- Volume 57 , Number 2
- Page: 526–8
Relapse or late reversal reaction?
Editor's Note: In an effort to increase the utility of the JOURNAL in continuing medical education, it has been suggested that a new feature of the JOURNAL be added on a trial basis to the Editorial Section-Clinical Notes. In this section, we welcome contributions dealing with practical problems in leprosy work. Submissions to this section will undergo minimal editorial changes and may well contain controversial points. Letters to the Editor pointing out other viewpoints are welcome.- RCH
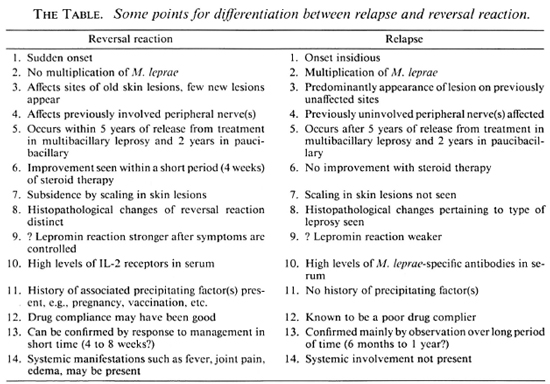
The clinical symptoms of active leprosy and of reversal reaction both reflect the cellular immune response to mycobacterial antigens. Clinically, it is often difficult to distinguish between relapse and reversal reaction.1,2 The histopathological criteria for differentiation are often inconclusive. Bacteriological examination is of little help, except in multibacillary leprosy, since smears of paucibacillary leprosy patients are usually negative. Although, in general, reversal reactions appear earlier after cessation of treatment than relapses, occasionally reversal reactions are seen one or more years after cessation of treatment. Data on time of relapse after multidrug therapy (MDT) are as yet insufficient, but preliminary data suggest that relapse is not common within the first few years after completion of MDT.3
Theoretically, the conventional criteria for relapse4 are: a) reappearance and multiplication of Mycobacterium leprae, reflected in an increase in the bacterial index (BI); b) appearance of skin lesions at previously unaffected sites; and c) appearance of neuritis in previously unaffected nerves. However, in practice, if we take into account the variability of skin-smear readings, only an increase of one unit or more in the average BI should be considered as indicative of rcmultiplication of M. leprae.
In practice, the old skin and nerve lesions are often not accurately mapped and it cannot be ascertained that the lesions are new. Therefore, the value of conventional criteria for distinguishing between relapse and reversal reaction is uncertain, and there is a need for well-defined criteria.
One potential criterion is the rapid response of reactive phenomena to treatment with corticosteroids. A second potential criterion is the outcome of serological tests with monoclonal antibodies against M. leprae-specific antigens.5
Probable reasons for relapse
Wrong classification. If a multibacillary leprosy case is wrongly classified as paucibacillary, the chances of relapse will probably be high. This can be correlated with: a) number of lesions; b) distribution of lesions; c) number of nerves involved; d) pattern of sensory loss on extremities; c) histopathological classification; and f) lepromin test.
Inadequate chemotherapy. In paucibacillary leprosy cases, where the duration of therapy is fixed, adequate drug compliance is essential to reduce the risk of relapse.
Drug resistance. In theory, primary infection with rifampin-resistant strains of M. leprae will give rise to relapse in paucibacillary cases.
Reinfection. The individual who has contracted leprosy probably has a greater risk of getting reinfected than an individual who has not contracted the disease. If the coverage with MDT is not adequate (< 75% of estimated cases), then the risk of relapse due to reinfection is possible. This risk of reinfection can also occur through migration of susceptibles to endemic areas where MDT is not yet introduced or where the coverage is inadequate.
Persisters. The existence of the phenomenon of persisting M. leprae is possible in both paucibacillary leprosy and multibacillary leprosy. However, the role of persisters attribule to the risk of relapse is not clear.2
Probable reasons for late reversal reaction
Clearance of M. leprae antigens. It is well known that the available drugs for MDT are responsible for bacterial killing. Bacterial clearance is probably related to the competence of the phagocytic system of the individual. This system is deficient to some extent in paucibacillary leprosy cases and to a large extent in multibacillary leprosy cases. The continued presence of antigen from dead M. leprae is a risk factor for the development of reversal reaction. There are probably methods to quantify this antigenic load in patients at the end of chemotherapy and to associate it with future risk of reversal reaction.
Relapse. Reversal reaction may occur due to remultiplication of M. leprae, increasing the antigenic load and consequently causing relapse and reversal reaction. In theory, relapse should precede reversal reaction if occurring due to multiplication of M. leprae. However, we do not have means available at the moment to differentiate between antigenic load due to viable and nonviable M. leprae.
Duration of treatment. In the past, the phenomenon of reversal reaction after discontinuation of dapsone monotherapy was rarely observed, and any reversal reactions occurring after discontinuation of therapy were probably classified as relapses.6-9 In most programs, the treatment of paucibacillary leprosy cases was continued for at least 5 years and for multibacillary leprosy, life-long. It may be assumed that the risk of reversal reaction, after starting treatment, in paucibacillary leprosy is at least for 5 years and in multibacillary leprosy is for life because clearance of antigens released from dead bacilli takes at least 5 years in paucibacillary leprosy and is never completed in multibacillary leprosy. Therefore, it may be worthwhile to search for ways to enhance bacterial clearance, such as immunotherapy with M. leprae and BCG, during or at the end of chemotherapy to reduce the risk of reversal reaction.
Other factors. Some other factors, such as pregnancy, vaccination, major illnesses, surgical procedures, emotional stress, blood transfusions, etc., may precipitate the development of reversal reaction, if such influence occurs before complete bacterial or antigen clearance is achieved.
In summary, if we can differentiate between the presence of live M. leprae and dead M. leprae, the diagnosis of relapse or reversal reaction is not difficult. However, in practice it is extremely difficult to differentiate these two phenomena by clinical manifestations alone. There is a need to accumulate accurate clinical data and specimens for laboratory tests to elucidate these differences by a large-scale prospective study.
- Vijayakumar Pannikar, M.B.B.S., M.Sc. (Lond.)
Associate Epidemiologist
- Kumar Jesudasan, M.B.B.S., Ph.D. (Lond.)
Head, Department of Epidemiology and Leprosy Control
- P. Vijayakumaran, M.B.B.S., D.P.H.
Senior Medical Officer
- Melville Christian, M.B.B.S.,
D.T.M.&H., Dip.Epid. (Prague)
Director
Schieffelin Leprosy Research and Training Centre, Karigiri
North Arcot District
Tamil Nadu 632106, India
Acknowledgment. The authors wish to express their gratitude to Dr. V. Benjamin, Interim Director, Schieffelin Leprosy Research and Training Centre, Karigiri. India, for giving permission to publish this paper. We also wish to thank Miss S. Sivaprakasam for secretarial assistance.
1. National Leprosy Eradication Programme in India: Guidelines for Multidrug Therapy in Endemic Districts. Rev. ed. New Delhi: Leprosy Division, Directorate of Health Services, Ministry of Health and Family Welfare, 1988.
2. WHO Expert Committee on Leprosy. Sixth Report. Geneva: World Health Organization, 1988. Tech. Rep. Ser. 768.
3. Leiker, D. L., Christian, M., Jacobson, R. R. and Pattyn, S. Report of THELEP subcommittee on relapse and reversal reaction in paucibacillary leprosy. Geneva: World Health Organization, 1987.
4. World Health Organization. TDR/THELEP/Protocol/82.1: Standard protocol for chemotherapy trials in nonlepromatous leprosy, 1988, 21-24.
5. Leiker, D. L. Reactive phenomena in paucibacillary leprosy (personal communication).
6. Erickson, P. T. Relapse following apparent arrest ofleprosy by sulphone therapy. Int. J. Lepr. 29(1951)63-74.
7. Lowe, J. The late results of sulphone treatment in East Nigeria. Lepr. Rev. 25(1954)113-124.
8. Quagliato. R., Hechelli, L. M. and Marques, R. M. Bacterial negativity and reactivation(relapse)of lepromatous outpatients under sulphone treatment. Int. J. Lepr. 38(1970)250-263.
9. Rodriguez, J. N. Relapses after sulphone therapy in leprosy of lepromatous type. Int. J. Lepr. 26(1958)305-312.