- Volume 58 , Number 3
- Page: 571–2
A case of borderline tuberculoid leprosy presenting with papulonodular lesions
This department is for the publication of informal communications that are of interest because they are informative and stimulating, and for the discussion of controversial matters. The mandate of this JOURNAL is to disseminate information relating to leprosy in particular and also other mycobacterial diseases. Dissident comment or interpretation on published research is of course valid, but personality attacks on individuals would seem unnecessary. Political comments, valid or not, also are unwelcome. They might result in interference with the distribution of the JOURNAL and thus interfere with its prime purpose.
To the Editor:
A classical borderline tuberculoid leprosy patient 1 usually presents with macules or plaques resembling tuberculoid leprosy but the lesions arc more in number with a lesser degree of dryness, hair loss, and sensory loss. Recently, we encountered an interesting case of borderline tuberculoid leprosy with characteristic skin histopathology, presenting with innumerable plaques, papules, and nodules.
The patient, a 50-year-old man, was referred to our hospital with eruptions all over the body of 2 months' duration. There was no history of contact or of having taken an-tileprosy treatment. On examination, the patient had innumerable plaques, papules, and nodules all over the body, more on the extremities, varying in size from 0.3 cm to 1.5 cm in diameter (Figs. 1, 2, and 3). Nodules were also present on both ears. The plaques were well defined and erythematous. A few hypopigmented macules were seen on the lower limbs (Fig. 2). There was no sensory loss on either the skin lesions or in the glove-and-stocking area. There was no nerve thickening.

Fig. 1. Plaques and nodules on both upper limbs.

Fig. 2. Plaques, nodules, and macules on both lower limbs.

Fig. 3. Plaques on the buttocks.
Slit-skin smears for acid-fast bacilli were done twice and were found negative. A lepromin test was positive with a late reading of 9 mm. Biopsies taken from a plaque and a nodule at two different sites revealed a normal epidermis with extensive epithelioid and giant-cell granulomas with mod-crate lymphocytic infiltration in the dermis. There was partial destruction of appendages and nerves. Acid-fast staining (hematoxylin and cosin) was positive with a bacterial index of 1+ to 2+ (Fig. 4). A diagnosis of borderline tuberculoid Hansen's disease was made.
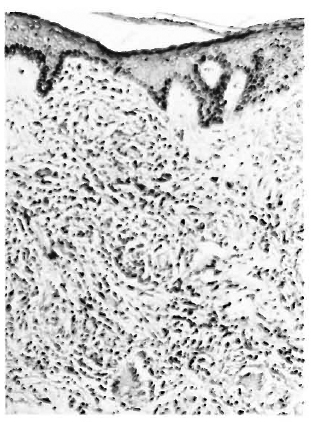
Fig. 4. Skin biopsy showing classical features of BT leprosy (H&E x 40).
In conclusion, this patient presented with a generalized skin disease clinically consistent with lepromatous leprosy. However, skin smears were negative and skin biopsy showed the characteristic picture of borderline tuberculoid leprosy. The positive lepromin test also indicates an intact cell-mediated immune response to Mycobacterium leprae. Although there is no histological evidence to prove that this disease started as lepromatous leprosy, taking into consideration the generalized papulonodular disease we presume that the patient would have upgraded to borderline tuberculoid leprosy from the lepromatous end of the spectrum.
- A. Ramachandran, M.D.
Assistant Director (Clinical)
- Rita Laxman, M.D.
Assistant Director (Pathology)
Central Leprosy Teaching and Research Institute
Chengalpattu 603001
Tamil Nadu, India
REFERENCES
1. Ridley, D. S. and Jopling, W. H. Classification of leprosy according to immunity; a five-group system. Int. J. Lepr. 34 (1966) 255-273.