- Volume 58 , Number 3
- Page: 462–5
An unusual case of hansen's disease (lepromatous leprosy) with circulating anticoagulant and macroglobulinemia
ABSTRACT
A 42-year-old Mexican migrant laborer with a previous history of neurofibromatosis presented with a stuffy nose and chronic ulceration of his soft palate. Multiple subcutaneous nodules were found on his skin, and laboratory investigation revealed an elevated activated partial thromboplastin time (APTT). Further laboratory evaluation showed a lupus-like circulating anticoagulant deemed IgM by quantitative immunoglobulin studies. Although coagulation defects in lepromatous leprosy arc rare, the preoperative preparation of a patient with leprosy may require a screening prothrombin time (PT), APTT and platelet count. Abnormalities in these values may indicate the need for specific factor assays and a search for circulating anticoagulant.RÉSUMÉ
Un travailleur emigré mexicain de 42 ans avec une histoire antérieure de neurofibromatose s'est présenté avec un nez encombré et une ulcération chronique du palais. Des nodules sous-cutanés multiples furent trouvés sur sa peau, et les examens de laboratoire ont montré un temps de thromboplastine partielle activée (TTVA) élevé. La poursuite de l'investigation de laboratoire montra des facteurs anticoagulants comme dans le lupus, que des études quantitatives ont révélé être des IgM. Bien que des troubles de la coagulation soient rares dans la lèpre lépromateuse, la préparation pré-opératoire d'un patient atteint de lèpre peut nécessiter la vérification du temps de prothrombine (TP), et le comptage des plaquettes. Des anomalies dans ces valeurs peuvent indiquer le besoin de dosages de facteurs spécifiques et la recherche d'anticoagulants circulants.RESUMEN
Se presenta el caso de un obrero de origen mexicano, de 42 años de edad, con una historia previa de neurofibromatosis, que presentó una nariz congestionada y ulceración crónica del paladar blando. En su piel se encontraron múltiples nodulos subcutáneos y los exámenes de laboratorio revelaron un elevado tiempo parcial de tromboplastina activada (TPTA) y la presencia de un anticoagulante circulante parecido al encontrado en lupus y de clase IgM, según los estudios cuantitativos de inmunoglobulinas. Aunque los defectos de coagulación son raros en la lepra lepromatosa, la preparación prcoperativa de un paciente con lepra puede requerir de la medición del tiempo de protrombina (TP), del TPTA y del número de plaquetas. Las anormalidades de estos valores pueden indicar la necesidad de ensayos para factores específicos y la búsqueda de anticoagulante circulante.A.B. is a 42-year-old Mexican laborer who emigrated to the U.S.A. from Mexico 8 years prior to his presentation. He was in good health until one year ago when he began to have frequent coughs, colds, and minor nose bleeds. He was treated symptomatically. His past medical history included a diagnosis of neurofibromatosis made by the microscopic examination of biopsies of the numerous subcutaneous nodules he exhibited throughout his body.
On physical examination he had a stuffy nose and an indurated ulceration of the hard palate (2.0 x 3.0 cm) (Fig. 1). Multiple subcutaneous nodules were evident throughout his body surface.
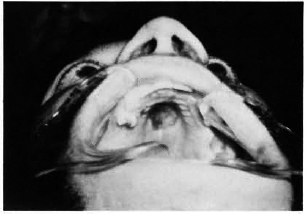
Fig. 1. Chronic ulcer, soft palate.
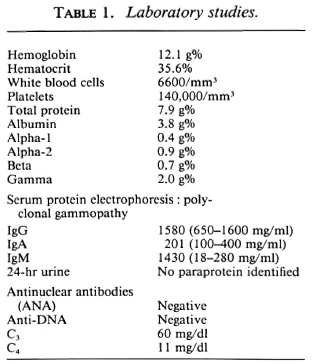
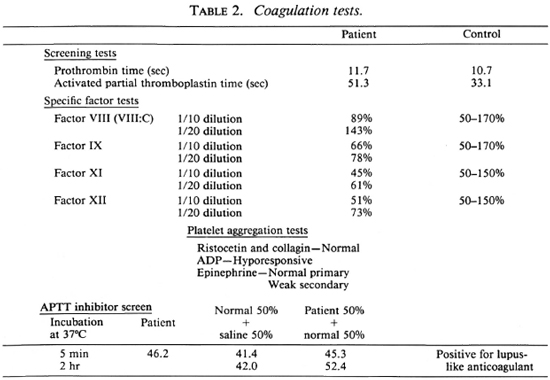
Laboratory evaluation disclosed a prolonged activated partial thromboplastin time (APTT) of 51.3 sec (control = 33.1 sec). His prothrombin time and factor assays were normal at 1/20 dilution (Table 2). Further examination showed that the patient had an immediate inhibitor of APTT with low intrinsic factor avidity which was readily diluted. The discrepancy in APTT did not correct on mixing with normal plasma. Because of the presence of abnormal circulating anticoagulant, laboratory testing for lupus erythematosus was performed. His ANA, anti-DNA, and complement studies were within normal limits. The patient had a negative VDRL test. A detailed drug history was negative. The patient had an elevation of the gamma globulin fraction in a polyclonal distribution on serum protein electrophoresis (Table 1). Quantitative immunoglobulin determination revealed an IgM of 1430 mg/dl. IgG and IgA were within normal limits. While the patient admitted drinking 8 to 10 beers a week for several years, his liver function tests were normal.
The patient underwent biopsy of the subcutaneous nodules, nasal cartilage, and soft palate lesions without any bleeding complications. Pathological examination of the cartilage and palatal tissues initially showed chronic inflammation with a preponderance of plasma cells, lymphocytes, and histiocytes. The cells contained PAS-positive intranuclear globules ("Dutcher bodies") which are associated with IgM gammopa-thy. Ziehl-Neelsen staining of the biopsy material from the subcutaneous nodules, however, gave a diagnosis of lepromatous leprosy (Figs. 2 and 3).
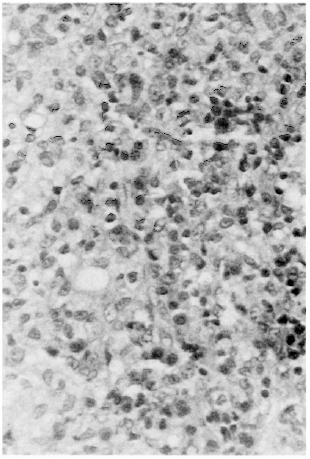
Fig. 2. Biopsy of subcutaneous nodule showing lymphocytes, plasma cells and histiocytes.
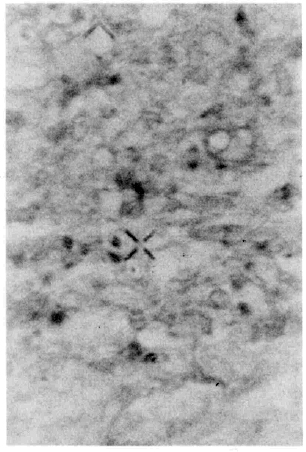
Fig. 3. Spécial Zichl-Neelsen staining showing clusters of leprosy bacilli.
DISCUSSION
Leprosy (Hansen's disease) is an ancient disease which is rarely encountered in the day-to-day practice of medicine in the U.S.A. However, it is becoming frequently recognized in those areas where migrant populations from Mexico and South-East Asia arc prevalent. The presentation of sinusitis, oral ulcer, and subcutaneous nodules in an immigrant patient should raise the suspicion of Hansen's disease. Interestingly, unfamiliarity with this disease and unawarcness of its low infectivity rates created some anxiety in our medical personnel. The patient was eventually transferred to the special unit for leprosy at the University of Southern California Medical Center where treatment with rifampin and dapsone was begun.
An association of "lupus anticoagulant" with lepromatous leprosy has been previously reported by Cole, et al. (2) in an asymptomatic patient without antecedent erythema nodosum leprosum. In Cole's case, the anticoagulant was felt to be an IgM immunoglobulin. Basu, et al. (1) also reported significant numbers of leprosy patients with an alteration in coagulation tests, but did not screen them for circulating anticoagulant. It is suggested that screening coagulation tests should be performed in leprosy patients prior to surgical procedures. If screening tests are abnormal, specific factor assays and a search for lupus anticoagulant may be helpful.
Acknowledgments. The author wishes to acknowledge the pathological diagnosis and special staining by K. Yamazaki, M.D., of Fountain Valley Community Hospital, and the coagulation review of this paper by Herman Branson, M.D., Assistant Professor, Department of Pathology, University of California, Irvine. Special thanks to Anil deSilva, M.D., Albert Einstein School of Medicine, for review of this manuscript. The technological assistance of A. Fagin, M.D., and the photographic help of Michael K. Samoszuk, M.D., are greatly appreciated. S. Arya, M.D., referred this interesting patient.
REFERENCES
1. Basu, A. K.., Chatterjee, J. B., Mukherjee, A. and Ghosh, S. Observations on hemostasis in leprosy. Bull. Calcutta Sch. Trop. Med. 18(1970)33-34.
2. Cole, F. S., Brusch, J. L. and Talarico, L. Circulating anticoagulant in lepromatous leprosy. Int. J. Lepr. 47(1979)121-125.
1. M.D., Ph.D., 801 N. Tustin Avenue, Suite 404, Santa Ana, California 92705, U.S.A.
Received for publication on 13 January 1989.
Accepted for publication in revised form on 7 March 1990.