosy was given to them. The next stage was to use mass methods such as drama, puppet shows, films and slides to spread the information to a large number of people. Leaders also spoke and introduced the shows. This was followed up with small group meetings for motivation, again involving the leaders as far as possible. Lastly, at the action stage all absentees were called for treatment.
This whole process took about 6 months in each area, after which follow up was continued. The results can be seen in The Figure which shows considerable improvement in percent attendance from 43% in January 1982 to 95% in March 1987. This is the percentage of all remaining known cases, not just the percentage of registered cases. Percent treatment at the end of December 1987 was lower because a new pattern of MDT was being introduced.
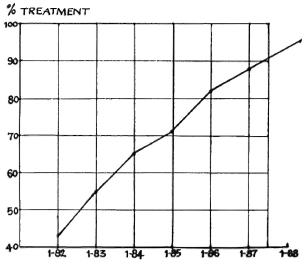
The Figure. Percent attendance January 1982- January 1988.
Case detection has also increased over the past 3 years. The number of new cases found per 1000 population was 1.0, 1.3. 1.8, 1.7. for 1984. 1985, 1986, 1987, respectively. This will not represent a real increase in incidence, but improved early detection of cases by the workers. In 1987, 29% of the new cases were detected by voluntary reporting as compared with 18% in 1983. So, it can be seen that a considerable effect has been obtained for both of the behavioral changes required.
Conclusions. The results indicate that the health education model used here can show considerable improvement in the percent of known cases taking treatment and in early case detection. All three factors in the model-information, motivation, and action-must be considered, not just information alone.
- C. M. E. Matthews, PhD., M.P.H.
Field Director
Christian Fellowship Community Health Centre
Ambilikkai
Anna District
Tamil Nadu, South India
Acknowledgments. We are most grateful to American Leprosy Missions, Inc., for much valuable help. I also thank Mr. Santiagu, Non-Medical Supervisor, and Mr. Vecrabadran, Mr. Manoharan, Mr. Joshua Deniel, Mr. Mahimainathan. and Mr. Gopalakrishnan, Leprosy Inspectors.
1. Matthews, C. M. E., Selvapandian, A. J. and Jesudasan, M. Health education and leprosy. Lepr. Rev. 51 (1980) 167-171.
2. Lionberger, H. F. Adoption of New Ideas and Practices. Ames, Iowa, U.S.A.: Iowa State University Press, 1960.
3. Cartwright, D. Some principles of mass persuasion. Hum. Relations 2 (1949) 253-255.
* The author died tragically in an accident while this manucript was under review. Her obituary appears on page 883 of this issue.-RCH