- Volume 57 , Number 1
- Page: 12–9
Single lesion subpolar lepromatous leprosy and its possible mode of origin
ABSTRACT
Three case reports of patients with a single, nodular, subpolar lepromatous skin lesion, one on the left elbow, another on the posterior aspect of the left leg, and the third on the extensor ulnar aspect of the right forearm, are presented. The lesions, clinically and histopathologically, resemble lepromas which develop at the site of experimental inoculation of Mycobacterium leprae in armadillos. These are sites on the body which are likely to be traumatized. With the distinct possibility of the presence of viable M. leprae in the soil of Louisiana and Texas f rom wild armadillos with the natural disease, it is suggested that these three patients acquired the infection f rom the environment and had inoculation lepromas.RÉSUMÉ
On présente ici trois études de cas chez des malades présentant une lésion cutanée unique nodulaire de lèpre infra-polaire. Chez un malade cette lésion était située sur le coude gauche, chez un autre sur la face postérieure de la jambe gauche, et chez le dernier au niveau de l'extenseur cubital de l'avant-bras droit. Cliniquement et histopathologiquement, ces lésions ressemblaient à des lépromes qui se seraient développées chez le tatou à l'endroit d'une inoculation expérimentale de Mycobacterium leprae. Ces endroits sont sur le corps ceux qui sont le plus susceptibles de subir des traumatismes. Comme le possibilité existe que des M. leprae viables soient présents dans le sol, en Louisiane et au Texas, provenant de tatous sauvages atteints de l'affection naturelle, on suggère que ces trois malades ont acquis l'infection à partir de l'environnement et qu'il s'agit de lépromes d'inoculation.RESUMEN
Se presentan 3 casos de pacientes con una sola lesión en piel de tipo nodular lepromatosa subpolar; una lesión estuvo sobre el codo izquierdo, otra sobre la cara posterior de la pierna izquierda, y la tercera sobre el lado ulnar extensor del antebrazo derecho. Las lesiones semejan clínicamente e histopatológicamente a los lepromas que se desarrollan en el sitio de inoculación experimental de Mycobacterium leprae en armadillos. Estos son sitios corporales sujetos a frecuentes traumatismos. Con la particular posibilidad de la presencia de M. leprae en el suelo de Louisiana y Texas, derivados de armadillos silvestres con lepra natural, se sugiere que estos 3 pacientes adquirieron la infección del medio ambiente y desarrollaron lepromas en el sitio de inoculación.Lepromatous leprosy is thought of as a generalized disease affecting much of the skin and most of the peripheral nerves. In wellestablished lepromatous leprosy, numerous macules, papules, or nodules are widely distributed in the skin, afecting the face, the cars, the trunk, and the extremities. There may also be diffuse, fine, or gross infiltration of the skin. Slit-skin smears from the skin lesions and from routine sites, such as the earlobcs, elbows, knees, and buttocks, are always positive for acid-fast bacilli.
In 1985, we reported a patient with a single nodular lesion on the left elbow with histologic, bacteriologic, and immunologic evidence of subpolar lepromatous disease (16) . It was considered a rare and unusual presentation of lepromatous leprosy. Since then we have encountered three more such patients, and they are the subjects of this report. It is possible that this unusual manifestation of lepromatous disease may be partly related to how the disease was acquired by these patients.
CASE REPORTS
Case 1, #3809. The patient was a 47-year-old Caucasian male from Louisiana, who had never traveled outside the U.S.A. He was admitted to the Gillis W. Long Hansen's Disease Center in June 1985 with a complaint of having a tingling sensation just proximal to his left elbow 4-5 years prior to admission. A nodule' gradually and insidiously developed in the same area. The patient was a truck driver and while working would traumatize this nodule with resultant bleeding, but he experienced no pain. He consulted a dermatologist who biopsied the lesion. A provisional diagnosis of lepromatous leprosy was made, and the patient was then referred to Carville for definitive diagnosis and therapy.
Physical examination revealed a 1 x 3 cm, erythematous, shiny, nodular lesion proximal to the left elbow. This lesion, which was elevated approximately 0.5 cm above the surrounding skin, showed diminished sensation along with the adjacent skin. There was also a minimal degree of sensory loss in the ulnar distribution on the left palm and border of the left hand. No other skin lesions were noted. There was no evidence of enlargement or tenderness of the ulnar, radial cutaneous, peroneal, sural, or greater auricular nerves.
Slit-skin scrapings from the site of the lesion showed a bacterial index (BI) of 4 + with a morphological index (MI) of 0%. Skin scrapings at the six additional routine sites (cars, elbows, and knees) were negative for acid-fast bacilli (AFB). Additional biopsies were done in two different areas of the skin lesion for histopathological examination, to culture for acid-fast organisms and for mouse foot pad inoculations. AFB from a a portion of one biopsy were injected into the mouse foot pads and a growth of from 5 x 103 to 6.8 x 105 bacilli in 6 months was noted. The organisms were sensitive to dapsone (0.01%, 0.001%, and 0.0001% in diet), and to clofazimine, 0.001%, and rifampin, 0.01% in the diet. Löwenstein-Jensen and Middlebrook 7H11 media were inoculated with the bacillary suspension, and no growth was reported after 6 weeks' incubation at 25ºC, 35ºC, and 42ºC.
The patient was placed on a daily regimen of 100 mg of dapsone and 600 mg of rifampin. In May of 1987 the lesion had regressed.
Histopathology. The biopsies were fixed in 10% buffered formalin, processed for paraffin sections, and 5 µm sections were made. The sections were stained with hematoxylin and eosin (H&E) and a modified Fite's stain for AFB (3).
Three biopsies taken within a period of 3 months were available for examination, and all showed a similar picture. The sections showed skin with minimal hyperkeratosis and proliferation of the epithelium. Beneath the epidermis was a clear zone which separated it from a granuloma occupying nearly 80% of the dermis (Fig. 1). The granuloma consisted of mostly macrophages infiltrating the collagen and encircling the skin appendages. There were diffusely scattered lymphocytes and plasma cells. Foamy degeneration of the macrophages was well marked. A dermal nerve was surrounded by macrophages. The arrectores pilorum muscle bundles were infiltrated and were partly destroyed. The inflammation extended to the subcutaneous tissue. In one of the biopsies, there was a small area composed mostly of haphazardly arranged, spindle-shaped macrophages.
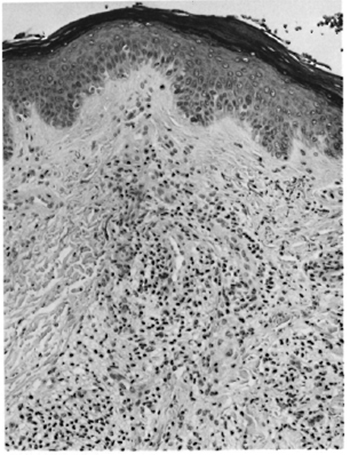
Fig. 1. Patient #1. Photomicrograph showing granuloma composed of mostly macrophages and scattered limphocytes (H&E x 100).
The acid-fast stain showed a very irregular distribution of organisms. In most areas the bacillary load was 5+ to 6+ (Fig. 2), but in some sites, especially in the deeper tissue, the load was only 3 + . Bacilli were also present inside the dermal nerve and arrectores pilorum muscle cells (Fig. 3). These bacilli lost their acid-fastness on treatment with pyridine. The histopathological picture was consistent with that of subpolar lepromatous leprosy.
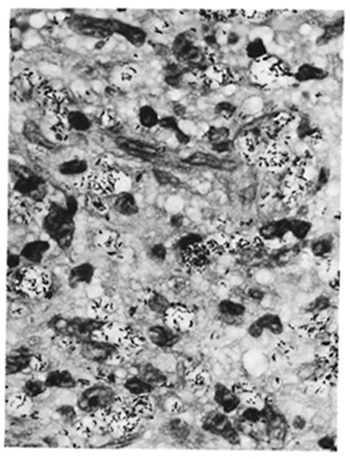
Fig. 2. Patient #1. Photomicrograph showing foamy macrophages, many containing clumps of AFB (H&E x 550).
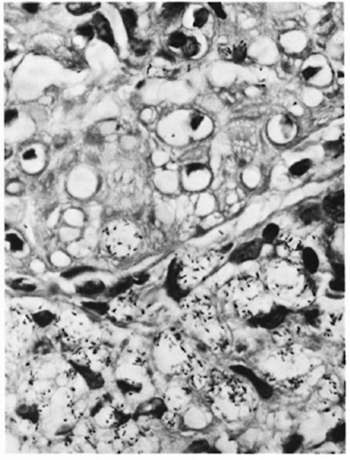
Fig. 3. Patient#1. Photomicrograph showing macrophages containing M. leprae infiltrating arrectores pilorum muscle bundles. The muscle cells contamn many M. leprae (modified Fite x 550).
Case 2, #3879. The patient was a 44-year-old black female, a native of southern Louisiana, who had never traveled outside the U.S.A. Approximately 6 months prior to admission in April of 1986, the patient noticed a nonpainful reddish-brown lump on the posterior aspect of her left leg. This nodule, measuring approximately 0.7 x 0.6 cm, was cosmetically unacceptable to the patient and was removed by excision biopsy in March of 1986. A diagnosis of lepromatous leprosy was made, and the patient was referred to Carville.
Physical examination revealed an area of dry, darkened skin over the posterior aspect of her left leg with a few sutures still in place. The patient's skin was otherwise unremarkable except for a few scattered burn scars on her extremities and a large, ovoid burn scar covering portions of her left lower breast and left upper abdomen. There was no loss of sensation even at the site of the original lesion. No nerve enlargement or tenderness was detected.
Slit-skin scrapings from the site of the original lesion and from six routine sites were all negative for AFB. A lepromin test was done and was biopsied at 21 days. The histopathological appearance was consistent with that of a borderline-lepromatous lepromin.
The patient was started on a daily regimen of 100 mg of dapsone and 600 mg of rifampin. She continued on this treatment and was last seen in January of 1987 without progression of disease.
Histopathology. The biopsy was fixed, processed, and sections made and stained as described for Case 1. Sections of the biopsy specimen showed skin with marked atrophy of the epithelium in several areas. Underneath the epithelium was a fairly well circumscribed nodular lesion invading the dermis and extending into the subcutaneous tissue. The epithelium in one area was much thinned, and the inflammation came up to the atrophic epidermis (Fig. 4). The lesion was composed of mainly macrophages which were mostly spindle shaped and arranged in interlacing bands (Fig. 5). In some areas they were intermingled with a few plasma cells and many lymphocytes. In the deeper area where the lesion was separated from the normal tissue there were a significant number of lymphocytes. There was also collagen formation with areas of hyalinization in scattered areas. Nerve bundles showed perineural thickening and infiltration of the perineurium with macrophages.
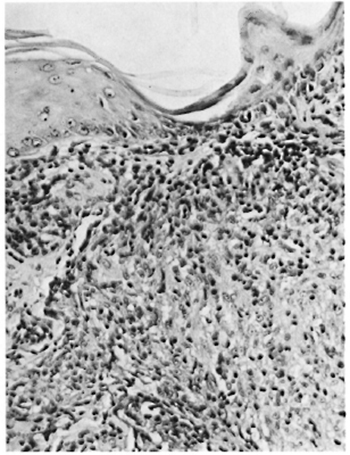
Fig. 4. Patient #2. Photomicrograph showing lepromatous granuloma coming up to the epidermis with marked atrophy of the epidermis (H&E x 160).

Fig. 5. Patient #2. Photomicrograph showing pre-dominantly spindle-shaped macrophages forming the granuloma (H&E x160).
Acid-fast staining showed bacilli with a varying BI of 2 + to 6 +. Bacilli were present inside spindle-shaped macrophages (Fig. 6) and nerve bundles (Fig. 7). The bacilli lost their acid-fastness on treatment with pyridine. A diagnosis of subpolar lepromatous leprosy with a prominent histoid component was made.

Fig. 6. Patient #2. Photomicrograph showing clumps of AFB inside the long, slender cytoplasm of spindle-shaped macrophages (modified Fite x650).
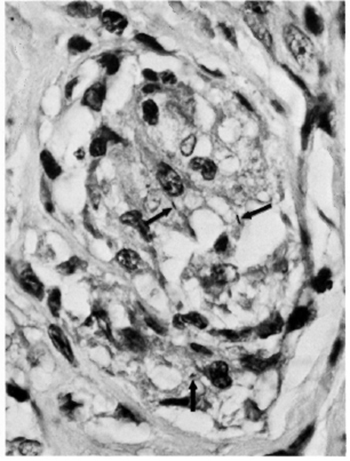
Fig. 7. Patient #2. Photomicrograph showing AFB inside nerve tissue (modified Fite x 650).
Case 3, #3952. The patient was a 29-year-old, Caucasian male, native of east Texas, who had never traveled outside the U.S.A. Approximately 3 months prior to admission in July 1987, the patient noted a "pimple" on the external ulnar aspect on his right forearm from which he expressed "pus." The lesion healed but the patient felt a "hard knot" about 0.5 cm in diameter under the site of the pustule. Two weeks prior to admission, the patient visited his family physician who palpated a bilobular, subcutaneous nodule -each lobe approximately 0.4 cm in diameter. There was no loss of sensation or hair and there was only slight elevation of the skin. The nodule was removed by excisional biopsy. A diagnosis of lepromatous leprosy was made, and the patient was referred to Carville.
Physical examination of the patient revealed a well-healed, 1-cm-long scar at the external ulnar aspect of the right forearm with slight surrounding erythema. No anesthesia was noted at the site. Skin examination was otherwise negative except for small brown macules covering his upper body and arms. They were felt to be sequelae of pimple-like lesions. Peripheral nerves were not tender or enlarged.
Slit-skin scrapings from the site of the original lesion showed a 131 of 2+ with an MI of 0%. Skin scrapings at six additional (routine) sites were negative for AFB. A biopsy was taken next to the site of the original lesion. Half of the biopsy was cultured for mycobacteria; the other half was processed for histology. After 6 weeks' incubation of a suspension from this biopsy on Löwenstein-Jensen and Middlebrook 7H11 media at 25ºC, 35ºC, and 42ºC, no growth was reported.
The patient was started on 100 mg of dapsone and 600 mg of rifampin daily. On a return visit in December 1987, no new skin lesions were noted and skin scrapings at routine and selected sites were all negative.
Histopathology. The biopsies were fixed and processed, and sections were made and stained as for Case 1. Sections from the first biopsy showed skin and subcutaneous tissue. The epidermis was unremarkable. In the deep dermis with extension to the subcutaneous tissue there was a fairly well circumscribed, multilobulated nodule composed mostly of interlacing bundles of spindle-shaped macrophages, with a few macrophages with abundant foamy cytoplasm (Fig. 8). There were diffusely scattered lymphocytes and plasma cells which increased in number toward the periphery of the nodule, especially in areas of the nodule adjoining the normal tissue. Nerve bundles showed perineural thickening and infiltration of the perineurium with macrophages.
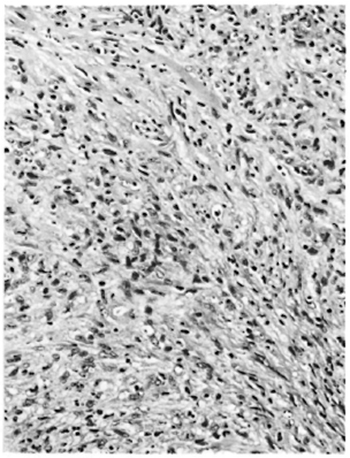
Fig. 8. Patient #3. Photomicrograph showing spindle-shaped macrophages forming major portion of the granuloma and also deposition of collagen between the cells (H&E x 160).
Acid-fast staining showed numerous bacilli inside macrophages, with the bacterial load varying from 3+ to 6 + . Acid-fast organisms were also present inside the nerves (Fig. 9) and arrectores pilorum muscle cells. The bacilli lost their acid-fastness on treatment with pyridine. A diagnosis of subpolar lepromatous leprosy showing marked histoid changes was made.

Fig. 9. Patient #3. Photomicrograph showing a nerve bundle with perineurium infiltrated by macrophages containing AFB. Schwann cells also show intraneural AFB (modified Fite x 650).
The second biopsy showed skin and subcutaneous tissue. The epithelium was unremarkable. In the dermis there were fibrous tissue and several foreign-body giant cells and macrophages around fragments of cotton liber. Acid-fast staining showed no bacilli. A diagnosis of skin with scar tissue and foreign body reaction was made.
DISCUSSION
Clinical examination of the three patients revealed no skin lesions other than the single nodular lesion each one of them complained of. All of the peripheral nerves which are likely to be involved in disseminated leprosy were clinically normal. The skin smears obtained from the sites of the nodular lesions after the attempted excision biopsy were positive in two patients and negative in one. Six other smears taken from routine skin sites in all three patients were negative for acid-fast organisms. Therefore, it is reasonably certain that the patients had only one skin lesion. However, it is possible that some of the peripheral nerves could be affected. Subclinical involvement could have been detected only through multiple nerve biopsies and, therefore, cannot be ruled out. Patient #1 had a minimal loss of sensation in the ulnar border of the left hand and palm. He had the skin lesion for nearly 5 years, and it is very likely that the ulnar nerve in this patient was involved in the disease process.
In patient #1, biopsy material was available to study the growth of the organism in mouse foot pads and to do cultures in laboratory mycobacterial culture media. In patient #3, only cultures of the organisms in laboratory media were done. The growth pattern in mouse foot pads and drug sensitivities were the same as that of M. leprae, and the organisms failed to grow in laboratory media.
In all three patients the biopsy showed an inflammatory lesion composed mostly of macrophages admixed with plasma cells and lymphocytes. In patient #1 many of the macrophages had a large cytoplasm with foamy degeneration, and a small proportion of them were spindle shaped. In patients #2 and #3 most of the macrophages were spindly and the patients' diseases were considered as histoid variants. In all three patients there was unequivocal evidence of infiltration of dermal nerves by acid-fast organisms, and the bacterial load was up to 6 + in many areas of the sections. Therefore it is reasonable to conclude that these three patients each had a single skin lesion of subpolar lepromatous disease.
Although the exact route by which leprosy is most likely to be transmitted remains controversial, transmission through the skin and via the nasal route are more commonly proposed based on available evidence. The site of the lesion in patient #1 was the left elbow, and he gave a history of repeated trauma or bleeding. In patient #2 the lesion was at the posterior aspect of the left leg and in patient #3 it was at the external ulnar aspect of the right forearm. All of these skin areas are directly exposed to the environment and are likely to be traumatized.
In patient #1 the lesion was nearly 4 to 5 years old by history and measured 1 cm x 3 cm. Three representative biopsies were done from the lesion and the lesion was too big to reconstruct the picture from its inception. In patient #2 the nodule was only 6 months old by history, was less than 0.7 cm in diameter, and was totally excised. It was fairly well circumscribed and involved the epidermis and the dermis. In patient #3 the nodule was only 3 months old by history, was lobulated, was 0.8 cm in diameter, and was completely excised. It was fairly well circumscribed and involved the dermis and the subcutaneous tissue.
In the armadillo, an animal highly susceptible to leprosy, the first sign of the disease is a nodule at the site of inoculation of the M. leprae suspension (6,15). The histopathology of the first lesions in the intradermally inoculated animal shows a macrophage granuloma with a significant component of spindle-shaped cells (7), which is similar to what was seen in these patients. The skin lesion at the inoculated site of one of the first armadillos experimentally infected with M. leprae showed histiocytes containing AFB coming up to the epidermis, and there was no clear zone separating the basal layer of the epidermis from the infiltrate of the dermis (9). The histopathology of the skin lesion in patient #2 (Fig. 4) is exactly like what was described in the inoculated site of the armadillo. The "free zone" was absent. There is a great similarity between the histopathologic appearances of the first skin lesion in the armadillo at the site of inoculation and those of the lesions of the patients reported here.
It is now a well-established fact that leprosy exists in Louisiana and Texas in wild armadillos, and that the disease is caused by M. leprae (12). The disease has been found in armadillos living in close proximity to humans (4). The number of M. leprae discharged into the environment from these animals, living and dead, is enormous. A lepromatous armadillo can have up to 1010 bacilli per gram of infected tissue (8). There is evidence to show that M. leprae can remain viable in moist soil up to 46 days (1). Also, an association between human leprosy and contact with armadillos has been reported by many authors (2, 10, 11, 14).
These three patients showed highly unusual, single lesion, lepromatous leprosy. The sites of the lesions were areas susceptible to being traumatized. The clinical and histopathologic characteristics of the lesions were the same as those of inoculation lepromas in experimentally infected armadillos. The patients were from areas of Louisiana and Texas which are known to have natural leprosy among wild armadillos. Large numbers of viable M. leprae can be shed into the environment from armadillos with natural leprosy, and these organisms can remain viable for extended periods of time in the environment. We feel it reasonable to suggest that these three patients were highly susceptible to leprosy, and that they acquired the infection by means of trauma which lodged a significantly large dose of viable M. leprae from the environment into the skin to produce inoculation lepromas. It has been suggested that leprosy can be transmitted among armadillos in nature through inoculation of M. leprae following trauma (5, 13). Further testing of this hypothesis may require the development of genetic probes of M. lepraecapable of identifying different strains of the organism.
Acknowledgments. We would like to acknowledge with gratitude the excellent technical help from Mr. John Marcell, secretarial assistance from Mrs. Mary M. Jackson, and the photographic work by Mr. Gregory T. McCormick.
REFERENCES
1. Desikan, K. V. and Sreevasta. Studies on viability of M. leprae outside the human body. Lepr. India 51(1979)588-589.
2. Freiberger, H. F. and Fudenberg, H. An appetite for armadillo. Hosp. Pract. 16(1981)137-144.
3. Job, C. K. and Chacko, C. J. G. A modification of Fite's stain for demonstration of M. leprae in tissue sections. Indian J. Lepr. 58(1986)17-18.
4. Job, C. K., Harris, E. B., Allen, J. L. and Hastings, R. C. A random survey of leprosy in wild nine-banded armadillos in Louisiana. Int. J. Lepr. 54(1986)453-457.
5. Job, C. K., Harris, E. 13., Allen, J. L. and Hastings, R. C. Thorns in armadillo ears and noses and their role in the transmission of leprosy. Arch. Pathol. Lab. Med. 110(1986)1025-1028.
6. Job, C. K. , Sanchez, R. M. and Hastings, R. C. Manifestations of experimental leprosy in the armadillo. Am. J. Trop. Med. Hyg. 34(1985)151-161.
7. Job, C. K., Sanchez. R. M., McCormick, G. T. and Hastings, R. C. First lesion in experimental armadillo leprosy. Indian J. Lepr. 57(1985)71-77.
8. Kirchheimer, W. F. and Sanchez, R. M. Quantitative aspects of leprosy in armadillos. Lepr. India 49(1977)48-53.
9. Kirchheimer, W. F., Storrs, E. E. and Binford, C. H. Attempts to establish the armadillo(Dasypus novemcinctus Linn.)as a model for the study of leprosy. Int. J. Lepr. 40(1972)229-241.
10. Lumpkin, L. R., Ill, Cox, G. F. and Wolf, J. E., Jr. Leprosy in five armadillo handlers. J. Am. Acad. Dermatol. 9(1983)899-903.
11. Lumpkin, L. R., Ill, Cox, G. F. and Wolf, J. E., Jr. Leprosy in armadillo handlers.(Letter)J. Am. Acad. Dermatol. 10(1984)1073.
12. Meyers, W. M., Walsh, G. P., Binford, C. H., Storrs, E. E. and Brown, H. L. Indigenous leprosy in nine-banded armadillos. In: The Armadillo as an Experimental Model for Leprosy Research. Washington, D.C.: Pan American Health Organization, 1978, pp. 67-76. PAHO Scicn. Publ. No. 366.
13. Smith, J. H., File, S. K., Nagy, B. A., Folse, D. S., Buckner, J. A., Webb, L. J. and Beverding, A. M. Leprosy-like disease of wild armadillos in French Acadiana, Louisiana. J. Reticuloendothel. Soc. 24(1978)705-719.
14. Thomas, A. T., Mines. S. J., Thomas, D. C, Mack, T. M. and Rea, T. H. Armadillo exposure among Mexican-born patients with lepromatous leprosy.J. Infect. Dis. 156(1987)990-992.
15. Walsh, G. P. Experimental leprosy in the ninebanded armadillo(Dasypus novemcinctus). In: The Armadillo as an Experimental Model for Leprosy Research. Washington, D.C.: Pan American Health Organization. 1978, pp. 57-63. PAHO Scien. Publ. No. 366.
16. Yoder, L. J., Jacobson, R. R. and Job, C. K.A single skin lesion-an unusual presentation of lepromatous leprosy. Int. J. Lepr. 53(1985)554-558.
1. M.D., F.R.C.Path., F.A.M.S., Chief; M.
2. M.D., Medical Officer (Research), Pathology Research Department.
3. M.D., Ph.D., Chief, Clinical Branch.
4. M.D., Ph.D., Chief, Laboratory Research Branch, GWL Hansen's Disease Center, Carville, Louisiana 70721, U.S.A.
Received for publication on 28 June 1988.
Accepted for publication in revised form on 28 October 1988.