- Volume 57 , Number 2
- Page: 499–505
Hepatic Morphology in Reactional States of Leprosy
ABSTRACT
Liver function tests and liver biopsies were studied in 23 leprosy patients in reaction and 10 without reaction. The liver biopsies in leprosy patients with reaction showed exudative lesions, epithelioid and tuberculoid granulomas, and foam-cell granulomas. Portal vasculitis was encountered in a few cases. Neutrophilic infiltration into the foam-Cell granulomas was seen in a few cases of lepromatous (LL) leprosy with reaction. In six cases ofbordeline (BL, BB and BT) leprosy with reaction, a spectrum of lesions bearing footprints of exudative lesions were seen evolving into epithelioid-cell granulomas. Foam-cell granulomas and tuberculoid and epithelioid granulomas along with exudative lesions were encountered in two cases on individual biopsy strips. An altered albumin-to-globulin ratio was the chief functional derangement observed in these cases. The spectrum of changes observed in borderline leprosy with reaction could be discrete steps in the evolution of upgrading reaction.RÉSUMÉ
Chez 23 malades de la lèpre en réaction, et chez 10 malades sans réaction, on a procédé à des épreuves de la fonction hépatique et pratiqué des biopsies du foie. Les biopsies de foie provenant de malades de la lèpre souffrant de réaction, ont montré des lésions exsudatives, des granulomes épithélioïdes et tuberculoïdes, et des granulomes à cellules spumeuses. Une vasculitc portale a été notée chez un petit nombre de cas. Dans quelques cas de lèpre lépromateuse (LL) avec réaction, on a relevé une infiltration neutrophilique dans les granulomes à cellules spumeuses. Dans 6 cas de lèpre dimorphe (BL, BB et HT), on a vu évoluer au niveau des granulomes à cellules épithélioïdes toute une gamme de lésions présentant les caractéristiques de lésions exsudatives. Dans deux biopsies individuelles, on a mis en évidence des granulomes à cellules spumeuses, ainsi que des granulomes tuberculoïdes et épithélioïdes, coexistant avec des lésions exsudatives. La principale anomalie fonctionnelle notée dans ces cas consistait en une altération du rapport albumine/globuline. La gamme des modifications observées dans la lèpre dimorphe avec réactions peut correspondre à des étapes discrètes dans l'évolution de la réaction "upgrading."RESUMEN
Se hizo un estudio de la función y de la alteración hepática en 23 pacientes con lepra en reacción y en 10 pacientes sin reacción. Las biopsias de hígado de los pacientes con lepra rcaccional mostraron lesiones exudativas, granulomas epitelioides y tuberculoides, y granulomas espumosos. En algunos casos se encontró vasculitis portal. En pocos casos se observó infiltración neulrofílica en los granulomas de células espumosas de los pacientes lepromatosos en reacción. En 6 casos de lepra intermedia (BL. BB y BT) reaccional, se observaron lesiones de tipo exudativo evolucionando a granulomas de células epitelioides. En 2 biopsias se encontraron secciones individuales con granulomas de células espumosas y granulomas de células epitelioides, junto con lesiones exudativas. En estos casos, la anormalidad funcional prominente fue una alteración en la relación albúminaiglobulina. El espectro de los cambios observados en la lepra intermedia en reacción, podría representar los pasos discretos en la evolución hacia una reacción con mejoría.Reports on the pathomorphology of the liver in leprosy have been few and far between. The available studies mostly relate to the nature of involvement of the liver in nonreactional leprosy (3,4,10,12,16,17). In some of these studies, however, a few cases of leprosy with reaction are mentioned (4,12). Kramarsky, et al. (11) have reported one case of erythema nodosum leprosum whose liver biopsy was studied in detail in the perspective of hepatic morphological changes in reaction. In keeping with the rapid advances in the field of immunology, our understanding of certain aspects of leprosy, particularly of the reactional states, has improved, in light of which the morphological changes stand to be interpreted better. All this and the paucity of studies on the liver in leprosy reactions prompted us to undertake the present study to find out the histomorphological changes in the liver in reactional states of leprosy.
MATERIALS AND METHODS
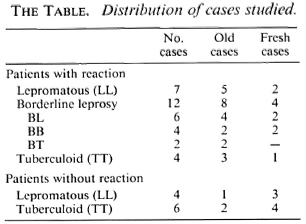
During 1985-1987, we studied liver function tests and liver biopsies of 33 leprosy patients attending the Leprology Clinic of Ispat General Hospital, Rourkcla, Orissa, India. All of the patients were known cases of leprosy, either already taking treatment from our clinic (from a minimum of 6 months to a maximum of 15 years) or were freshly diagnosed cases scheduled to be put on treatment. The cases were classified according to the criteria of Ridley and Jopling 5). However, because the cases in the "bordeline spectrum" are immunologically unstable and tend to move in cither direction, for convenience the borderline lepromatous (BL), borderline borderline (BB), and borderline tuberculoid (BT) cases have been grouped under borderline leprosy in keeping with Jopling (9). The cases considered for the study were both with and without reaction, who consented to undergo the investigation and liver biopsy after the purpose and risks of the procedure were explained to them. Reactions were not classified histologically in order to avoid a preconceived bias on the type of histological changes that were expected to be encountered on the liver biopsies. Although we were mainly concerned to study cases of leprosy with reaction, a few cases without reaction were also included in order to form a basis for the study of hepatic histomorphology. The distribution of the cases is summarized in The Table. Tuberculosis-the other common granulomatous disease in this region-was excluded in all the cases by relevant investigations. The age range of the patients was from 10 to 69 years with a median of 39 years. There were 27 male and six female patients.
The patients were admitted at least for a day into the wards for the investigations. Five ml of heparinized blood was collected for biochemical tests of liver function. From the plasma total and conjugated bilirubin, alanine aminotransferase, alkaline phosphatase, γ-glutamyl transpeptidase, total protein and albumin were estimated on an Hitachi-705 autoanalyzer. Liver biopsies were performed using the Menghini aspiration needle as per standard procedure. The following staining procedures were used for all the cases on formal saline fixed-tissue sections: hematoxylin and eosin, Gordon and Sweet's reticulin, alkaline Congo red for amyloid, Fite's method for leprosy bacilli (6), Chromotrope-2R for protcinaccous deposits, and phosphotungstic acid-hematoxylin (PTAH) for the demonstration of fibrin.
RESULTS
The histomorphological changes observed in the different groups are summarized below.
Lepromatous (LL) with reaction. In the seven biopsies studied in this group, two important types of lesions were encountered. One lesion was fundamentally an exudative type in the sinusoids and portal vessels and was seen in four cases. In these, there were foci of sinusoidal neutrophilic infiltration (Fig. 1), and well-circumscribed sinusoidal exudative lesions of variable sizes containing an inflammatory exudate composed of neutrophils, lymphocytes, an occasional eosinophil, and fibrin (Fig. 2). Portal vasculitis, predominantly a lymphocytic infiltration of the portal vessel wall, along with a few neutrophils was seen in two of these cases (Fig. 3). One of them had foam-cell granulomas in addition to the exudative lesions. The second type of lesion, seen in two cases, showed neutrophilic infiltration into foam-cell granulomas. Thus, the confluent granulomas appeared disrupted. One case showed only fibrin deposits along the sinusoidal wall.

Fig. 1. Focus of sinusoidal inflammatory infiltration (H&E x400).
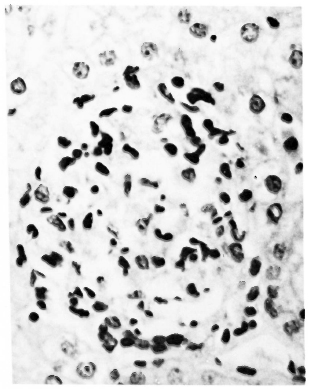
Fig. 2. A well-developed and circumscribed large sinusoidal exudative lesion. A varicty of inflammatory cells and fibrin are seen (H&E x 400).
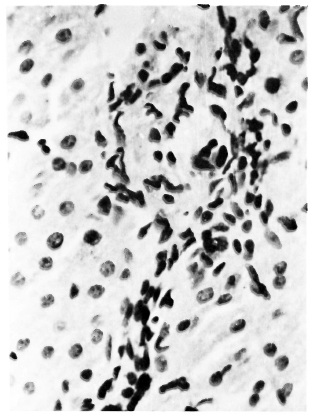
Fig. 3. Portal vasculitis. Note inflammatory infiltration, gross edema, and fibrinous exudation around the vessel. Course of the vessel is seen at the bottom (H&E x400).
Borderline leprosy with reaction. Twelve cases were studied in this group. In one case there was no appreciable histological change, and only fatty changes of the liver were seen in another case. The histological findings noted in the remaining ten cases are as follows. Six cases showed a spectrum of sinusoidal exudative lesions but not portal vasulitis. Some of these changes were as described above under sinusoidal exudative lesions. Some of these lesions were quite large and distended the sinusoids with inflammatory cells and fibrin. In addition to this, in some of these lesions macrophages were seen in the inflammatory infiltrate (Fig. 4). In some others, epithelioid cells were observed in the centers of the lesions. The number of epithelioid cells was variable; in some lesions there were only a few (Fig. 5), in others this was the predominant cell type such that the lesion could be called an epithelioid-cell granuloma with only a few lymphocytes and neutrophils left as foot prints of their origin from exudative lesions (Fig. 6). It was observed that as the population of epithelioid cells increased, the number of inflammatory cells decreased. Thus, whereas the exudative lesion appeared loosely textured and edematous, the epithelioid-cell granuloma was compactly cellular and gave a solid appearance. In one epithelioid-cell granuloma coalescence of the epithelioid cells into a Langhans'-type giant cell was observed (Fig. 7). Along with these changes, foam-cell granulomas were seen in two of these cases. Only for the purpose of description we have used the terms epithelioid-cell granulomas for lesions composed of epithelioid cells and tuberculoid granuloma for lesions replete with Langhans' giant cells in addition to lymphocytes. Thus, among the remaining four biopsies in this group, foam-cell granulomas as encountered in lepromatous leprosy (3,17) were seen in two biopsies, one each along with epithelioid-cell granulomas and tuberculoid granulomas (Fig. 8). One biopsy showed foci of exudative lesions and tuberculoid granulomas but no intervening stages in the spectrum of changes described above. The last case in this group showed only tuberculoid granulomas and no other changes.
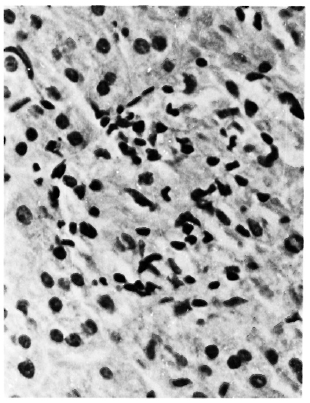
Fig. 4. Appearance of macrophages in sinusoidal exudative lesion. Note the lesion distends the sinusoid (H&E x 400).
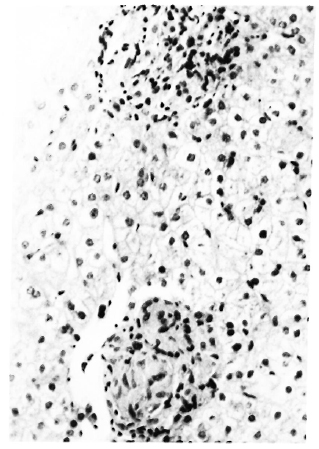
Fig. 5. Two well-delineated sinusoidal lesions. One on top is more of an exudative lesion; one on bottom looks solidly cellular composed of epithelioid cells (H&E x200).
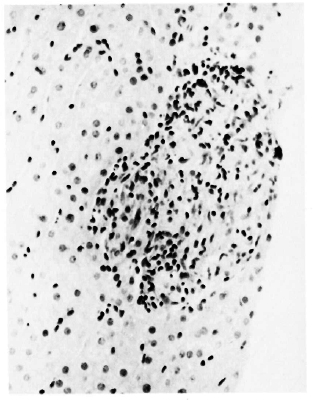
Fig. 6. A large, well-circumscribed epithelioid-cellgranuloma bearing scattered lymphocytes and neutrophils-footprints of its origin from an exudative lesion(H&E x 200).
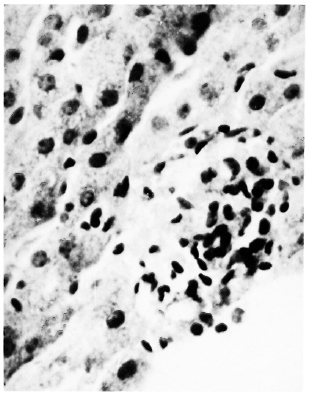
Fig. 7. A sinusoidal granuloma bound at the pe riphery by endothelial cells showing at the center co alescence of epithelioid cells into a Langhans'-type giant cell (H&E x 400).
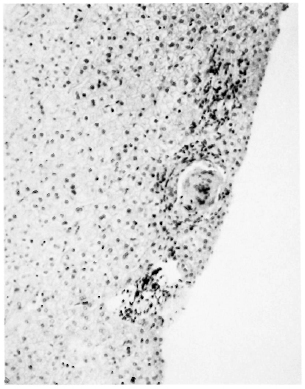
Fig. 8. Three granulomas in a row. From top to bottom: a developing epithelioid granuloma, a fully developed tuberculoid granuloma, and a small foam-cell granuloma (H&E x 100).
Tuberculoid (TT) with reaction. Of the four cases studied, one showed exudative lesions and two cases showed portal vasculitis. Two cases showed a large number of noncascating tuberculoid granulomas. In one biopsy an exudative lesion showed apoptotic cells instead of a neutrophilic exudate.
Lepromatous (LL) without reaction. Four LL cases were studied. One biopsy did not show any lesion, two cases showed foamcell granulomas, and the other case showed small foci of sinusoidal neutrophilic infiltration.
Tuberculoid (TT) without reaction. Six TT cases were studied. Three of them did not show any histological lesion in the biopsies, one case showed tuberculoid granulomas, and the remaining two cases revealed changes of alcoholic liver disease.
Other histological changes. Apart from the changes described, six patients from different groups showed mild-to-moderatc fatty changes in the liver. Four of them also showed diffuse focal hepatocytolysis. All'of them had a history of prolonged alcohol intake. Two other cases with a history of more than 7 years' antileprosy drug treatment showed diffuse focal hepatocytolysis.
No significant differences were observed in the lesions between the old and treated patients and the fresh cases.
Special stains. Fite's stain for lepra bacilli showed acid-fast bacilli (AFB), granules and globi in the foam-cell granulomas in Kupffcr cells and in the middle of some of the exudative lesions. Cases positive for AFB included: In the patients with reaction, 4 of the lepromatous (LL), 6 of the borderline (BL and BB), and 3 of the tuberculoid (TT) cases. In patients without reaction, all liver sections were negative for AFB, although nasal and skin serapings were positive in three cases. Only one lepromatous patient with reaction showed faint sinusoidal deposits of amyloid. The other cases were negative for Congo red. The reticulin framework was not disturbed. Only the foci of tuberculoid granulomas appeared well delineated without any necrosis. The proteinaccous and fibrinoid nature of the material in the exudative lesions was confirmed by Chromotrope-2R and PTAH staining.
Biochemical changes. The predominant biochemical change observed was the alteration of albumin-to-globulin ratio in 16 patients, 15 of whom were in reaction. Twelve of these cases in reaction had a globulin level of 4 g/dl or more. Albumin levels of < 3 g/dl were detected in four patients, all of them chronic alcoholics with histological evidence of alcoholic liver disease. One patient showed a mild elevation of alanine aminotransferase and a moderate increase of γ-glutamyl transpeptidase. Her liver biopsy showed focal hcpatocytolysis with lymphocytic infiltration.
DISCUSSION
Inflammatory exudative-type lesions are documented in skin biopsies in reactional states of leprosy (8,11,18). The full range of acute exudative-type changes was seen in the liver biopsies of our cases with reaction. Exudative lesions of the type observed by us have been reported by Kramarsky, et al. (11) in a lone case of erythema nodosum leprosum (ENL). However, because of the number of cases in this study, many lesions in different stages of evolution were captured on the same strip of liver tissue. This enabled us to study the nature of the progression of the lesions.
The exudative lesions encountered in our cases were in the form of sinusoidal and portal vasculitis and also as neutrophilic infiltrate into foam-cell granulomas. Exudative lesions in reactional states in the skin have been shown to be mediated by immune complexes (5,18). There is evidence of circulating immune complexes in lepromatous leprosy (13), and the lesions in the kidney in ENL are also believed to be immune-complex mediated (2). This apart, complexes also form on the cell surfaces with bacterial antigens present there (5). In light of this, we believe that the exudative lesions documented in our cases are possibly immune-complex mediated, and the neutrophilic infiltrate into foam-cell granulomas could be a reaction to cell-surface complexes.
One interesting aspect has been the development of epithelioid-cell granulomas from some of the exudative lesions. Leprosy bacilli have been shown in the endothelial cells of dermal vessels and vessel walls, and living, dead and disintegrated bacilli enter the circulation during reactional states (7,11). In some of the exudative lesions in our eases, AFB and granules were seen enmeshed in the exudative lesions which evidently might have come from the circulation. There is evidence of decreased fibrinolysis in these cases (14 ) which could promote the formation of thrombi and aid in the entanglement of bacilli. It is possible that the presence of these bacteria and their antigens evoked a granulomatous reaction. Thus, a spectrum of lesions evolving into epithelioid-cell granulomas were encountered. This could be interpreted as an upgrading reaction, more so because these were seen only in the group of borderline leprosy patients with reaction. Whether tuberculoid granulomas seen in this group evolved from the epithelioid-cell granulomas or started cle novo is difficult to say, because these are free of any evidence as to their origin. Nevertheless, the simultaneous presence of foam-cell, epithelioid, and tuberculoid granulomas on the same strip of liver biopsy in one of the patients supports the possibility of an upgrading reaction.
In tuberculoid (TT) leprosy with reaction only small foci of vasculitis were encountered. The chief tissue reaction was the formation of a large number of tuberculoid granulomas. Worthwhile inference cannot be drawn from the one focus of apoptosis seen in one case.
Our observations on the liver biopsies in lepromatous (LL) and tuberculoid (TT) cases without reaction have been basically no different than those already reported in the literature (3,4,10,12,16,17). Exudative lesions in one of the lepromatous (LL) patients and portal vasculitis in one of the tuberculoid (TT) cases perhaps represent subclinical complex-mediated injuries.
The chief biochemical finding of elevated gamma globulin was expected (1) but the low albumin levels found were in the cases of chronic alcoholics with evidence of alcoholic liver disease. This may not be related to the state of leprosy. The definite biochemical evidence of hepatitis encountered in one case could be a reaction to prolonged drug intake.
The hepatic lesions encountered in reaction were basically identical to those reported in skin biopsies in such cases. However, the spectrum of changes from exudative lesions through epithelioid granulomas to tuberculoid granulomas in reactional states ofbordeline leprosy could possibly be the discrete steps of the evolution of an upgrading reaction.
REFERENCES
1. BALAKRISHNAN, S. Blood chemistry in acute exacerbation in leprosy. Lepr. India 37(1965)247-251.
2. CHUGH, K. S., KAUR. S., KUMAR, B., NATH, I., DAMLE, P. B., SHARMA, B. K., SAKHUJA. V. and DATTA, B. N. Renal lesions in leprosy amongst North Indian patients. Postgrad. Med. J. 59(1983)707-711.
3. CONTRERAS, F., JR., TERENCIO DE LAS AGUAS, J. and CONTRERAS. F. Hepatic lesions in lepromatous patients. Int. J. Lepr. 37(1969)270-279.
4. COOK, G. C. and CORACUAN, M. Hepatic structure and function in Papua New Guineans with leprosy. Trans. R. Soc. Trop. Med. Hyg. 76(1982)721-727.
5. DHARMENDRA and DESIKAN, K. V. Mechanism of reactions. In: Leprosy. Dharmendra, ed. Bombay: Samant and Co., 1985. vol. 2, p. 988.
6. FITE, G. L., CAMBRE, P. J. and TURNER, M. H. Procedure for demonstrating lepra bacilli in paraflïn sections. Arch. Path. (Chicago) 43( 1947)624-625.
7. JOB, C. K. and DHARMENDRA. Histopathology of reacting skin lesions in leprosy. In: Leprosy. Dharmendra, ed., Bombay: Samant and Co., 1985, vol. 2, p. 823.
8. JOB. C. K., GUDE. S. and MACADEN, V. P. Erythema nodosum leprosum; a clinico-pathological study. Int. J. Lepr. 32(1964)177-184.
9. JOPLING, W. H. Handbook of leprosy. London: William Heinemann Medical Books Ltd., 1984, 3rd ed., p. 37.
10. KORANNE, R. V., SINGH, R. and IYENGAR, B. Liver involvement in tuberculoid leprosy. Indian J. Dermatol. 23(1978)21-25.
11. KRAMARSKY, B., EDMONDSON, H. A., PETERS, R. L. and REYNOLDS. T. B. Lepromatous leprosy in reaction. A study of the liver and skin lesions. Arch. Path. (Chicago) 85(1968)516-531.
12. KUMAR. B., SINGH, S. and KAUR, S. Jaundice occurring as a complication of erythema nodosum leprosum (a report of two cases). Lepr. India 52(1980)586-590.
13. MORAN, C. J., RYDER, G., TURK, J. L. and WATERS, M. R. F. Evidence for circulating immune complexes in lepromatous leprosy. Lancet 2(1972)572-573.
14. RAMU, G. and BALAKRISHNAN, S. Plasma fibrinogen levels and fibrinolytic activity in lepromatous leprosy. J. Assoc. Physicians India 25(1977)133-138.
15. RIDLEY. D. S. and JOPLING, W. H. Classification of leprosy according to immunity; a five-group system. Int. J. Lepr. 34(1966)255-273.
16. ROBINS, K., LEENA DEVI, K. R., VIJAYKUMAR, T. and GOPINATH, T. Liver in leprosy. II. Histopathological changes. Lepr. India 53(1981)600-607.
17. VERGHESE, A. and JOB, C. K. Correlation of liver function with the pathology of the liver in leprosy. Int. J. Lepr. 33(1965)343-348.
18. WATERS, M. F. R., TURK. J. L. and WEMAMBU, S. N. C. Mechanisms of reactions in leprosy. Int. J. Lepr. 39(1971)417-428.
1. M.D., Senior Specialist, Pathology; Ispat General Hospital, Rourkela, Orissa 769005, India.
2. D. Dermat., Specialist I/C, Skin & V.D.; Ispat General Hospital, Rourkela, Orissa 769005, India.
3. M.D., Specialist I/C, Internal Medicine;Ispat General Hospital, Rourkela, Orissa 769005, India.
4. M.D., Specialist I/C, Biochemistry; Ispat General Hospital, Rourkela, Orissa 769005, India.
5. M.D., Director. Medical & Health Services, Ispat General Hospital, Rourkela, Orissa 769005, India.
Reprint requests to Dr. Bose.
Received for publication on 27 October 1988.
Accepted for publication in revised form on 16 February 1989.