- Volume 58 , Number 1
- Page: 78–97
The need for new drugs in the treatment and control of leprosy*
Editorial opinions expressed are those of the writers.
Purely in numerical terms, leprosy represents an enormous challenge to global health. Although no longer endemic in northwestern Europe, many millions of sufferers persist, predominantly in the underdeveloped world. Estimates vary as to exactly how many sufferers there are, but the World Health Organization (WHO) put the figure at 10.6 million in 1975.1 Since then estimates have varied between 10 and 12 million, but the prevalence is unlikely to have changed much, according to a recent report.2 That same report, published in October 1987, listed 5,340,895 registered sufferers, which is obviously a vast underestimate. Of these cases, approximately 62% are from Asia, 34% from Africa, 3% from South America, and the rest of the world accounts for only 1%. It can be seen that, purely in terms of numbers, the problem is enormous and, indeed, it is not surprising that the WHO has put leprosy in its top six tropical diseases demanding intensive research and training. More important, however, is the vast population at risk. Figures published in October 1987 2 estimate that 1.6 billion people live in areas where leprosy is a serious problem, i.e., where the estimated prevalence is over 1 case per 1000 persons. These people represent a vast reservoir of potential sufferers. Any threat to the control of leprosy, therefore, represents a threat to the health of these people.
Strategies for treatment and control of leprosy
The WHO recently detailed three main objectives of leprosy control.3 These were: a) to interrupt transmission of the infection in order to reduce incidence; b) to treat patients in order to achieve their cure and, where possible, complete rehabilitation; and c) to prevent the development of associated deformities. Various different methods of intervention have been tried in an attempt to achieve these goals. Drugs are the only agent that can effectively alter all three parameters. Immunization and chemoprophylaxis may profoundly affect transmission and an efficient screening method may also be useful. Various other interventions, such as segregation, education and a change in socioeconomic factors, may well help but these are less easily manipulated and therefore not the mainstay of programs.
Chemotherapy. The only really effective tool available for both individual treatment and control of leprosy in the community is chemotherapy. For this reason, the control of leprosy is largely undertaken by case detection and drug treatment. Implicit in the effective use of chemotherapy are several important cofactors. These include:
Case detection-this involves widespread and thorough coverage of endemic areas to find out new cases.
Ease of treatment-it should be borne in mind that the ideal treatment would involve: a) tablet formulation. It would certainly be an idea to put recommended drugs in a combined preparation; b) the tablet should have a low cost; c) it should be orally administered; d) the treatment should have long periodicity (not daily). e) If regular doses are necessary, they should be by selfadministration at home. f) The minimization of side effects. All of these factors will ensure better compliance and the minimal development of drug resistance. The recent popularity of calendar-marked blister packs illustrates some of these points.
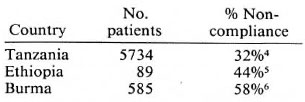
Case management-this will involve the minimization of dropouts. Compliance has been a major problem with leprosy chemotherapy to date, as shown in the table below. It may involve lack of attendance at clinics, incorrect drug taking, or even selling drugson the black market.
The first method used to tackle the problem of leprosy, in historical terms, was segregation. However, with the advent of sulfone drugs in 1941, chemotherapy became the mainstay of leprosy treatment and control. This situation is unlikely to change for some years. As the WHO technical report 3 into the chemotherapy of leprosy stated in its introduction, despite "... welcoming the steady progress made by... IMMLEP in its long term objective of developing a leprosy vaccine of proven effectiveness, the study group considered that the classical strategy of leprosy control, based on early detection and effective chemotherapy, is likely to remain unchanged for many years."
Sulfone resistance
Sulfones were introduced to treat leprosy in 1941. Sulfone resistance was suspected throughout the 1950s, but it was possible that what had initially appeared as resistance was, in fact, relapse due to inappropriate scrum levels or lack of compliance. However, a paper published in 1964 7 showed that 3 out of 7 strains from clinically resistant patients were insensitive to dapsone in the mouse foot pad system. The reason that resistance had taken so long to emerge was thought to be due to the long generation time of Mycobacterium leprae (11 days). The mutants took literally years to develop. By 1966 it was estimated that the prevalence of dapsone resistance in Sungei Buloh Leprosarium in Malaysia was 1 per 1000.8 This was probably an underestimate due to the use of high concentrations of dapsone in the mouse diet when testing. At this rate there did not seem to be an important problem.
In 1973 the prevalence of secondary dapsone resistance among the same group hadrisen to 35 per 1000.9 It was also shown that in a second group of patients who had received Solapsone as their initial treatment (an equivalent of about 10 nig dapsone daily), the prevalence ofdapsone resistance was 75 per 1000. This confirmed early suspicions that development of resistance was linked to low-dose therapy. By 1975 this figure had risen to 100 per 1000 10 and 166 cases in that center had been confirmed by the mouse foot pad system.
Information from other countries suggested rates of 190 per 1000 in Ethiopia;11 100 per 1000 in Costa Rica;12 and 37 per 1000 in Israel.13
When the WHO Expert Committee met in 1977 their answer was to call for the abandonment of monotherapy and the introduction of multidrug therapy (MDT) in the form ofdapsone with at least a brief course of either rifampin or clofazimine for the treatment of all multibacillary cases.1 4 Unfortunately, these recommendations were followed in only a small number of areas and change was very slow to occur.
In 1976 dapsone resistance was demonstrated in India15 in an area that had received well delivered dapsone monotherapy since 1963. The WHO Scientific Working Group on the Chemotherapy of Leprosy (THELEP) then began a survey in that same area which found the prevalence of resistance to be much higher than an interim estimate of 23 per 1000.16 Another THELEP trial in southern India found a prevalence of 20 per 1000.3
Other surveys of secondary dapsone resistance among smaller populations yielded the following results: Jiangsu Province, China, 51 per 1000;17 Shanghai, China, 34/40 per 100;3 Burundi, about 50 per 1000;3 and Mali, about 50 per 1000.18 Resistance was also reported in a number of other countries as widely separated as Australia, the United States of America, Guadeloupe, and The Netherlands. In short, wherever resistance has been sought among treated and relapsed patients it has been found. When multibacillary patients relapse with secondary dapsone resistance, they can infect their contacts with dapsone-resistant M. leprae. Those contacts who subsequently develop clinical leprosy will suffer from primary dapsone resistance. Primary resistance can occur in both paucibacillary and multibacillary leprosy, but there is no immediate clinical or bacteriological way of identifying dapsone resistance in paucibacillary leprosy. Nevertheless, it must be assumed that primary dapsone resistance occurs in at least as many paucibacillary cases as multibacillary ones, although the multibacillary cases are relatively more important since they provide the reservoir for infection.
Primary resistance was first documented in 1977 19 and again in 1978.20 By 1979 Pearson, et al.11 had found that 5 out of 14 patients in the Addis Ababa area and 11 out of 15 from other parts of Ethiopia were suffering from primary resistance. Primary resistance was further shown in 18 out of 93 patients presenting with multibacillary leprosy at Carvillc, Louisiana, U.S.A.3 Further studies showed the following rates: The Phillipines, 3.6 per 100;21 Bamako, Mali, 35.0 per 100;22 Chingleput, southern India, 37.5 per 100.22 In some countries the strains showed a low resistance but in others, such as Malaysia, they were fully resistant. This is probably indicative of the high local prevalence of fully resistant secondary dapsone resistance. Still more worrying is the recent report that primary resistance is increasing at a faster rate than secondary resistance.3
Resistance probably occurs by a stepwise mutation.23 The early mutants have lower levels of resistance but the resistance increases with further mutation. An objective for therapy now appears to be to maintain the levels of dapsone at a high enough concentration to inhibit not only the original M. leprae population but also the 1st, 2nd, 3rd, etc., step mutants and, thus, minimize the development of fully resistant strains. The answer is to prescribe full-dose dapsone treatment and to make sure it is taken regularly. When the epidemiology of resistance has been studied, it was found that there was no obvious cause but that prolonged low-dose therapy seemed to play a role.24
These low blood levels may be caused by a number of factors. Firstly, in early chemotherapy there was a tendency to use as low a dose of sulfones as possible in order to minimize the toxic side effects and acute lepra reactions. The results seemed just as satisfactory, and so this practice gained wide acceptance. Another method was to slowly increase the dosage after the initiation of treatment, again to avoid toxicity and the development of lepra reactions. Both of these erroneous practices have now been discontinued.
Perhaps the major problem was irregular drug intake. This was largely due to poor patient compliance. It may also have been iatrogenic, for example, when therapy was continued or reduced in the hope of controlling reactions or toxicity. Unfortunately poor compliance is still a formidable problem and one of the objectives of MDT is to shorten the duration of treatment which should improve compliance.
Another cause of low serum levels was alternative sulfone preparations. Solapsone has been implicated by some in the development of resistance,25 and the use of acedapsone and other slow-release preparations have been hindered by chronically low serum levels.
It has been noted 3 that any successful program will lead to an increased number of resistant patients as those with sensitive strains are cured. However, at present the worldwide leprosy prevalence has not declined since the WHO count in 1966. In these circumstances the rise of dapsone resistance presents a serious challenge to leprosy control. It was with these problems and the resistance to other important drugs in mind that the WHO Expert Committee met in 1982 and published its new recommendations for chemotherapy. These recommendations heralded a definite switch toward MDT.
Resistance to rifampin seems to occur as a one-step process, usually within 4 years, when patients are given rifampin monotherapy.26 This suggests that it should only be used in MDT. Persisting viable bacilli have been isolated from patients receiving both rifampin alone and MDT (see below).27
There is only one recorded incidence of clofazimine resistance.28 This may have resulted from irregular intake, and the resistant strain was still sensitive to rifampin and ethionamide. Clofazimine was only used in monotherapy until the middle 1970s but now should be used in combination regimens only. It is probably as effective as dapsone in monotherapy.
Resistance to ethionamide develops in a few years if given as monotherapy, and there is crossresistance to thiacetazone and thiambutosine.29 Resistance was first suspected in a program where 7 out of 102 patients relapsed when treated with 500 mg ethionamide daily.30 Of six strains isolated from these patients, five were then found to be resistant in the mouse foot pad.31 Hence, ethionamide should only be used in MDT.
Future chemotherapy
From experience with tuberculosis it is preferred to use bactericidal agents as far as possible. With tuberculosis such drugs allow a shorter period of treatment and, when used in combination, there is less chance of developing resistant mutants. Any combination of drugs must consist of two or more effective drugs, each of which must work by a different mechanism. In addition, known resistance to any drug will invalidate its use in MDT. The drugs so far considered are relatively safe in monotherapy and in combination, with the possible exception of rifampin with ethionamide due to hepatotoxicity.
The following reasons were recently given for the failure of dapsone monotherapy:32 poor compliance, the emergence of dapsone resistance (most importantly), and the phenomenon of bacterial persistence. These problems have all been referred to earlier for dapsone monotherapy. For any new regimen to work it must prevent these same problems arising as far as possible.
The concept of compliance will be just as important to MDT, and the shorter courses of treatment with monthly supervision should be of considerable advantage in this respect. Recent studies in Ethiopia have shown compliance in MDT programs to be excellent.33
In the treatment of multibacillary leprosy, if three drugs are used there should be no resistant mutants and resistance should not occur, so MDT should prevent the development of resistant strains. Although paucibacillary cases harbor many less bacilli, MDT is still recommended due to primary resistance. Otherwise resistant patients would continue being treated until the resistance became clinically manifest. A further advantage to the paucibacillary patients is the shorter duration of treatment. Early reports of MDT in Malawi show that it may have kept drug resistance low.34
The final problem to be overcome is that of the "persisters" in multibacillary leprosy. After 3 to 4 months of dapsone therapy (50-100 mg daily) 99.9% of the M. leprae bacilli are killed in a nonresistant patient. The same occurs with clofazimine, and after only 1 week with a single dose of rifampin (600-1500 mg). It has also been observed that multibacillary cases of leprosy can relapse after treatment. A report in 1974 23 showed that 7 out of 12 patients treated for 10 to 12 years with dapsone still harbored persisting viable bacilli. This was after negative skin scrapings and negative biopsy results which were performed by conventional means. Similar "persisters" survive despite being surrounded by normally bactericidal concentrations of drugs. It is considered that they are physiologically dormant and escape ill effects. Exactly how long such organisms may last under monotherapy is uncertain. A study in Malaysia showed that in 362 multibacillary patients treated for 18.5-22 years up until 1970 with supervised dapsone monotherapy, 25 (8.8%) relapsed over the next 8-9 years. This gave an annual relapse rate of 1%,3 showing that "persisters" may survive for at least 20 years. Encouragingly though, it has been shown that relapse is more likely after short-term, supervised or unsupervised treatment rather than long-term supervised therapy.35 Similar "persister" organisms have now been isolated from patients treated with rifampin (as monotherapy or combined with thiambutosine) for 5 years36 and with clofazimine for 10 years.3
Initial studies into the elimination of "persisters" by MDT were not encouraging.36 The results from the THELEP trials (for combined drug treatment) in Bamako and Chingleput showed that "persisters" were detected in 9% of all patients, without relation to regimen, duration of treatment, primary resistance to dapsone, number of M. leprae inoculated into mice, or any other characteristic.37 Indeed, in a trial in Malta, where 200 leprosy patients were given isoniazid, rifampin, dapsone, and prothionamide for periods of between 18 and 24 months, there was only one possible relapse after 4½ years among the 80 multibacillary patients.
It has been pointed out that in order to significantly shorten the time taken to achieve a cure in tuberculosis, the drugs must be used to totally eliminate the organism.3 However, tuberculosis chemotherapy has been successful without necessarily eliminating all of the organisms. The exact importance of "persisters" is uncertain, although it is certainly preferable to eliminate them. Fortunately, recent evidence suggests that the presence of M. leprae does not carry a high risk of relapse on termination of treatment.38, 39
MDT. Studies on MDT have been encouraging to date. In China a trial of MDT on 519 patients, of whom 22.09% were fully sulfone resistant and 10.79% were recurrent cases, showed that MDT was more effective than dapsone monotherapy.40 In Wardha, India, supervised MDT therapy has reduced the prevalence rate from 11.1% in 1981 to 1.8% in 1987. The effect on disease transmission reflected in incidence rates will, however, be more gradual.41 The WHO Study Group trials of MDT in India, Malawi, Nepal, Ethiopia, Tanzania, Sierra Leone, and the Dominican Republic have shown MDT to be reasonably successful, although conclusions cannot yet be drawn. Although there are many difficulties to be sorted out, the aim must now be to spread MDT worldwide. WHO recently recorded, "...ther e is sufficient evidence available from chemotherapeutic trials and field trials undertaken by THELEP in Chingleput, Karigiri, Polambakkam, and Bamako to affirm that the WHO recommended multidrug regimens are capable of preventing and overcoming dapsone resistance. In addition preliminary data from field trials suggest that so far there is no evidence of significant relapse after completion of treatment with MDT."2 That same report criticized the implementation of MDT for being too slow, and advocated the strengthening of existing health care structures in almost all leprosyendemic countries.
With the apparent success of well implemented MDT, it may now be asked why new drugs are still needed. WHO said in its report on chemotherapy,3 "...th e armamentarium of drugs that exert bactericidal effects against M. leprae is quite limited, and there is only a small number of drugs available for use in multidrug regimens. The development of additional drugs that are bactericidal against M. leprae, and that act by mechanisms distinct from those by which the already available drugs act, is much to be desired."
At the present time, resistance has been documented to each of the drugs in current use. Resistance to all agents is also on the increase, and there is a real threat of multiple resistant strains emerging in the near future. On top of this, there exists a population of 1.6 billion people living in areas where endemicity is prevalent at a rate of over 1 per 1000. These people live mainly in poor areas where any change in their standard of living is a distant hope. Education and understanding are still not at as high a level as they could be, and so a situation has occurred in which a huge vulnerable population is exposed to the threat of potential suffering. It has also been shown that the distribution of leprosy in time is not static.42 This was shown by the epidemic in the Nauru Islands and the decline in endemicity in Europe during the Middle Ages. This presentation is, of course, sensationalist. It is very unlikely that a major global epidemic will occur, but the various control programs around the world do stand to have their painstaking work undermined. Any grip that is held over leprosy may be loosened by the development of dapsone resistance and latterly the resistance to the other drugs. For control measures, the development of new drugs must be a priority.
Any new drugs developed would be used in MDT programs with existing agents. Each new drug is then an additional safeguard against the development of multiresistant strains of M. leprae. Additionally, new drugs are sought that would be cheaper, with less side effects, easier to administer, need to be taken for a shorter duration, and may be easier to take. For a patient who objects to taking clofazimine because of the coloring, and who cannot take ethionamide or rifampin due to liver disease, dapsone monotherapy is still the only choice. New agents would allow more options in such a case and indeed in many other situations. Meanwhile, until new agents are developed, the rigorous implementation of MDT is essential.
Tactics for development of new drugs
The major concern when developing antimicrobial drugs is that of targeting. Bacteria (including mycobacteria) are prokaryotes, whereas human cells are eukaryotes. This means that bacterial cells will differ in structure and metabolism from human cells, an obvious difference being that most bacterial cells have a peptidoglycan cell wall. This particular difference is exploited by many current antibiotics, including penicillin. No harm will be done to the host cells since they do not possess a cell wall. In order to develop a drug that is bactericidal against M. leprae researchers must try to exploit its particular idiosyncracics without affecting neighboring human cells. This is especially important for an intracellular bacteria like M. leprae which prefers to remain in Schwann cells and macrophages. Several possibilities have been put forward.
Mycobacterial cell envelopes are particularly unusual. They are abnormal in having an outer membrane incorporating complex free lipids, associated with an arabinogalactan-mycolic acid matrix.43 Many of the lipid structures are species-specific, and their biosynthetic pathways represent possible targets for antibiotics. These chemical targets in mycobacteria may be considered at several different levels based on the broadness of their specificity. The highest degree of specificity is shown by serotype-specific surface lipid antigens, such as the polar glycopeptidolipids. Antibiotics which could inhibit the incorporation of these antigens' determining sugars into these lipids would be selective for single serotypes of mycobacteria. An extensive range of targets with steadily decreasing specificities have been identified. There is great potential in directing drugs at these targets but, at present, access is restricted by insufficient biochemical knowledge. An example of such an action is ethambutol, which has been reported to interfere with arabinogalactan assembly.44 Other specific drugs remain a future possibility.
Inside the cell there are no definite structures as in eukaryotic cells, and so the possible targets for drug action are the metabolic biochemical pathways. These have been reviewed recently by Wheeler,45 who has recommended attacking the synthesis of characteristic molecules from intermediates because all intermediates need not be synthesized by mycobacteria; whereas all characteristic molecules must be. Wheeler suggested four possible targets: a) the tetrahydrofolate pathway-dapsone and dihydrofolate reductase (DHFR) inhibitors; b) iron uptake-mycobacteria scavenge essential iron with high-affinity iron chelators, exochelins and mycobactins;46 these iron scavengers might potentially be poisoned; c) lipid biosynthesis-lipids form an essential part of the cell envelope with many complex pathways which must be studied in detail; and d) nucleic acid biosynthesis- mycobacteria can scavenge nucleotides,47 so drugs should be directed against the synthesis of nucleic acids from these nucleotides.
Ideally, the characteristics of new agents would be as:48 bactericidal rather than merely bacteriostatic and able to destroy "persister" organisms; effective orally; parasite specific and therefore with few side effects; and cheap to produce. Any new agent will, therefore, not just require an impressive laboratory activity but also the right pharmacokinetic and synthetic properties.
Unfortunately, there is no great financial incentive for the development of such agents and so research is underfinanced. The funding of drug research for leprosy has always been a problem. The less industrialized countries of Africa, Asia, and Latin America have about 75% of the global population. They consume (even including the oilrich nations) under 20% of the world's drug production. It has also been pointed out that only l%-3% of the international pharmaceutical industry's total research and development is devoted to tropical diseases.49 It is the countries with endemic leprosy, unfortunately, that cannot afford to spend money on drugs. This means some drugs for leprosy are "orphan drugs" and originate from developments in other more "profitable" diseases. For example, rifampin was developed for tuberculosis and was then inherited by leprosy. Jacobson50 has said that leprosy has "always been the stepchild of tuberculosis as far as drug development is concerned." It is possible though that the current concern over atypical mycobacterial infections in AIDS patients (especially M. avium-intracellulare) will spawn some new agents. These strains have been very resistant to existing tuberculosis drugs and have stimulated much research.
Another problem with drug research in the past was the lack of models on which to try new agents. The mouse foot pad test developed by Shepard51 was a major breakthrough. Other methods were also developed with mice, including the kinetic method,52 measuring the rate of intracellular ATP decay,53 and a method involving hypoxanthine incorporation.45 The use of animal models has recently been reviewed.54
Provision of bacilli in sufficient numbers has also been a problem. The closely related species of M. lufu and M. lepraemurium have been used with great success, although inconsistency across mycobacterial species is renowned. The harvesting of M. leprae from a nine-banded armadillo in large quantities has been invaluable.
Developments in drug research
Quinolones. The quinolones are congeners of nalidixic acid which is commonly used in the treatment of urinary tract infections. These agents work by inhibiting DNA synthesis during bacterial replication, probably by interference with DNA gyrase (topoisomerase) activity. The DNA of the bacterial chromosome is compacted about 8000-fold compared with the fully extended macromolecule in the "B " form. For replication and recombination, the DNA strands must separate and unwind the double helix. One of the proteins involved in the complicated unwinding is DNA gyrase. This enzyme has only been found in prokaryotic cells, and couples the hydrolysis of ATP to the introduction of negative superhelices into DNA. In the absence of ATP the enzyme behaves as a "swivelase," relaxing negative turns. Resistant mutants have an insensitive enzyme. Various analogs of nalidixic acid have been developed and have met with varying success against mycobacterial infections.
Norfloxacin and cinoxacin are two analogs with good activity against a number of gram-positive and gram-negative organisms. Ciprofloxacin and pefloxacin are two members of a newer group of quinolones that showed increased activity over gramnegative organisms and gram-positive cocci. Their use was extended to systemic infections. In a paper on the activity against aerobic and anaerobic bacteria, ciprofloxacin was described as 4-32 times more active than norfloxacin. The frequency of resistance to ciprofloxacin was 10-7-10-9.55 Both drugs were active against bacterial strains which were multiresistant to other antibiotics. Ciprofloxacin and norfloxacin were also tried against 100 various mycobacterial strains (not including M. leprae). Experiments showed that ciprofloxacin was more active against M. tuberculosis and M. fortuitum, with MICs of 1.0 and 0.25 μg/ml, respectively, against 90% of the isolates. Norfloxacin had MICs of 8.0 and 2.0 μg/ml.56 More results were obtaine rofloxacin and other 4-quinoloncs against M. tuberculosis and M. avium-intracellulare. In vitro activity of ciprofloxacin ofloxacin, amifloxacin and norfloxacin were tried against 22 isolates of M. tuberculosis. The MICs for 90% of the isolates in the case of ciprofloxacin and ofloxacin were 0.5 and 1.0 μg/ml, respectively. Amifloxacin and norfloxacin were less active. The MICs for 90% of the isolates for ciprofloxacin and ofloxacin against 20 clinical strains of M. avium-intracellulare were found to be 2.0 and 8.0 μg/ml, respectively.57 Ofloxacin has been used with other antituberculous agents with success in 5 out of 19 patients with previously multiresistant disease.58
More recently, ciprofloxacin has been shown to be effective against 5 out of 7 strains of M. avium-intracellulare in AIDS patients.59 Contributing to this effect is the fact that quinolones build up high intracellular concentrations in white blood cells. Intracellular concentration ratios of 2.4 for ciprofloxacin and 1.8 for fleroxacin have been observed (Van der Auwera, Matsumoto and Husson, 1989, unpublished data). From this, the picture certainly looks bright as far as leprosy is concerned. The problem is to find a good model for leprosy. The pharmacokinetics of the mouse frequently differ greatly from those of the human and in vitro tests with M. lufu are limited. Despite this, preliminary tests with ciprofloxacin on M. lufu in vitro did show good results, while experiments in the mouse foot pad showed that ciprofloxacin failed to inhibit growth of M. leprae. This just shows that extrapolation from one species to another, even within the same family, is not valid. The highest level of drug used in that study was slightly in excess of the equivalent recommended dose in humans.60
In a more recent study,61 the activities of pefloxacin and ciprofloxacin were tested against M. leprae in the mouse foot pad system. Once again, ciprofloxacin was disappointing in the dose given, being unable to prevent the growth of M. leprae. However, in mice treated continuously on 50 mg per kg per day of pefloxacin, growth of M. leprae was not prevented but the number of bacilli in the foot pads measured monthly remained less than in control mice. No growth at all occurred in those treated with 150 mg per kg daily. In mice treated for only 3 months with 150 mg per kg daily, the growth delay that followed cessation of the drug was 126 days, suggesting that approximately 99% of the M. leprae had been killed. The pharmacokinetics of pefloxacin are more favorable in humans with a halflife of about 10 hours in man,62 and so it emerges as a possible therapeutic agent. Unfortunately, other research in Belgium contradicts these findings.63 In this study pefloxacin showed no activity agains strains of M. leprae in the mouse foot pad system at doses of 100 or 150 mg/kg given on five days of the week. There was some activity with 300 mg/kg given on three days of the week. On the other hand, ofloxacin was bactericidal against M. leprae when administered five times a week at dosages of 150, 100 and even 50 mg per kg.
Further studies have been carried out in Japan. Investigators there64 argue that since ofloxacin has shown considerable antimycobacterial activity both in vitro65, 66 and in vivo58, 67 it should be tried in the mouse foot pad system. Ofloxacin caused a marked decrease in growth rate of M. leprae even after cessation of treatment. It can be assumed that ofloxacin is bactericidal against M. leprae. Experiments also showed that ofloxacin was bactericidal in vitro. These investigators did mention a report by Ito (summarized reports of Conference on Research on Leprosy. Sasakawa Memorial Health Foundation, Japan, 1986) that orally administered ofloxacin failed to control leprosy in two strains of mice. They also mentioned a personal communication from Grosset that supported the efficacy of ofloxacin.
More recently, Grosset, et al. have treated mice infected with M. leprae for 3 months with either 0.01% dapsone in the diet, ofloxacin 50 or 150 mg/kg, pefloxacin 150 mg/kg, or 50 mg/kg prothionamide.68 The organisms did not multiply initially but resumed growth in the fourth month after cessation of therapy, except in those administered ofloxacin 150 mg/kg. This showed the bactericidal activity of ofloxacin, killing all viable organisms at this dose. Indeed, no growth was detectable at 18 months. The only existing agent to match this is rifampin. This dosage is equivalent to 400 mg in man which is the usual dose.69 This was very encouraging since pefloxacin, which is less active in the mouse but has very similar pharmacokinetic properties, has already been shown to be strongly active in the treatment of previously untreated multibacillary leprosy.70
Ito, et al. have tried ofloxacin for activity against M. leprae in both normal and nude mice.71 They found that in nude mice ofloxacin for 100 days at 0.025% was slightly effective but at 0.05% and 0.075% it showed significant depression. In normal mice 0.075% had no effect but treatment with 1 mg of ofloxacin six times a week for 100 days (equivalent to 0.025% in diet) showed significant depression of growth.
In summary, there certainly appear to be some promising developments with the new quinolones. Thus, in a recent pilot trial in the Ivory Coast, where 10 multibacillary patients received 400 mg pefloxacin twice daily, no viable M. leprae from skin biopsies from the patients after only 4 months' treatment were detected in normal or nude mice72 These quinolones are orally administered, and also act by a mechanism different from existing agents and would add an extra dimension to MDT. Side effects for ciprofloxacin are not common, but there has been a report of antagonism between quinolones and rifampin.71 Unfortunately, these agents are very expensive at present, hindering distribution in many countries. The half-life is only about 10 hours, which necessitates daily treatment. Hopefully there will be much more research into the quinolones which will yield more effective and cheaper drugs. Perhaps some of the newer quinolones may prove effective. The quinolones are extremely effective broad-spectrum antibiotics and therefore of much interest for the drug companies. It can only be hoped that an effective antileprotic agent emerges as a spin-off.
DHFR inhibitors. Dapsone is thought to inhibit the dihydropteroate synthetase reaction, unique to bacteria. A subsequent step in the reaction sequence involves DHFR and this also occurs in eukaryotic cells, hence targeting is more difficult. Failure to reduce dihydrofolate causes depletion of active folate with the consequent cessation of DNA synthesis, ultimately leading to cell death. Drugs such as trimethoprim and pyrimethamine have been used against bacteria and protozoa, respectively. If a drug could be found that was specific to mycobacterial DHFR then a potential drug for leprosy might be found. Trimethoprim itself has been tested on mycobacterial strains with little success. A German study74 showed that most nontuberculous mycobacteria (M. leprae was not tested) were resistan methoprim. Similar experiments in the U.S.A. confirmed that trimethoprim was inactive against M. cheloni.75 Trimethoprim in combination with sulfamethoxazole (a sulfonamide) remains the treatment of choice for infections by M. marinum. 76
Trimethoprim was found to be ineffective against M. leprae in the mouse foot pad.77 A new series of DHFR inhibitors, the 2,4-diaminoquinazolines, were found to be effective against Mycobacterium sp. 607 (experimental strain). In combination, it was found that the MIC of the quinazoline was reduced by eightfold and that of dapsone by 20-fold.78 Further experiments showed that the 2,4-diaminoquinazolines were effective against M. leprae in the mouse foot pad.79 During early administration of these drugs, the multiplication of M. leprae was prevented but later, while the mice were still receiving the drug, multiplication resumed at a normal rate. Two quinazolines were studied, SRI 105 and SR 168. Dapsone and SRI 105 were bacteristatic; while dapsone and SR 168 had bactericidal potential. Further experiments showed that the quinazolines were not bactericidal nor could any synergy with dapsone be demonstrated. A later compound H 1 did seem to be bactericidal and possess synergy with dapsone.80 Since then, surprisingly, trimethoprim has shown to have considerable activity against isolated DHFR from mycobacteria, indicating a limited permeability of the mycobacterial cell wall to the drug.
Proof that the mycobacterial DHFRs are different from other bacterial DHFRs was recently documented. Researchers isolated the DHFR from M. phlei and showed it to have a different relative molecular mass (15 kDa) and a different isoelectric point (pI = 4.8) to that of Escherichia coli.81 The X-ray structure of E. coli DHFR shows a positively charged arginine moiety in the cavity of the active center.82 Experiments with trimethoprim analogs bearing more negative substituents lead to increased activity against the isolated enzyme. Such compounds have permeability problems with intact bacteria. Synthesis of more lipophilic derivatives with negatively polarized but unionized groups, such as K 130, have shown activity against M. lufu.
Tests on M. leprae in the mouse foot pad models have also shown inhibition. This effect is delayed, despite blood concentrations well above the MIC for K 130, and is not too alarming since the same problem arises with trimethoprim against gram-negative bacteria. This simply emphasizes the limitations of the mouse model. Other tests on M. leprae suspensions measuring the inhibition of tritiated thymidine uptake and ATP levels show similar inhibition by both K 130 and K 128.83
Dapsone analogs. Research has been carried out to sec whether an analog of dapsone could produce a more useful compound.83 By using different substituted groups at strategic positions in the basic diaminodiphenyl sulfone molecule, it is possible to alter the lipophilic, electronic and steric properties. The aim of this manipulation was primarily to increase the activity against M. leprae but, also, to improve other characteristics of the drug. This research has been greatly assisted in recent times by "quantitative structure-activity relationship" analysis. This allows, with computer help, a deeper understanding of the chemistry of drug action without necessarily having to synthesize the drug. Using these techniques on dapsone and its analogs has not proved very rewarding in tests on cell-free systems. Unfortunately, only a small increase in activity has been possible. From this study it seems that only the electronic and steric effects of the substituents seem to be important in determining the observed differences in activity.
The same research has shown that the susceptibility of the vulnerable enzyme (dihydropteroate synthetase) was the same in both resistant and sensitive strains of M. leprae. The conclusion from this is that resistance docs not occur by modification of the target enzyme.
Changes in lipophilicity were not found to be responsible for the observed changes in activity in these cell-free systems, but such changes do effect renal clearance-so the pharmacokinetic properties can be altered, i.e., increased lipophilicity and increased half-life. This could be used to adapt the pharmacokinetics of dapsone derivatives to those of other drugs used in combination. A bonus of this research was the finding that some of the more active derivatives may give reduced toxicity, i.e., reduced methemoglobin formation.
This research has produced some interesting results but in some respects was disappointing. No great increase in bactericidal activity was found and it must be remembered that any new agent will still be restricted in use by dapsone resistance since it will work by the same mechanism. Although possibly useful in the short term to reduce toxicity or to manipulate pharmacokinetics, such agents are unlikely to play a part in long-term leprosy control due to the problem of dapsone resistance.
Ansamycins. Rifamycin, a natural antibiotic from streptomyces, was the forerunner of rifampin. Other derivatives of rifamycin that have been employed more recently are the ansamycins. In 1983, a letter published in The Lancet84 described the in vitro activity of a new ansamycin (LM 427), a derivative of rifamycin S, against M. tuberculosis. Studies had shown that LM 427 was 6-7 times more potent than rifampin in mice and, furthermore, had shown activity against rifampin-resistant strains of M. avium in vitro. This offered the possibility of a new therapeutic agent without crossresistance to any of the existing agents, despite working in a similar fashion to rifampin. LM 427 was then tried on M. leprae from newly diagnosed multibacillary cases in the mouse foot pad system. It was active against 6 out of 6 strains at concentrations of 0.3 parts per million in the mouse diet. This minimum concentration was significantly less than the equivalent dose of rifampin. Next, LM 427 was tried on rifampin-resistant strains of M. leprae in the mouse foot pad.85 The results were extremely encouraging; growth was prevented even at the lowest doses.
Similar results were found in other mycobacterial species. Only 13% of M. avium strains that were rifampin resistant were found to be resistant to low doses of ansamycin, and these were strains that had been highly resistant to rifampin. However, extensive crossresistance was found with rifampin-resistant M. tuberculosis strains.86
A study in China87 took some of the new ansamycins and screened them both in vitro for activity against cultured mycobacteria and then in vivo against M. lepraemurium. Compounds comparable or superior to rifampin were then tried against M. leprae in the mouse foot pad. Two ansamycins proceeded to the second test, R-76-1 and DL 473 (rifapentine). Against the cultured mycobacteria the MIC of R-76-1 was eight times less than rifampin. With the mice infected with M. lepraemurium R-76-1 was three times more effective than rifampin. DL 473 was also more effective in that it could be given in fewer doses and had a longer-lasting effect than rifampin. Using the kinetic test method and 0.001% of drug in the diet, R-76-1 was bactericidal against M. leprae. Using the proportional bactericidal method, a single dose of 1.25 mg of DL 473 per kg was active against M. leprae; whereas the smallest active dose of rifampin was 10 mg per kg. Most encouraging of all was a small clinical trial with R-76-1. This was conducted on 20 patients with multibacillary leprosy. Of these, 10 strains had been tested in the mouse foot pad for resistance; 7 were fully resistant to dapsone and 1 was resistant to both thiambutosine and thiacetazone. At a dosage of 150 mg daily, the treatment was very effective. Side effects included jaundice in two patients which may have been unrelated. Unfortunately, severe erythema nodosum leprosum reactions occurred.
A more recent study88 has compared the activity of rifabutine and another ansamycin, rifapentine, with rifampin. Activity was tested in the mouse foot pad. Rifabutine and rifapentine were found to be eight times more active against M. leprae than rifampin when given in a single dose.
A new derivative 3-rifamycin SV (RFD, R-773) has been tested on five cases of multibacillary leprosy with some success. Before treatment, all of the bacilli from the patients were able to infect mice and the number of bacilli increased from 11.3 to 80 times. Bacilli taken after day 7 of treatment did not infect the mice and multiplied only slightly in three cases.89 Good clinical and bacteriological effects were also seen in 45 multibacillary patients treated by combination RFD, clofazimine, and dapsone for 1-2 years.90
There is little doubt that these agents are promising. They will probably be expensive, like rifampin, but with their increased activity they may be given at a lower dosage with perhaps fewer side effects.
Cephalosporins. Cephalosporins, like the penicillins, are beta-lactam antibiotics. They work by inhibiting the bacterial transpeptidase enzyme which is responsible for cellwall synthesis. Penicillins are inactive against M. leprae. This is due to the development of beta-lactamases which are rapidly induced on exposure to penicillins.91 However, cephalosporins are resistant to most of the existing beta-lactamases.
The in-vitro activity of cephalosporins against mycobacteria has been reported.92 It was found the cephalosporins with pyridyl or aminomethyl phenyl moieties in the seven position were active against M. tuberculosis. This was confirmed,93 and a hierarchy of activity against M. tuberculosis established-ceforamide, cephapirin, cephalothin, cephazolin, cephalexin, etc., with diminishing activity. A similar ranking or der was found for activity against M. kansasii and M. avium-intracellulare, although the MICs were higher than for M. tuberculosis. More recently, a study found that ceforamide, ceftizoxime, cephapirin, and cefotaxime have good activity against M. tuberculosis, in descending order.94 Another study has shown that cefoxitin is active against M.fortuitum although less so against M. chelonei.95 (Cefoxitin is strictly a cephamycin but these are closely related to ceph alosporins.)
In 1967 it was reported that cephaloridine was effective against M. leprae in mice in doses of 300 mg/kg daily.96 Then, in 1971, a report showed both cephaloridine and cephaloglycin to be bactericidal against M. leprae by the kinetic method. Cephalexin was found to be ineffective in similar doses.97
More recently the activity of selected betalactam antibiotics were tried against M. leprae in mice by the kinetic method.98 It was found that significant inhibition of growth was obtained with 7-aminocephalosporanic acid, cephaloglycin and cefuroxime but the most effective agents were cefoxitin and cephaloridine. These results showed that a particular molecular structure may be required for maximal activity against M. leprae since the most successful drugs shared common moieties. This has obvious implications in future drug development, and further optimization of this structure may produce exciting new drugs. Unfortunately, some of the cephalosporins have to be injected which will hinder use in remote locations, and the newer drugs are exceptionally expensive at the moment. With more research it can be hoped that more active, orally administered derivatives may become available.
Minocycline. The tetracyclines are a group of antibiotics that inhibit bacterial protein synthesis. They do this by binding to the 30S ribosomal subunit of bacteria, but they will also inhibit eukaryotic protein synthesis at higher concentrations. Their action is specific to bacterial cells, however, because of selective absorption. Tetracyclines have already been shown to be ineffective against M. leprae.96
Minocycline is the most lipid soluble of the tetracyclines. It is a semisynthetic derivative that became available in 1972, and it is especially active against aerobic bacilli.99 Minocycline has been shown to be active against M. marinum,100 and it is also the most active tetracycline against M. tuberculosis.101 Minocycline is more active against slow-growing mycobacteria than rapid-growing strains.101
In a recent study,102 minocycline was found to be active against M. leprae infection in mice. The plasma MIC was exceedingly low (< 0.2 μg/ml), much lower than the MIC previously found for other bacteria.101 Higher concentrations led to greater activity. Fortunately, these levels are well within the clinically achievable range (2-4 μg/ml).103 Minocycline proved to be more bactericidal than all other currently used drugs except rifampin but, more importantly, its effect was additive with other agents including dapsone and particularly rifampin.
The activity of minocycline against M. leprae is probably due to its lipid solubility at neutral pH. It is thus able to penetrate the outer capsule and cell wall.104 It is 30 times more lipid soluble than tetracycline. Another consequence of this property is its excellent penetration of the tissues, including the skin and neural tissue, both crucial in the case of leprosy. Studies show that the usual dose of 100 mg twice a day results in dermal concentrations of 2-3 μg/ml and epidermal levels of 4-6 μg/ml.103 On the negative side there are reports of vestibular toxicity.105 However, this usually occurs immediately, if at all, and is reversible after cessation of treatment. In addition, longterm therapy has been successful in the treatment of acne. A clinical trial is soon to take place, and the prospects are promising since it would be cheaper than rifampin and would also work well in existing regimens of MDT. Furthermore, it is given orally.
Aminoglycosides. These drugs exert antimicrobial actions by binding the 30S ribosomal subunit; some also bind to the 50S subunit, and here they inhibit protein synthesis and impair the fidelity of RNA translation. Actions against M. tuberculosis are well known, and actions were also discovered against M. leprae. There were reports of successful animal studies,106, 107 and successful trials of streptomycin were completed in Malaysia.108 Further activities of kanamycin and amikacin have also been shown.109 Amikacin is particularly active against M. avium-complex infections.110 Unfortunately, aminoglycosides are not absorbed on oral administration, and animal studies involving intraperitoneal injections are not very practical on a large scale. Additionally, the doses used were high and could potentially cause renal and acoustovestibular damage in chronic therapy.
A recent study111 tested the bactericidal activity of kanamycin and streptomycin in lower, potentially therapeutic, doses. Using high doses (100 mg/kg) both agents are bactericidal. At lower doses, kanamycin lost significant bactericidal activity but streptomycin was still effective, although to a lesser degree. Reducing the frequency of streptomycin administration maintained a reduced but significant level of bactericidal activity. Finally, streptomycin, when combined with rifampin, was found to be synergistic, even when given only once a month. The author proposed that monthly streptomycin might present an alternative to clofazimine in MDT, and it could be admin-istered once a month to multibacillary patients with rifampin.
Deoxyfructo-5-hydroxytryptamine (DF5-HT). DF5HT is a human metabolite, first detected in man in 1981.112 This new agentshowed antileprotic activity on bacillary suspensions in vitro113 and in the mouse footpad system.114 DF5HT is bacteristatic rather than bactericidal.115 It was shown to have an extremely low toxicity (1200 mg/kg in mice by oral administration). No toxicity was found at 200 times the clinical dose in man, and a small pilot study in Bamaha, India, showed a good clinical response in seven patients.116 Activity has also been shown against bacilli in Schwann cells of a nerve culture and in macrophages from multibacillary patients. Tests also showed enhanced lymphocyte-macrophage interaction promoted by the drug. This may be the result of a stimulus to the cell-mediated immunity. Protection against sciatic nerve damage was also shown for the mouse.115 Most recently, a trial was conducted in India,117 giving 10 mg/kg to six patients with multibacillary leprosy for 6 months. Compliance was checked with a marker. Improvement occurred in 5 out of 6 patients in both clinical and histological terms. In some cases, DF5HT showed an ability to clear bacilli faster than dapsone. This may be due to an immunostimulating effect.115 The variations in response may be due to variations between metabolites of the drug (itself a metabolite).
Both dapsone and rifampin are immunosuppressive and the addition of an immunopotentiating drug may shorten the duration of treatment. The neuro-protective effect of DF5HT has great therapeutic potential. Researchers are also looking for other human metabolites, such as dcoxyfructo-5hydroxytryptophan and some lipid soluble derivatives of DF5HT. The time of resorption and penetration into M. leprae-infected tissues is very different for these metabolites, and simultaneous application may yield some advantages in the treatment of multibacillary leprosy.
Clofazimine derivatives. It has been shown that host defense against mycobacterial infection depends largely on the efficacy of the myeloperoxidase-hydrogen peroxide-halide system.118 Clofazimine has been found to increase the release of these reactive oxidants.119 This is probably partly responsible for both its immunosuppressive and antimycobacterial properties.120 Immunosuppression may also be due to stimulation of prostaglandin E2 (PGE2) production in white cells.
Research into new compounds was done recently as part of a WHO project to develop new analogs of clofazimine. It was hoped that these might be active against clofazimine-resistant strains of M. leprae and also less toxic. The new compounds B3691, B3713, B3640, and B3648 were developed and have been shown to have activity against clofazimine-resistant strains of M. smegmatis (0.4-2.0 μg/ml).121 The clofazimine analogs exerted similar levels of inhibition of M. leprae strains in peritoneal macrophages of mice. At lower concentrations and shorter exposures (48 hours), clofazimine was more effective than the analogs. Among the analogs, B3691 appeared most promising. There were also problems with absorption. Experiments with 10 phenazine derivatives showed spatially distinct sites for action on PGE2 production and antimycobactcrial activity.122
Similar results have been obtained elsewhere. The analogs require a basic nitrogen in the "rimino" side chain, and a specified gap between this nitrogen and the imino nitrogen. These analogs also showed activity against infected mouse macrophages.123
More recently, activities of various phenazines against M. leprae were investigated in vitro using a radiorespirometric assay. This showed an increased activity, in ascending order, for compounds containing no chlorine atoms, a monochlorinated phenazine nucleus, and chlorines in the para positions of both the anilino and phenyl ring. The most active compounds contained a 2,2,6,6-tetramethyl piperidine substitution at the imino nitrogen. Most of the chlorinated phenazines were much more active than clofazimine in vitro.124
Mycobacterial ribonucleotide reductase (MRR) inhibitors. It has long been known that thiacetazone is active against M. leprae. It has also been found with related thiosemicarbazones (TSC) that manipulation of the nitrogen atom in the alpha position results in varying activities against M. lufu strains; TSCs lacking the nitrogen atom are less active.125 The literature suggests that these metal ion chelaters act as inhibitors of the iron-containing bacterial enzyme MRR. In addition to this, the toxicity of acylpyridine-TSCs has been considerably reduced by replacing their thioamide group by different N-hetrocycles.125 This has led to the development of a new compound, PH22, which also has increased antibacterial activity and chelating properties. In accordance with the hypothesized mode of action, it was found that PH22 derivatives are very potent inhibitors of DNA synthesis. Interestingly, a very pronounced synergism between PH22 and several other drugs known to be inhibitors of the DNA synthesis pathway was found.
Long-acting dapsone injections. This method of dapsone administration has often been used in chemoprophylaxis with mixed results. Potentially, this form of administration could be very promising in the treatment of leprosy. It has already been noted that one of the major reasons for the downfall of sulfone monotherapy was the lack of compliance. Lack of compliance indirectly contributed to the development of sulfone resistance. Theoretically, a slow-release dapsone repository placed intramuscularly could be of major therapeutic significance. These injections are given every few months, and a serum dapsone concentration well above the MIC is maintained between injections. Patients then only have to visit the clinic every few months.
A paper published in 1968 126 reported that the growth of M. leprae could be inhibited by unexpectedly low doses of dapsone. At the same time, repositories were being tried for malaria and experiments were performed on mice. One agent, 4,4'-diacetyldiaminodiphenyl sulfone (DADDS or acedapsone), was active when given every 2 months in a dose of only 6 mg/kg. The repository nature of DADDS arises from its insolubility in aqueous solvents and in the vehicle in which it is suspended for injection. Active dapsone is slowly released by tissue enzymes. When DADDS was tested for efficacy against multibacillary leprosy, it was found to be just as effective as dapsone in a controlled trial, although the blood sulfone level was much reduced (usually less than 0.2 µg/ml). This level was still higher than the MIC as determined in mice. A later report showed that of 10 multibacillary patients receiving DADDS, 3 improved as fast as a dapsone control group and 7 improved more slowly.1 27
The low plasma levels produced by acedapsone were a disadvantage (it is estimated that 225 mg every 11 weeks is equivalent to 2 mg per day of dapsone). Such low concentrations encouraged the emergence of resistant strains of M. leprae. The use of such low-dose injections has declined, although they are occasionally used in MDT, e.g., with rifampin.
The potential for a powerful therapeutic agent still remains with injectable preparations because of the reduced requirement for compliance. WHO3 stated that ". . . formulation of dapsone or a derivative of dapsone, that, on monthly administration, would provide bactericidal concentrations of dapsone within the tissues without the risk of toxicity is desirable." Much research has since been done to find a method of slow release that would maintain concentrations at higher levels without toxicity. More recent studies,128 showed that long-acting injections gave much better results in women. Satisfactory blood concentrations were obtained for women; whereas the levels were unacceptable in men.
An answer to this problem was offered by Cockshott, et al.129 who showed, with CT scans of the gluteal region, that due to the thicker adipose layer in females intramuscular injections are, in fact, delivered intra-adipose. This theory was confirmed by a group130 who delivered injections into adipose tissue in both sexes and found no significant difference in subsequent dapsone plasma concentrations. Encouragingly, the results for both sexes showed the maintenance of bactericidal concentrations of dapsone (injections = 1000 mg). They advocated the future use of intra-adipose injections.
Slow-release preparations have always been erratic. A recent study131 attempted to correlate the response to DADDS with the number of bacilli in skin smears in multibacillary patients prior to therapy. An analysis of the data failed to show any correlation. The development of slow-release preparations is a complex process, and the physical properties, such as solubilities, partition coefficients and crystal properties, must be balanced to obtain the desired pharmacokinetics. As a result, many different groups have been tried as modifications of the basic dapsone structure.132
One such example is monoacetyldapsone (MADDS). MADDS is the major metabolite of dapsone in blood. It has a lower aqueous solubility than dapsone, and so might be more suitable. Also, different crystal properties might lead to better "syringeability" of the injection. In earlier experiments, similar discrepancies between males and females were noticed133 but a subsequent intra-adipose study showed almost perfect zero order release that produced lower dapsone concentrations for a longer period of time than dapsone injections themselves.134 More recently, in two field trials in Nigeria 74 men and women received intra-adipose injections of either dapsone or MADDS.135 Dapsone was successful, reasonable concentrations were maintained, and the only side effect was an injection abscess. With MADDS, better sustained-release results were obtained but, unfortunately, a number of abscesses occurred at injection sites. Depot injections of dapsone certainly show great therapeutic potential and, with more development, MADDS may also become practical.
Macrolides. Macrolides, of which erythromycin is the best known example, bind the 50S ribosomal subunit in susceptible organisms and thereby inhibit protein synthesis. Their activity against mycobacteria has been reported previously.136 Potent activity of erythromycin has been demonstrated against M. leprae in vitro as determined by the measurement of intracellular ATP,137 radiorespirometric assay of palmitate oxidation,138 and measurement of the rate of PGL-I synthesis.139 However, in the mouse foot pad, erythromycin has failed to inhibit growth of M. leprae. This may be due to poor pharmacokinetics. The acid lability of erythromycin in humans can be avoided by enteric coating, but its half-life is still far too short (1.1-3.5 hours) to be used against leprosy.
Experiments were recently performed to assess new semisynthetic macrolides with superior acid stability and longer half-lives, both in vitro and in vivo.140 Both clarithromycin and roxithromycin proved more potent than erythromycin in vitro; clarithromycin showed the greater activity. In vivo in mice, clarithromycin showed the highest concentration; whereas erythromycin was undetectable even when administered at 0.1 % (w/w) in the diet. When given at 0.01 % (w/w) in the diet, erythromycin and roxithromycin were unable to inhibit growth of M. leprae; whereas clarithromycin showed bactericidal activity. On this basis, a clinical trial of clarithromycin in leprosy is awaited.
Additionally, macrolides are orally active, relatively cheap, do not require refrigeration, possess low toxicity, concentrate intracellularly, and act at a distinct site from other agents.
Pyrazinamide. Pyrazinamide in combination therapy has been shown to be active against persisters in tuberculosis. Although it shows no inhibitory effect against M. leprae in the mouse foot pad when used alone,141 this docs not necessarily mean that it will be inactive as part of a therapy combination in humans. Since it is thought to act in the acidic environment of the macrophage to inhibit M. tuberculosis,142 it may be of some use in leprosy.
Recently, it was tried as part of combination therapy in multibacillary patients143-63 BL and LL patients were given 1500 mg of pyrazinamide as part of different drug regimens for the first 2 months; 51 other BL and LL patients were put on similar regimens without pyrazinamide. After 2 years, those on pyrazinamide had a morphological index (MI) of 0; those who did not receive it still had some solidly staining bacilli. Five percent of the biopsies of smooth muscle in the pyrazinamide group produced growth in mouse foot pads compared with 23.7% of the controls. After 5 years, the pyrazinamide group was still slightly better off. The ability of pyrazinamide to eliminate persisters may be of use clinically. A longer trial is necessary.
Conclusion
This review has attempted to explain the need for new drugs in the treatment and control of leprosy. To understand the immediacy of this requirement, it is first necessary to establish why drugs are the only answer to present needs. This requires an understanding of the epidemiology of leprosy. Such a study reveals that epidemics have occurred in susceptible populations, and also that there is a vast population, namely 1.6 billion people, living in "at risk" areas. Once these points are appreciated, it can be seen that it is very important to establish control in the present situation. This can only be done with painstakingly thorough measures.
Man's intervention in the disease process, which at first promised to be decisive, as with so many other infectious diseases, has been undermined by the development of dapsone resistance. The implementation of MDT will do a great deal to regain the initiative, but undoubtedly problems with resistance, compliance and persistence will hinder progress. The way forward lies in three major areas: the development of new drugs, the development of an effective vaccine, and the meticulous implementation of MDT.
New drug treatments, in particular, could drastically afreet the state of the disease in the world today and, by doing so, relieve the suffering of thousands. All of these new agents are still a few years from widespread use but, fortunately, there are some promising candidates. Exactly which drugs will emerge from the clinical trials cannot be predicted, but it can only be hoped that they are cheap, easy to use, and nontoxic.
Finally, it should be remembered that high technology has a limited role to play in leprosy. The areas of the world that need these new drugs are not the medical oases of America and western Europe but countries with environments that demand a much more pragmatic understanding.
- Richard J. Baker
1. Sansarricq, H. Leprosy in the world today. Lepr. Rev. 52 Suppl.1(1981)15-31.
2. World Health Organization. Wkly. Epidem. Rep. 62(1987)101-108.
3. WHO Study Groups. Chemotherapy of leprosy for control programmes. Geneva: World Health Organization, 1982. Tech. Rep. Ser. 675.
4. Hertroijs, A. R. A study of some factors affecting the attendance of patients in a leprosy control scheme. Int. J. Lepr. 42(1974)419-27.
5. Low, S. J. M. and Pearson, J. M. H. Do leprosy patients take dapsone regularly? Lepr. Rev. 45(1974)218-223.
6. Hagan, K.J., Smith, S.E., Gyi, K. M., Lwin, M. M., Myaing, Y. Y., Shwe, T., Tin, K. M., Than, K. N., HIa, T. and Kywe, W. W. The reliability of self-administration of dapsone in leprosy patients in Burma. Lepr. Rev. 50(1979)201-211.
7. Pettit, J. H. S. and Recs, R. J. W. Sulphone resistance in leprosy. Lancet 2(1964)673-674.
8. Pettit, J. H. S., Ridley, D. S. and Rees, R. J. W. Studies on sulfone resistance in leprosy. Int. J. Lepr. 34(1966)375-390.
9. Meade, T. W., Pearson, J. M. H., Rees, R. J. W. and North, W. R. S. The epidemiology of sulfone resistant leprosy. Abstract in Int. J. Lepr. 41(1973)684.
10. Pearson. J. M. H., Rccs, R. J. W. and Waters, M. F. R. Sulphone resistance in leprosy; a review of one hundred proven clinical cases. Lancet 2(1975)69-72.
11. Pearson, J. M. H., Haile, G. S., Barnetson, R. St. C. and Rees, R. J. W. Dapsone resistant leprosy in Ethiopia. Lepr. Rev. 50(1979)183-199.
12. Peters, J. H., Shepard. C. C, Gordon. G. R., Rojas, A. V. and Elizondo, D. S. The incidence of DDS resistance in lepromatous patients in Costa Rica: their metabolic disposition of DDS. Int. J. Lepr. 44(1976)143-151.
13. Levy, L., Rubin, G. S. and Sheskin, J. The prevalence ofdapsone resistant leprosy in Israel. Lepr. Rev. 48(1977)107-112.
14. WHO Expert Committee on Leprosy. Fifth report. Geneva: World Health Organization, 1977. Tech. Rep. Scr. 607.
15. Taylor. P. M., Chacko, C. J. G. and Job, C. K. Study of sulphone resistance in leprosy patients in India. Lepr. Rev. 47(1976)5-11.
16. Balraj, V., Jesudasan, K., Chacko, C. J. G., Christian. M., Taylor, P. M., Fritschi, E. P. and Job, C. K. Prevalence of secondary dapsone resistance in Gudiyattam Talak, the leprosy control area of the Schieffelin Leprosy Research and Training Centre, Karigiri. 1. Preliminary report. Int. J. Lepr. 48(1980)397-401.
17. Li, W. H., el al. [Clinical and experimental studies on sulfone resistant leprosy.] Chin. J. Dermatol. 14(1981)75-79.
18. Baquillon. G., Ferracci, C, Saint-Andre, P. and Pattyn, S. R. Dapsone-resistant leprosy in a population of Bamako (Mali). Lepr. Rev. 51(1980)315-319.
19. Pearson, J. M. H., Haile, G. S. and Rees, R. J. W. Primary' dapsone resistant leprosy. Lepr. Rev. 48(1977)129-132.
20. Jacobson, R. R. and Hastings, R. C. Primary sulfone resistant leprosy. Abstract in Int. J. Lepr. 46(1978)116.
21. Guinto, R. S., Celona. R. V., Fajardo, T. T. and dela Cruz, E. C. Primary dapsone-rcsistant leprosy in Cebu, Philippines. Int. J. Lepr. 49(1981)427-430.
22. WHO Subcommittee of Chemotherapy of Leprosy (THELEP). Primary resistance to dapsone among untreated lepromatous patients in Bamako and Chingleput. Lepr. Rev. 54(1983)177-183.
23. Hastings. R. C. Growth of sulfone-resistant M. leprae in the footpad of mice fed dapsone. Proc. Soc. Exp. Biol. Med. 156(1977)544-545.
24. Jacobson, R. R. The clinical aspects of dapsone resistance. In: A Window on Leprosy. Chatterjee, B. R., ed. Calcutta: The Statesman Commercial Press. 1978, pp. 146-152.
25. Gelber, R. H., Gooi, H. C, Waters. M. F. R. and Rees, R. J. W. The pharmacology of Sulphetrone and its implications in sulphone resistance. Lepr. Rev. 45(1974)308-312.
26. Jacobson, R. R. and Hastings, R. C. Rifampicin resistant leprosy. Lancet 2(1976)1304-1305.
27. Waters. M. F. R., Rccs. R. J. W., McDougall, A. C. and Weddell, A. G. M. Ten years of dapsone in lepromatous leprosy; clinical, bacteriological and histological assessment and the findings of viable leprosy bacilli. Lepr. Rev. 45(1974)288-298.
28. Warndorff-Van Diepen, T. Clofazimine resistant leprosy-a case report. Int. J. Lepr. 50(1982)123-127.
29. Pattyn, S. R. and Colston, M. J. Cross-resistance amongst thiambutosine, thiacetazone, ethionamide and prothionamide with Mycobacterium leprae. (Letter) Lepr. Rev. 49(1978)324-326.
30. Rollier, R. and Rollier, M. Traitement de la lèpre lépromateusc par l'éthionamide. Maroc Med. 52(1972)148-166.
31. Pattyn, S. R., Rollier, M.-T., Rollier, R. and Verdoolaeghe-Van Loo, G. Sensibilité envers la dapsone, la sulfamethoxypyridine et l'éthionamide, de Mycobacterium leprae provenant de malades traités par ces substances. Int. J. Lepr. 43(1975)356-363.
32. Waters, M. F. R. Concepts behind the development of multidrug therapy regimens in leprosy. Lepr. Rev. 57 Suppl.1(1986)61-67
33. Becx-Bleumink, M. Implementation of MDT in the ALERT leprosy programme in the Shoa region of Ethiopia; first results with paucibacillary patients. Lepr. Rev. 57(1986)111-119.
34. Boerrigter, G. and Ponnighaus, J. M. Ten years' leprosy control work in Malawi (central Africa)-I. Methods and outcome after treatment. Lepr. Rev. 57(1986)199-219.
35. Touw-Langendijk, E. M. J. and Naafs, B. Relapses in leprosy after release from control. Lepr. Rev. 50(1979)123-127.
36. Waters, M. F. R., Rees, R. J. W., Pearson, J. M. H., Laing, A. B. G., Helmy, H. S. and Gelber, R. H. Rifampicin for lepromatous leprosy: nine years' experience. Br. Med. J. 1(1978)133-136.
37. Subcommittee on Clinical Trials of the Chemotherapy of Leprosy (THELEP) Scientific Working Group. Persisting Mycobacterium leprae among THELEP trial patients in Bamako and Chingleput. Lepr. Rev. 58(1987)325-337.
38. Waters, M. F. R., Rees, R. J. W., Laing, A. B. G., Fah, K. K., Meade, T. W., Parikshak, N. and North, W. R. S. The rate of relapse in lepromatous leprosy following completion of twenty years of supervised sulphone therapy. Lepr. Rev. 57(1986)101-109.
39. Jopling, W. H., Ridley, M. J., Bonnici, E. and Depasquale, G. A. A follow-up investigation of the Malta-Project. Lepr. Rev. 55(1984)247-253.
40. Chen, D. MDT in China. China Lepr. J. 2(1986)28-29.
41. Jesudasan, K., Vijayakumaran, P., Pannikar, V. K. and Christian, M. Impact of MDT on leprosy as measured by selective indicators. Lepr. Rev. 59(1988)215-223.
42. Wade, H. W. and Ledowsky, V. The leprosy epidemic at Nauru: a review with data on the status since 1937. Int. J. Lepr. 20(1952)1-29.
43. Minnikin, D. E. Lipids: complex lipids, their chemistry, biosynthesis and roles. In: The Biology of the Mycobacteria. Vol. I. Physiology, Identification, and Classification. Ratledge, C. and Stanford, J. L., eds. London: Academic Press, 1982, pp. 95-184.
44. Takayama, K. and Kilburn, J. O. Inhibition of synthesis of arabinogalactan by ethambutol in G. and Mycobacterium smegmatis. In: Nineteenth Joint Research Conference on Tuberculosis. U. S.-Japan Cooperative Medical Science Program, Tokyo, Japan, 1984, pp. 162-177.
45. Wheeler, P. R. Metabolism in M. leprae: possible targets for drug action. Lepr. Rev. 57 Suppl. 3(1986)171-181.
46. Barclay, R. The role of iron in infection. Med. Lab. Sci. 42(1985)166-177.
47. Khanolkar, S. R. and Wheeler, P. R. Purine metabolism in M. leprae grown in armadillo liver. FEMS-Microbiol. Lett. 20(1983)273-278.
48. Hooper, M. The search for new drugs for the treatment of leprosy. Lepr. Rev. 56(1985)57-60.
49. Taylor, D. G. and Griffin, J. P. Drug development and delivery programmes for the third world. In: Orphan Diseases and Orphan Drugs. Fulbright Papers, Volume 3. Herbert Scheinberg, I. and Walshe, J. M., ed. Manchester: Manchester University Press, 1986, pp. 178-179.
50. Jacobson, R. R. Treatment. In: Leprosy. Hastings,R. C., ed. New York: Churchill Livingstone, 1985, p.219.
51. Shepard, C. C. The experimental disease that follows the injection of human leprosy bacilli into thefootpads of mice. J. Exp. Med. 112(1960)445-454.
52. Shepard, C. C. A kinetic method for the study ofactivity of drugs against M. leprae in mice. Int. J. Lepr. 35(1967)429-435.
53. Franzblau, S. G. and Hastings, R. C. Rapid in vitro metabolic screen for antileprosy compounds. Antimicrob. Agents Chemother. 31(1987)780-783.
54. Rees, R. J. W. Animal models in leprosy. Br. Med. Bull. 44(1988)650-664.
55. Chin, N.-X. and Neu, H.-C. Ciprofloxacin, a quinolone carboxylic acid compound active against aerobic and anaerobic bacteria. Antimicrob. Agents Chemother. 25(1984)319-326.
56. Gay, J. D., De Young, D. R. and Roberts, G. D. In vitro activities of norfloxacin and ciprofloxacin against Mycobacterium tuberculosis, M. avium complex, M. chelonei, M. fortuitum and M. kansasii. Antimicrob. Agents Chemother. 26(1984)94-96.
57. Fenlon, C. H. and Cynamon, M. H. Comparative in vitro activities of ciprofloxacin and other 4-quinolones against Mycobacterium tuberculosis and Mycobacterium intracellulare. Antimicrob. Agents Chemother. 29(1986)386-388.
58. Tsukamura, M., Nakamura, E., Yoshii, S. and Amano, H. Therapeutic effect of a new antibacterial substance (DL 8280) on pulmonary tuberculosis. Am. Rev. Respir. Dis. 131(1985)352-356.
59. Yajko, D. M., Nassos, P. S. and Hadley, W. K. Therapeutic implications of inhibition versus killing of Mycobacterium avium complex by antimicrobial agents. Antimicrob. Agents Chemother. 31(1987)117-120.
60. Banerjee, D. K. Ciprofloxacin (4-quinolone) and Mycobacterium leprae. Lepr. Rev. 57(1986)159-162.
61. Guelpa-Lauras, C.-C, Perani, E. G., Giroir, A. M. and Grosset, J. H. Activities of pefloxacin and ciprofloxacin against M. leprae in the mouse. Int. J. Lepr. 55(1987)70-77.
62. Montay, G., Goueffon, Y. and Roquet, F. Absorption, distribution, metabolic fate and elimination of pefloxacin mesylate in mice, rats, dogs, monkeys and humans. Antimicrob. Agents Chemother. 25(1984)463-472.
63. Pattyn, S. R. Activity of ofloxacin and pefloxacin against M. leprae in mice. Antimicrob. Agents Chemother. 31(1987)671-672.
64. Saito, H., Tomioka, H. and Nagashima, K. In vitro and in vivo activities of ofloxacin against M. leprae infection induced in the mouse. Int. J. Lepr. 54(1986)560-562.
65. Tsukamura, M. In vitro antimycobacterial activity of a new antibacterial substance, DL 8280-differentiation between some species of mycobacteria and related organisms by the DL 8280 susceptibility test. Microbiol. Immunol. 27(1983)1129-1132.
66. Tsukamura, M. In vitro antituberculous activity of a new antibacterial substance, ofloxacin (DL 8280). Am. Rev. Respir. Dis. 131(1985)348-351.
67. Tsukamura, M., Nakamura, E., Yoshii, S., Yanase, M., Yasuda, Y. and Amano, H. [Therapeutic effect of ofloxacin (DL-8280) on pulmonary tuberculosis (Report of a one year-administration study on sixteen treatment-failure patients).] Kekkaku 60(1985)365-369.
68. Grosset, J. H., Guelpa-Lauras, C.-C, Perani, E. G. and Beoletto, C. Activity of ofloxacin against Mycobaclerium leprae in the mouse. Int. J. Lepr. 56(1988)259-264.
69. Grosset, J. H. Pharmacokinetics in drug screening.Int. J. Lepr. 55 Suppl.(1987)852-856.
70. N'Deli, L., Guelpa-Lauras, C.-C., Perani, E. G.and Grosset, J. H. Effectiveness of pefloxacin in the treatment of lepromatous leprosy. Int. J. Lepr. 58(1990)12-18.
71. Ito, K., Kohsaka, K. and Miyata, Y. Effect of ofloxacin on experimental leprosy. (Abstract) Int. J. Lepr. 55(1987)778.
72. Grosset, J. H., Guelpa-Lauras, C.-C., N'Deli, L.and Perani, E. Pefloxacin or ofloxacin in lepromatous leprosy at Adzope (Ivory Coast). II. Biological results.Abstract in Int. J. Lepr. 57 Suppl.(1989)316.
73. Uttley, A. H. C. and Collins, C. H. in vitro activityof ciprofloxacin in combination with other standardantituberculous drugs against Mycobacteriunz tuber-culosis. Tubercle 69(1988)193-195.
74. Rodloff, A. C. in vitro susceptibility test of non-tuberculous mycobacteria to sulphamethoxazole, tri-methoprim and combinations of both. Antimicrob.Agents Chemother. 9(1982)195-199.
75. Swenson, J. M., Thornsberry, C. and Silcox, V. A.Rapidly growing mycobacteria: testing of susceptibilityto antimicrobial agents. Antimicrob. Agents Chemo-ther. 22(1982)186-192.
76. Hummer, D., Pitlik, S. D., Block, C., Kaufman,L., Amit, S. and Rosenfield, J. B. Aquarium borneMycobacterium marinzon skin infection. Arch. Der-matol. 122(1986)698-703.
77. Shepard, C. C. Combinations of drugs against M. leprae studied in mice. Int. J. Lepr. 40(1972)33-39.
78. De Graw, J. I., Brown, V. H., Colwell, W. T. and Morrison, N. E. Potential antileprotic agents. III. Inhibition of mycobacterial dihydrofolate reductase by 2,4,-diamino-5-methyl-6-alkylquinazoline. J. Med. Chem. 17(1974)762-764.
79. Gelber, R. H. and Levy, L. The effect of dihydrofolate reductase inhibitors on M. leprae in the mouse footpad. Int. J. Lepr. 44(1976)124-132.
80. Gelber, R. H. and Levy, L. Further studies of dihydrofolate reductase inhibitor activity on the multiplication of M. leprae. Abstract in Int. J. Lepr. 46(1978)111-112.
81. Al-Rubeai, M. and Dale, J. W. Purification and characterization of dihydrofolate reductase from Mycobacterium phlei. Biochem. J. 235(1986)301-303.
82. Baker, D. J., Beddell, C. R., Champness, J. N., Goodford, P. J., Norrington, F. E., Smith, D. R. and Stammers, D. K. The binding of trimethoprim to bacterial dihydrofolate reductase. FEBS Lett. 126(1981)49-52.
83. Seydel, J. K., Rosenfeld, M., Sathish, M., Haller, R., Kansy, M. and Hachtel, G. Strategies in the development of new drugs and drug combinations against leprosy demonstrated on the example of folate-and gyrase-inhibitors. Abstract in Lepr. Rev. 57 Suppl.3(1986)23-24.
84. Hastings, R. C. and Jacobson, R. R. Activity of ansamycin against M. leprae in mice. (Letter) Lancet 2(1983)1079-1080.
85. Hastings, R. C, Jacobson, R. R. and Richard, V. R. Ansamycin activity against rifampicin rsesistant M. leprae. Lancet 1(1984)1130.
86. Heifets, L. B. and Iseman, M. D. Determination of in vitro susceptibility of mycobacteria to ansamycin. Am. Rev. Respir. Dis. 132(1985)710-711.
87. Ji, B.-H., Chen, J.-K., Lu, X.-H., Wang, S.-Y., Ni, G.-X., Hou, Y.-H., Zhou, D.-H. and Tang, Q.-K. Antimycobacterial activities of two newer ansamycins, R-76-1 and DL 473. Int. J. Lepr. 54(1986)563-577.
88. Pattyn, S. R. Rifabutin and rifapentine compared with rifampin against Mycobacterium leprae in mice. (Letter) Antimicrob. Agents Chemother. 31(1987)134.
89. Lin, Z.-M. [Antileprosy effect of RFD (R-77-3) in the mouse foot pad technique.] China Lepr. J. 3(1987)232-234.
90. Chen, L.-F. [Effects of treatment of multibacillary leprosy with RFD, B663 and DDS in a short term.]China Lepr. J. 3(1987) 211-212.
91. Prabhakaran, K., Harris, E. B., Sanchez, R. M. and Hastings, R. C. Beta-lactamase synthesis in Mycobacterium leprae. Microbios 49(1987)183-188.
92. Misiek, M., Moses, A. J., Pursiano, T. A., Leitner, F. and Price, K. E. In vitro activity of cephalosporins against Mycobacterium tuberculosis H37Rv: structure activity relationships. J. Antibiot. (Tokyo) 26(1973)737-744.
93. Sanders, W. E. Jr., Schneider, N., Hartwig, C, Cacciatore, R. and Valdez, H. Comparative activities of cephalosporins against mycobacteria. In: Current Chemotherapy and Infectious Diseases. Nelson, J. D. and Grassi, C, eds. Washington D.C.: American Society for Microbiology, 1980, pp. 1075-1077.
94. Heifets, L. B., Iseman, M. D., Cook, J. L., Lind-holm-Levy, P. J. and Drupa, I. Determination of in vitro susceptibility of Mycobacterium tuberculosis to cephalosporins by radiometric and conventional methods. Antimicrob. Agents Chemother. 27(1985)11-15.
95. Casal, M. J. and Rodriguez, F. C. In vitro suscep-tibility of Mycobacterium fortuitum and Mycobacterium chelonei to cefoxitin. Tubercle 63(1982)125—127.
96. Gaugas, J. M. Antimicrobial therapy of experimental human leprosy bacilli (M. leprae) infection in the mouse. Lepr. Rev. 38(1967)225-230.
97. Shepard, C. C, Walker, L. L., Van Landingham, R. M. and Redus, M. A. Kinetic testing of drugs against Mycobacterium leprae in mice; activity of cephaloridine, rifampin, streptovaricin, vadrine and viomycin. Am. J. Trop. Med. Hyg. 20(1971)616-620.
98. Shepard, C. C, Walker, L. L., Van Landingham, R. M. and Good, R. C. Activity of selected beta-lactam antibiotics against H., Mycobacterium leprae. Int. J. Lepr. 55(1987)322-327.
99. Kucers, A. and Bennett, N. M. The Use of Antibiotics: A Comprehensive Review with Clinical Emphasis. 3rd ed. Philadelphia: J. B. Lippincott, 1979.
100. Loria, P. R. Minocycline hydrochloride treatment for atypical acid-fast infection. Arch. Dermatol. 112(1976)517-519.
101. Tsukamura, M. In-vitro antimycobacterial activity of minocyline. Tubercle 61(1980)37-38.
102. Gelber, R. Activity of minocyline in .11. leprae-infected mice. J. Infect. Dis. 156(1987)236-239.
103. MacDonald, H., Kelly, R. G., Allen, E. S., Noble, J. F. and Kanegis, L. A. Pharmacokinetic studies onminocyline in man. Clin. Pharmacol. Titer. 14(1973)852-861.
104. Fair, W. R. Diffusion of minocyline into prostaticsecretion in dogs. Urology 3 (1974) 339-344.
105. Allen, J. C. Minocyline. Ann. Intern. Med. 85(1976)482-487.
106. Faget, G. H. A. and Erickson, P. T. Use of streptomycin in the treatment of leprosy; a preliminary report. Int. J. Lepr. 15(1947)146-153.
107. Driesbach, J. and Cochrane, R. G. A study of the effect of streptohydrazid on lepromatous leprosy over a period of about three years. Lepr. Rev. 29(1958)136-142.
108. Gelber, R. and Gibson, J. The killing potential of various aminoglycoside antibiotics for M. leprae. (Abstract) Int. J. Lepr. 47(1979)684-685.
109. Gelber, R. H., Henika, P. R. and Gibson, J. B. The bactericidal activity of various aminoglycoside antibiotics against M. leprae in mice. Lepr. Rev. 55(1984)341-347.
110. Gangadharam, P. R. J., Perumal, V. K., Podapati, N. R., Kesavalu, L. and Iseman, M. D. In vivo activity of amikacin alone or in combination with clofazimine or rifabutin or both against acute experimental Mycobacterium avium complex infections in beige mice. Antimicrob. Agents Chemother. 32(1988)1400-1403.
111. Gelber, R. II. Further studies of the killing of M. leprae by aminoglycosides: reduced dosage and frequency of administration. Int. J. Lepr. 55(1987)78-82.
112. Mester, L., Szabados, L.. Mester, M. and Yadav. N. Maillard type carbamyl-amine reactions in vivo and their physiological effects. In: Progress in Food and Nutrition Science. Vol. 4. New York: Pergamon Press. 1981.
113. Jayaraman, P., Mahadevan, P. R., Mester, M. and Mester, L. Inhibition of the incorporation of [3H]DOPA in Mycobacterium leprae by deoxyfructoserotonin. Biochem. Pharmacol. 29(1980)2526-2528.
114. Mester, L. and Balakrishanan, S. DFS: first human metabolite with anti-leprosy activity. Acta Leprol. (Genève) 83(1981)21-23.
115. Ambrose, E. J., Antia, N. H. and Tannaz, J. B. The action of deoxyfructoserotonin on intracellular bacilli and on host response in lepromatous leprosy. Lepr. Rev. 56(1985)199-208.
116. Saint-André, P., Baquillon, G., Mester, L. and Mester, M. Bilan de neuf mois de traitement par la désoxyfructo-scrotonine des lépreux lépromateux. Acta Leprol. (Genève) 86-87(1982)189-197.
117. Antia, N. IL, Ambrose, E. J., Uplekcr, M. W., Mester, L. and Mahadevan, P. R. Elfect of deoxyfructoserotonin (DFS) on lepromatous leprosy. Lancet 1(1988)619-622.
118. Klebanoff, S. J. and Shepard, C. C. Toxic effect of the peroxidase-hydrogen peroxide-halide antimicrobial system on M. leprae. Infect. Immun. 44(1984)534-536.
119. Van Rensburg, C. E. J., Gatner, E. M. S., Imkamp, F. M. J. H. and Anderson, R. Effects of clofazimine alone or combined with dapsone on neutrophil and lymphocyte functions in normal individuals and patients with lepromatous leprosy. Antimicrob. Agents Chemother. 21(1982)693-697.
120. Zeis, B. M. and Anderson, R. Clofazimine-mediated stimulation of prostaglandin synthesis and free radical production as novel mechanisms of drug-induced immunosuppression. Int. J. Immunopharmacol. 8(1986)731-739.
121. Mittal, A., Seshadri, S. P., Conalty, M. L., O'Sullivan, J. F. and Nath, I. Rapid, radiometric in vitro assay for the evaluation of the anti-leprosy activity of clofazimine and its analogues. Lepr. Rev. 56 (1985)99-108.
122. Zeis, B. M., Anderson, R. and O'Sullivan, J. F. The effect of ten phenazine-derivatives in comparison to clofazimine on the production of prostaglandin E2 by polymorphonuclear leucocytes. Lepr. Rev. 58(1987)383-388.
123. O'Sullivan, J. F., Connelly, M. L. and Morrison, N. E. Clofazimine analogues active against a clofazimine-resistant organism. J. Med. Chem. 31(1988)567-572.
124. Franzblau, S. G. and O'Sullivan, J. F. Structure-activity relationships of selected phenazines against Mycobacterium leprae in vitro. Antimicrob. Agents Chemother. 32(1988)1583-1585.
125. Schaper, K.-J., Seydel, J. K., Rosenfeld, M. and Kazda, J. Development of inhibitors of mycobacterial ribonucleotide reductase. Lepr. Rev. 57 Suppl.3(1986)254-264.
126. Shepard, C. C, Tolentino, J. G. and McRae, D. H. The therapeutic effect of 4,4' diacetyl diaminodiphenyl sulfone (DADDS) in leprosy. Am. J. Trop. Med. Hyg. 17(1968)192-201.
127. Shepard, C. C, Levy, L. and Fasal, P. The death rate of M. leprae during treatment of lepromatous leprosy with acedapsone (DADDS). Am. J. Trop. Med. Hyg. 21(1970)440-445.
128. Modderman, E. S. M., Merkus, F. W. H. M., Zuidema, J., Huikeshoven, H. and Leiker, D. L. Sex differences in the absorption of dapsone after intramuscular injection. Int. J. Lepr. 51(1983)359-365.
129. Cockshott, W. P., Thompson, G. T., Howlett, L. J. and Sceley, E. T. Intramuscular or intralipomatous injections? N. Engl. J. Med. 307(1982)356-358.
130. Pieters, F. A. J. M., Zuidema, J. and Merkus, F. W. H. M. Sustained release properties of an intra-adiposely administered dapsone depot injection. Int. J. Lepr. 54(1986)383-388.
131. Levy, L. and Shepard, C. C. The number of M. leprae in the pre-treatment biopsy specimen does not determine the rate of response of patients with lepromatous leprosy to chemotherapy with acedapsone. Lepr. Rev. 57(1986)27-31.
132. Yang, T.-T. and Swarbrick, J. Sustained-release delivery systems, I: Phase diagram studies of dapsone and selected derivatives. J. Pharm. Sci. 75(1986)53-56.
133. Zuidema, J., Modderman, E. S. M., Merkus, F. W. H. M. and Hilbers, H. W. The intramuscular injection of monoacetyldapsone. In: Proceedings of the 2nd International Congress on Biopharmaceutics and Pharmacokinetics. Part 1. Aiache, J. M. and Hirtz, J., eds. Paris: Lavoisier, 1984, pp. 240-249.
134. Pieters. F. A. J. M. and Zuidema. J. Intra-adipose administration of monoacetyldapsone to healthy volunteers. Int. J. Lepr. 54(1986)510-516.
135. Pieters, F. A. J. M., Woonink, F. and Zuidema, J. A field trial among leprosy patients in Nigeria with depot injections of dapsone and monoacetyldapsone. Int. J. Lepr. 56(1988)10-20.
136. Molaui, A. and Weinstein, L. In vitro activity of erythromycin against atypical mycobacteria. J. Infect. Dis. 123(1971)216-219.
137. Franzblau, S. G. and Hastings, R. C. Rapid in vitro metabolic screen for antileprosy compounds. Antimicrob. Agents Chemother. 31(1987)780-783.
138. Franzblau, S. G. Oxidation of palmitic acid by Mycobacterium leprae in an axenic medium. J. Clin. Microbiol. 26(1988)1124-1129.
139. Harris, E. B., Franzblau, S. G. and Hastings, R. C. Inhibition of phenolic glycolipid-I synthesis in extracellular Mycobacterium leprae as an indicator of antimicrobial activity. Int. J. Lepr. 57(1989)588-591.
140. Franzblau, S. G. and Hastings, R. C. In vitro and in vivo activities of macrolides against Mycobacterium leprae. Antimicrob. Agents Chemother. 32(1988)1758-1762.
* This review, written in 1988 by Richard J. Baker, a medical student in London, was a prize-winning essay in the annual competition sponsored by the British Leprosy Relief Association (LEPRA) for essays on various aspects of leprosy. We take pleasure in publishing this review. Mr. Baker's present address is 4C Goulton Road, Hackney, London E5 8HA. England.