- Volume 57 , Number 2
- Page: 472–5
Leprosy in infants-report of two cases
ABSTRACT
Two infants, one 4 months old and the other 2 months old, having histologically confirmed indeterminate leprosy are reported. The route of infection, mode of transmission, and incubation period are discussed with reference to these two cases of infantile leprosy.RÉSUMÉ
On rapporte ici le cas de deux enfants, l'un âgé de 4 mois et l'autre de 2 mois, qui présentaient des lésions histologiquement confirmées de lèpre indéterminée. La voie d'infection, le mode de transmission, et la période d'incubation sont discutés à la lumière de ces deux cas de lèpre infantile.RESUMEN
Se reportan 2 infantes, uno de 4 meses de edad y el otro de 2 meses de edad, con lepra indeterminada confirmada histológicamente. La ruta de infección, el modo de transmisión, y el periodo de incubación, se discuten en referencia a estos dos casos infantiles de lepra.The occurrence of leprosy during infancy is uncommon. Two infants who had the disease are reported.
CASE REPORTS
Case 1. A 4-month-old female was brought to the clinic on 3 April 1986 with two pale lesions on the left back. These lesions had been noticed about a month before and, according to the mother, there had been some increase in the size of the lesions during this period. The mother was examined and no evidence ofleprosy was found. There was no history ofleprosy in the father or the siblings. However, one of the paternal uncles, staying in the same house, was suffering from active borderline tuberculoid (BT) leprosy. He was smear negative and had been taking treatment from our clinic for the last 4 months. It was on his suggestion that the baby was brought for check up.
On examination there were two small (about 3 cm), ill-defined, hypopigmented macules over the left back near the buttocks (Fig. 1). The skin of the lesions appeared normal, there being no infiltration, warmth or decreased sweating. The infant was suspected of having indeterminate leprosy. Skin smears from one car and one lesion were both negative for acid-fast bacilli (AFB). The lepromin reaction to Dharmendra antigen was also negative. Biopsy of the skin lesion revealed indeterminate histology. There was a mild mononuclear infiltrate in a dermal nerve and a small clump of AFB was seen in the nerve (Fig. 2). The child was put on dapsone (DDS) 5 mg a day, and during the next 6 months, the lesions completely healed.

Fig. 1. Back of case 1, showing two lesions.
Fig. 2. Histological section showing nerve alfection and bacilli ( ) (Fite-Faraco x 1000).
) (Fite-Faraco x 1000).
Case 2. On 2 June 1986 a female aged 2 months presented with a small lesion on the abdomen in the left iliac fossa region. The lesion had been noticed by the mother about a week earlier, had remained unchanged during this period, and had not been tender. No treatment had so far been taken. The mother of the child was an old case of BT leprosy (skin-smear negative) and had been on multidrug therapy (MDT) for paucibacillary leprosy for the last 9 months. She had been declared "disease inactive" 4 months earlier. No one else in the family had leprosy.
The infant had a single, coin-sized, mildly erythematous and slightly raised lesion with indistinct borders and a smooth surface in the left iliac region (Fig. 3). The pin-prick response was appreciably diminished over the lesion; elsewhere it was brisk. There was no peripheral nerve thickening. BT leprosy was suspected. A skin smear from the lesion was negative for AFB. A skin biopsy of the lesion revealed that the dermal nerves were infiltrated with round cells, but there was no granuloma as such. Fite-Faraco staining showed a few AFB in the nerve fiber, confirming the diagnosis ofleprosy (Fig. 4). The infant's blood and urine samples were collected for a phenolic glycolipid (PGL) antibody assay. The serum showed the presence of PGL-IgM antibodies, and PGL antibodies were also detected in the urine. The infant was put on 50 mg of rifampin monthly and 5 mg of DDS daily. During the next 3 months, the erythema disappeared and the lesion became flat. The treatment was continued for another 3 months.
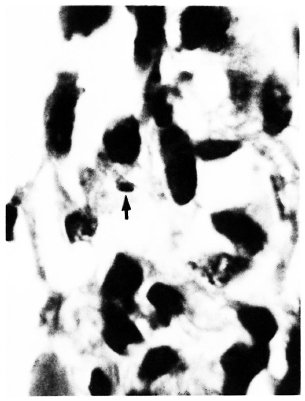
Fig. 3. Lesion in case 2 on left side of abdomen.

Fig. 4. A small clump of bacilli ( ) within the dermal nerve (Fite-Faraco x 1000).
) within the dermal nerve (Fite-Faraco x 1000).
DISCUSSION
In recent years, there has been a lot of interest in childhood leprosy, especially the disease affecting infants (2-4,8,9). A recent detailed review of this subject (1) indicates that leprosy in infancy is not as uncommon as hitherto believed, there being about 50 such recorded and 20 proved cases. It may be assumed that the real number is greater than this. We ourselves have come across six cases of leprosy in infancy. Of these, three (including the present ones) were proven cases of the disease in infancy.
Both of these infants, like the one reported earlier (4), undoubtedly had leprosy as confirmed histologically. In both instances, a skin biopsy showed indeterminate disease with nerve infiltration as well as AFB in the nerves. Additionally, in the second case, even though the infant was only 2 months old, specific anti-PGL IgM antibodies were detected in both serum and urine. These laboratory findings also support the clinical diagnosis of leprosy. The occurrence of leprosy in these two infants at such a early age raises important issues regarding the source of the infection, the route or mode of infection, and the incubation period.
Since the mother of case 1 did not suffer from leprosy and the mother of the second infant had smear-negative BT disease, the source of infection and the mode of transmission are not easily explained. In case 2, it is possible that at some stage the mother had a state of bacillemia and that the organisms had crossed the placenta to infect the fetus. Significant bacillemia in a proportion of nonlepromatous cases has been well documented (10), and intact Mycobacterium leprae have been demonstrated in the placenta and cord blood (6,11). Rising titers of specific IgA and IgM antibodies have also been demonstrated in the immediate postnatal period (first 3 months) in infants born to lepromatous mothers (2,7). These suggest that the fetus of a leprous mother is at risk of in utero infection or at least exposure to M. leprae antigens. Although this possibility of transplacental infection remains, it appears unlikely, since even the mother in case 2 was smear negative.
It is also possible that these infants acquired the infection postnatally through an intrafamilial household contact, and a rapid multiplication of the organisms resulted in the disease. Likewise, the possibility of an extrafamilial case infecting the infants soon after birth cannot be ruled out, although under the customary conditions in this part of India, this is unlikely.
The route of infection and mode of transmission are equally difficult to explain in both cases since no contact with a skin-smear positive leprosy case was known. In fact, the mother of the second infant had "inactive" disease during the late months of gestation. It is possible that in both these infants local inoculation was the mode of infection. However, infection through the nasal mucosa cannot be ruled out.
It has generally been considered that the incubation period of leprosy is very prolonged and could range from 2 to 20 years. This has been attributed to the slow multiplication of M. leprae as is evidenced by the growth curves in mice (9). In the two cases reported here, the incubation period could not have been more than a few months. Such a short incubation period can be explained by the possibility of a massive infection or by a more rapid multiplication of M. leprae than usual based on a higher proportion of viable organisms, a possibility recently suggested by Hastings and Morales (5). Massive infection does not seem probable in these infants since their probable source cases, an uncle in one and the mother in the other, were both smear-negative BT patients. It appears more likely that the short incubation period could have been due to a more rapid multiplication of M. leprae than usual in highly susceptible hosts such as these infants.
In conclusion, these two cases show that clinical leprosy can manifest at a very young age. Further, when there is an index case in the family, suspicious-looking lesions in infants and children should be looked for and, where necessary, a biopsy should be taken to rule out leprosy.
Acknowledgments. We express our profound gratitude to Dr. H. Srinivasan for critically reviewing the manuscript and for his valuable comments. We are particularly grateful to Dr. K. V. Desikan and Dr. C. J. G. Chacko for having con firmed the histological findings and Dr. U. Sengupta for doing the PGL antibody assays. We thank Mr. Shclandra Kulshrestha for secretarial assistance and Mr. Hari Om Agrawal for the photography.
REFERENCES
1. BRUBAKER. M. L., MEYERS, W. M. and BOURLAND, J. Leprosy in children one year of age and under. Int. J. Lepr. 53(1985)517-523.
2. DUNCAN, M. E., MELSOM, R., PEARSON, J. M. H., MENZEL, S. and BARNETSON, R. ST.C. A clinical and immunological study of four babies of mothers with lepromatous leprosy, two of whom developed leprosy in infancy. Int. J. Lepr. 51(1983)7-17.
3. GANAPATI, R. R., NAIK, S. S. and PANDYA, S. S. Child-hood leprosy-study of prevalence rates and clinical aspects through surveys in Bombay. Lepr. India 48 Suppl.(1976)645-660.
4. GIRDHAR, B. K., GIRDIIAR, A., RAMU, G. and DESIKAN, K. V. Borderline leprosy (BL) in an infant-report of a case and a brief review. Lepr. India 55(1983)333-337.
5. HASTINGS, R. C. and MORALES, M. J. Observations, calculations and speculations on the growth and death of M. leprae in vivo. Int. J. Lepr. 50(1982)579-582.
6. INABA, T. Über die Histopathologischen and Bakteriologischen Untersuchungen der Pla/enta bei Leprösen. Abstract in Lepro 9 (1938) 111 (quoted from Brubaker, et al. Leprosy in children one year of age and under. Int. J. Lepr. 53(1985)517-523).
7. MELSOM, R., HARHOE, M. and DUNCAN M. E. IgA. IgM and IgG anti-M. leprae antibodies in babies of leprosy mothers during the first two years of life. Clin. Exp. Immunol. 49(1982)532-542.
8. REVANKAR, C. R., DEWARKER, P. R., SINGH, M. and GANAPATI, R. Leprosy in preschool age. Lepr. Rev. 50(1979)293-296.
9. SHEPARD, C. C. Multiplication of Mycobacterium leprae in the foot-pads of the mouse. Int. J. Lepr. 30(1962)291-306.
10. SREEVATSA, SENGUPTA, U., RAMU, G. and DESIKAN. K. V. Evaluation of bacteraemia in leprosy patients. Lepr. India 50(1978)381-387.
11. VALLA, M. C. Lèpre et grossesse. Thèse de médecine, Lyon, France, 1976 (quoted from Brubaker. et al. Leprosy in children one year of age and under. Int. J. Lepr. 53(1985)517-523).
1. M.B.B.S.; Central JALMA Institute for Leprosy, Taj Ganj, Agra 282001. India.
2. M.D.; Central JALMA Institute for Leprosy, Taj Ganj, Agra 282001. India.
3. M.D.; Central JALMA Institute for Leprosy, Taj Ganj, Agra 282001. India.
4. M.B.B.S.; Central JALMA Institute for Leprosy, Taj Ganj, Agra 282001. India.
5. M.S.; Central JALMA Institute for Leprosy, Taj Ganj, Agra 282001. India.
6. M.D., Central JALMA Institute for Leprosy, Taj Ganj, Agra 282001. India.
Reprint requests to Dr. B. K. Girdhar, Central JALMA Institute for Leprosy, P.O. Box 31, Taj Ganj, Agra 282001, U.P., India.
Received for publication on 19 August 1988.
Accepted for publication in revised form on 22 December 1988.