- Volume 67 , Number 1
- Page: 6–12
Pregnancy and leprosy: a comprehensive literature review
ABSTRACT
The interaction between pregnancy, leprosy and leprosy reactions was examined in a systematic literature review. Several retrospective case series and one retrospective cohort study but only one prospective cohort study were identified in the English literature. Type 1 (reversal) reactions were particularly likely to occur during the post partum. This temporal association was also present for both overt and silent neuritis. Type 2 (erythema nodosum leprosum) reactions occur throughout pregnancy and during lactation, and may be severe and recurrent. No prospective, controlled studies were found that documented the complications of pregnancy in women treated with multidrug therapy regimens. Our study highlights the need for such studies, with appropriate controls, on women throughout pregnancy and lactation so that risk factors for reaction and neuritis during pregnancy can be identified and quantified.RÉSUMÉ
L'interaction entre la grossesse, la lèpre et les réactions lépreuses fut examinée au cours d'une revue systématique de la littérature. Plusieures séries rétrospectives de cas, une étude par cohorte rétrospective et seulement une étude par cohorte prospective furent identifiées dans la littérature anglaise. Les réactions de type 1 (réversions) étaient particulièrement susceptibles d'apparaître en post-partum. Cette association temporelle était présente à la fois pour les névrites asymptômatiques ou déclarées cliniquement. Les réactions de type 2 (érythème noueux lépreux) étaient présentes pendant toute la grossesse et durant l'allaitement, et elles pouvaient être sévères et récurrentes. Il n'a pas été trouvé d'étude prospective contrôlée qui documente les complications de grossesse chez les femmes traitées par la polychimiothérapie (PCT). Notre étude révèle le besoin pressant d'entreprendre de telles études, avec contrôles appropriés, à partir de femmes durant toute la période de grossesse et d'allaitement afin que les facteurs de risque de développer des réactions et des neurites soient identifiés et quantifiés.RESUMEN
Se hizo una extensa revision de la literatura inglesa para analizar las interacciones entre el embarazo, la lepra y la reacción leprosa. Se encontraron vários estúdios retrospectivos, un estúdio retrospectivo de cohortes y un estúdio prospectivo de cohortes. Las reacciones de tipo 1 (reversas) ocurrieron frecuentemente durante el periodo de post-parto. Esta asociación temporal también se observoó con las neuritis tanto abiertas como silentes. Las reacciones de tipo 2 (eritema nodoso leproso) ocurrieron durante el embarazo y la lactancia y a veces fueron severas y récurrentes. No se encontraron estúdios prospectivos controlados que documentaran las complicaciones de embarazo en las mujeres tratadas con poliquimioterapia. Nuestro estúdio subraya la necesidad de tales estúdios, con controles apropiados, durante el embarazo y'a lactancia. Esto ayudaría a identificar y cuantificar los factores de riesgo de reacción y de neuritis durante el embarazo.Sixty years ago Ryrie (17 ) wrote: "In the interaction of pregnancy and associated pathological conditions, leprosy must be one of the few major systemic diseases where such action is totally one sided. Leprosy does not have the slightest effect on the course of pregnancy; pregnancy has a marked effect on leprosy." This observation remains broadly true although few detailed studies have been produced on the interaction of pregnancy and leprosy in the last 60 years. This review critically appraises the available published literature on the effects of pregnancy and lactation on disease activity, type 1 and type 2 leprosy reactions, and neuritis.
The search strategy used was a search of the MEDLINE (from 1966 to 1997) and BIDS (from 1961 to 1997) bases and the compact disc of leprosy literature for 1913-1991 (1) using the key words leprosy, pregnancy, fertility and women. We identified 223 publications with this search; only papers with original data were studied, single case reports were excluded. Relevant cross-references from the above papers were also referred to, and a critical analysis of the published data was performed without statistical calculations.
Fifteen papers were studied. Of these, 1 (19) was a retrospective cohort study at a leprosarium, 5 (11, 12, 14-16) were case series, and 9 (4-10) were papers which reported on various studies of the same cohort in Ethiopia. The retrospective cohort study had no controls, while the prospective Ethiopian study used contacts of cases as controls rather than nonpregnant women with leprosy. Comparison of the various publications is difficult because some studies reported the number of patients, while others used the number of pregnancies. Pregnancy and the puerperium have different effects on the course of leprosy so, in this review, the disease complications of leprosy are analyzed by timing in relation to pregnancy. Each section starts with a commentary on the theoretical effects of pregnancy on leprosy and then reviews the actual observations.
Effect of Pregnancy on Leprosy
Theory
There is a relative suppression of T-cell activity during pregnancy, and pregnant women are more susceptible to viral infections such as hepatitis and intracellular pathogens such as toxoplasmosis (13). Thus, pregnant women could also be at greater risk of developing leprosy. Case reports over the last 60 years have documented the association between pregnancy and the first diagnosis of leprosy, or an exacerbation of symptoms in patients with established disease (5, 10-12, 19). These case reports are inevitably retrospective and may be affected by responder bias during recall and the increased contact that pregnant women have with medical services.
Observations
First presentation of leprosy during pregnancy. The first publication on pregnancy and leprosy is Tajiri's (19) retrospective 1936 study of a cohort of 240 female Japanese patients, in which he reported that 20.5% of the cases presented for the first time in pregnancy. King and Marks (12) reported on 26 patients in the U.S.A., where nine (34.6%) of the patients had presented with leprosy during or shortly after a pregnancy. Both of these studies were on patients resident in leprosaria. In 1997 Lyde (l4) reported on two cases of first presentation of leprosy during pregnancy in Dallas, Texas, U.S.A.
In a study examining the rate of new leprosy during pregnancy, Duncan, et al . (5) examined Ethiopian women living in villages around the Addis Leprosy Hospital in Ethiopia who had attended the leprosy hospital's antenatal clinics. Of 33 apparently health control women one developed biopsy-proved indeterminate leprosy during pregnancy (giving a rate of 3.0%). Duncan, et al. compare this rate of 3% with the reported new case rate of 0.1% in the villages surrounding the leprosy hospital. However, the sex ratio of this reported new case rate in villages is not given, nor is any information about case ascertainment, control recruitment or contact with leprosy patients. We were unable to locate any studies reporting the incidence of new leprosy cases during pregnancy in field surveillance programs.
Disease activity during pregnancy. Increased disease activity during pregnancy can be due to either disease progression or immunological complications. Both Tajiri and King and Marks reported so-called aggravation of leprosy during pregnancy. None of these authors defines aggravation, so it is unclear whether they are reporting disease progression or reactions. Tajiri (19) noted 48 cases of aggravation in 100 pregnancies. King and Marks (l2) in their study of lepromatous cases found that in 78% of pregnancies there was aggravation of disease when the patient was untreated, while it was aggravated in only 22% of pregnancies when the patient was on treatment with sulfones.
Immunological complications during pregnancy. Theory . Part of the normal physiology of pregnancy is a relative immunosuppression with the maternal immune response being directed away from cell-mediated immunity toward humoral immunity (21)- There is a down-regulation of Thl type responses during pregnancy with decreased production of IL-2, especially during the third trimester. Seventy percent of women with rheumatoid arthritis (a cell-mediated auto-immune pathology) experience a temporary remission of their symptoms during pregnancy Q. In contrast, systemic lupus erythematosus, which has an antibody-mediated pathology, worsens during pregnancy (2). Thus, one might predict that in leprosy type 1 reactions, which are due to increased cell-mediated immunity toward Mycobacterium leprae antigens, might be ameliorated during pregnancy while type 2 (erythema nodosum leprosum; ENL) reactions, which are principally due to the deposition of immune complexes and complement activation, would be increased.
Observations. Type 1 (reversal) reaction . Of 116 patients in the prospective cohort study (10) in Ethiopia, Duncan, et al . reported type 1 reaction in 40 cases. However, only 16 of these type 1 reactions were during pregnancy and 24 occurred during the post partum. Reactions occurred in all three trimesters. In the absence of controls it is impossible to ascertain whether this data shows a decrease in type 1 reactions during pregnancy.
Type 2 reaction . Pregnancy has been reported as precipitating ENL (l4). Maurus (14) reported in a retrospective study over the period 1957-1975 that 32% of the active cases in his study of 26 women under treatment through 62 pregnancies had episodes of ENL. These data were derived from the records at Carville, Louisiana, U.S.A. and the New Orleans Public Health Hospital, U.S.A. No data were given on the clinical features of ENL in these women nor of the timing of the ENL episodes in relation to pregnancy and parturition. It was not reported whether these women had experienced previous episodes of ENL. However, 68.7% of the women in this cohort with a bacterial index of >4+ had experienced ENL during pregnancy. Duncan and Pearson (8) followed a cohort of 76 women with multibacillary disease (LL 32, BL 44) through pregnancy and lactation; 38% developed ENL during the study, with rates of 22% for BL and 59% for LL patients, respectively. The timing of the first episode of ENL appears to show a small excess of initial episodes of ENL in the first trimester of pregnancy but initial episodes occur throughout pregnancy and up to 15 months post partum. In this study ENL during pregnancy was most commonly a skin manifestation. When all ENL episodes are considered in this cohort it can be seen that ENL occurs throughout pregnancy and lactation.
Neuritis. Duncan and Pearson (7) are the only authors to have specifically recorded nerve function during and after pregnancy. In their Ethiopian cohort 52 patients had 85 episodes of neuritis. The majority of these episodes occurred after delivery and will be considered in the following section. Borderline lepromatous (BL) patients had the lowest incidence of neuritis during pregnancy, with only 8.5% of episodes occurring during pregnancy, but a much increased risk after delivery. The comparative figure for episodes of neuritis during pregnancy are 34.6% in LL patients and 25% in TT/BT patients.
Relapse
The decrease in cell-mediated immunity during the latter half of pregnancy also might put women at risk of leprosy relapse. The only data on relapse rates during pregnancy comes from the Duncan, et al . (5) Ethiopian cohort study and they included a group of clinically cured BT and TT patients. They reported that of 25 tuberculoid and borderline tuberculoid patients released from treatment after monotherapy nine relapsed with active leprosy (6 BT, 3 BL) during pregnancy or lactation. Five out of the nine relapses occurred during the third trimester of pregnancy. Treatment for leprosy had been completed 3 months to 3 years previously. No other study has followed cured cases through pregnancy. Of 18 women with clinically active TT or BT disease and on dapsone monotherapy eight had a transient increase in skin lesion activity, usually in the third trimester. In three cases the lesions developed erythematous margins and in four cases there was a conversion from BI negativity to BI positivity. There was no histological evidence of reaction in these cases. Among 68 women with BL or LL disease 38 had increased disease activity during pregnancy, in 20 cases this was during the third trimester. In 34 of these cases the increased activity was confirmed by a rise in the BI and in four cases increased activity was confirmed by biopsy only. In 16 cases this increased activity was only a transient phenomenon and the BI fell during lactation; five patients had histologically confirmed downgrading from BL to LL during pregnancy. This study was conducted during the transition between monotherapy and MDT, and during the time when cases of dapsone resistance were being recognized. Among 67 multibacillary cases documented by Duncan, et al. 15 cases of BL and 13 of LL clinically dapsone-resistant relapses were found (9).
Lyde (14) reported a case of relapse during the pregnancy of a Mexican woman with lepromatous leprosy who had received 20 months of daily rifampin and dapsone therapy and 2 years later, at the onset of her next pregnancy, presented with a lepromatous relapse. This case indicates that relapse remains a possibility even after multidrug therapy.
Puerperium, Lactation and Leprosy
Theory
Following parturition, there is a recovery of cell-mediated immunity in the mother, and this puts women at risk of developing immune-mediated complications. Although puerperium and lactation were well recognized by earlier leprologists (3) as a time when acute reactions could occur, it was only in 1975 that the first case series of reactions associated with pregnancy was published (16).
Observations
Type 1 reactions. Rose and McDougall (16) documented type 1 reactions in seven women with borderline leprosy from Guyana and Zambia. The reactions developed from 3-16 weeks after delivery, and all of the women presented with large, erythematous skin lesions. Rapid, severe nerve damage was also a prominent feature, with four of the cases having major nerve trunk damage and resultant paralysis with foot drop, lagophthalmos and claw hand all being reported.
The cohort study from Ethiopia (7) demonstrates a clear increase in the number of type 1 reactions after delivery, especially in the first 6 months of lactation. The Table gives the numbers of women having type 1 reactions at each stage of pregnancy and lactation. During pregnancy and lactation BL patients were at greatest risk, with 42% of pregnancies being complicated by a type 1 reaction. For BT and LL patients the rates were 27% and 29%, respectively. Nerve damage was also prominent in this cohort with 90% (36/40) of the patients having either nerve or skin and nerve involvement. Unfortunately, the data are not subdivided by disease type and timing so that the risk for women at different time points of pregnancy and lactation cannot be calculated. Recurrent type 1 reactions were also a feature in this group, but it is not possible to calculate from the data how many women were affected.
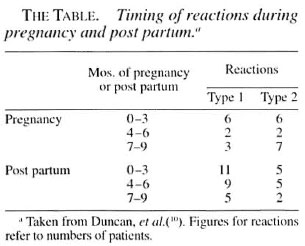
Type 2 reactions. Type 2 reactions, unlike type 1 reactions, do not have a clear temporal association with delivery and lactation (The Table). In the Ethiopian study (8), the first presentation of ENL occurred throughout pregnancy with a decline during lactation. However, recurrent ENL persisted throughout delivery and lactation, with 15% of the group experiencing ENL for the 18-month period from the third trimester to 15 months post partum. A significant increase in neuritis was seen in the women with ENL, of whom 70% had neuritis during pregnancy compared with 30% in the nonENL group. Thirty episodes of ENL with significant motor and/or sensory loss occurred, and almost every episode involved multiple nerves. Involvement of other systems was also noted with eye, bone and joint problems.
Neuritis. The data of Duncan and Pearson (7) show a clear association between the puerperium and the development of neuritis. They reported patients with overt neuritis, i.e., pain and/or nerve tenderness, and also patients with silent neuritis, i.e., impairment of sensory and/or motor function without nerve pain or tenderness. Their paper presents data relating partially to the numbers of patients and partially to the episodes of neuritis. Thus it is not possible to calculate the percentages of patients in each category who had neuritis post partum. However, 40% of TT/BT patients, 47% of BL and 44% of LL patients had neuritis during pregnancy and lactation. The association of neuritis and the post partum was strongest in the BL patients; 21 patients had 35 episodes of neuritis, only three of these episodes occurred during pregnancy. In all, 52 patients had 85 episodes of neuritis with 74 episodes resulting in nerve damage. Both type 1 and type 2 reactions contributed to the category of overt neuritis. Silent neuritis occurred in 14 out of 52 patients in this study. The details of the nerves involved were not presented.
Fetal Health and Pregnancy
Few obstetric problems have been reported in women with leprosy, irrespective of the disease type. In an early leprosarium- based study, Maurus (15) reported a rate of pregnancy complications of 532 in his 26 patients through 62 pregnancies. There were no controls in this study. He also found a 22% rate of prematurity with 17% fetal demise. This has not been seen in the study in Ethiopia (5,10'). Duncan found the pregnancies uncomplicated. However, in the Ethiopian cohort (4), babies of lepromatous mothers weighed significantly less than those of other leprosy mothers as well as controls. The placental weight and placental coefficient (baby weight + placental weight) was also less, but the gestational age was not recorded. In the same study, 80% of the babies of lepromatous patients were severely under weight at 12 months of age compared to the Boston standard.
An assay of estrogen excretion may be used as an index of feto-placental function. Estrogen excretion was assayed in 64 women with leprosy and 15 controls in the Ethiopian cohort (6). Mean estrogen excretion between 32 and 40 weeks' gestation was found to be lowest in lepromatous patients and highest among the controls. This probably reflects decreased uteroplacental perfusion. No explanation has been put forward for the low level found in lepromatous cases.
Fertility and Leprosy
Leprosy has not been found to have any effect on menarche, the menstrual cycle or fertility, as reported by Tajiri (19) in his retrospective cohort and Hardas, et al . (11) in a case study. No prospective studies have been reported. In contrast to males, where sterility occurs after involvement of the testes in lepromatous leprosy, the ovaries remain free from granulomas. Hardas, et al . found no evidence of involvement in four ovary specimens studied.
DISCUSSION
Reviewing the accumulated information on pregnancy and leprosy illustrates the lack of hard data relevant to current practice. From the available information one cannot tell a pregnant leprosy patient what her risk is of developing a post-partum type 1 reaction or even give the patient being released from control any indication of how long she may be at risk of developing a post-partum reaction. Only one prospective cohort study has followed women with leprosy through pregnancy and lactation. The findings from the study in Ethiopia cannot be extrapolated to populations in Asia, Latin America or even other parts of Africa.
In the cohort study from Ethiopia, healthy contacts of cases were taken as controls; appropriate controls would have been nonpregnant women with leprosy. The use of such controls would have permitted the calculation of the relative risks of developing reactions in the various stages of pregnancy and lactation.
A further weakness of the current data is that the earlier studies (12, 19) were done in the pre-sulfone and sulfone eras, while the Ethiopian studies (5, 7-10) were done during the pre-MDT era and during the initial implementation of MDT. It is possible that the current multibacillary drug regimen with its clofazimine component protects women against developing ENL during pregnancy, or it may protect them from experiencing the severe recurrent ENL that was reported in the Ethiopian study, but this hypothesis needs to be tested in an observational study. MDT may have little effect on the incidence of post-partum type 1 reactions because even after the completion of MDT M. leprae can persist in the skin and peripheral nerve. Thus, with the restoration of full cell-mediated immunity after delivery previously unrecognized antigen may precipitate a type 1 reaction. The question of differentiating between relapse and late type 1 reaction in the post-partum woman is particularly difficult and pertinent. The persistence of live but dormant M. leprae in peripheral nerve as demonstrated by Shetty, et al . (18) may partly explain the severity of post-partum neuritis, if multiplication of organisms occurs during the relative immunosuppression of pregnancy and if the post-delivery recovery of cell-mediated immunity coincides with an increased bacterial load in the peripheral nerve then severe neuritis could ensue.
It is important that a cohort of women treated with MDT and released from control should be followed up to establish how long the risk of post-partum reaction persists after completion of treatment. The data on relapse suggest that this was a significant problem during the monotherapy era. The risk of pregnancy-associated relapse after treatment with MDT needs to be established and particular attention paid to whether women with an initially high BI are particularly at risk.
The lack of any study from India on this problem is surprising, particularly given the high number of patients and the large vertical control programs that could have such data.
Studies that could be done include: following a cohort of women of childbearing age with leprosy throughout pregnancy complications as well as leprosy complications, such as reactions, extensions of lesions, and neuritis. Nonpregnant women, matched for disease type, nerve involvement, treatment duration and social class would serve as controls. These studies would address the important unanswered questions about reactions, neuritis and relapse in pregnant and newly delivered women.
Acknowledgment. Dr. H. H. Sinha was supported by a World Health Organization Training Fellowship.
REFERENCES
1. Compact Disc of Leprosy Literature, 19131991. Loma Linda, California, U.S.A.: Leprosy Research Foundation, 1993.
2. Da Silva, J. A. and Spector, T. D. The role of pregnancy in the course and etiology of rheumatoid arthritis. Clin. Rheumatol. 11(1992)189-194.
3. Davey, T. F. and Schenck, R. R. The endocrines in leprosy. In: Leprosy in Theory and Practice. 2nd edn. Cochrane, R. G. and Davey, T. F., eds. Bristol: John Wright & Sons Ltd., 1964, p. 200.
4. Duncan, M. E. Babies of mothers with leprosy have small placentae, low birth weights and grow slowly. Br. J. Obstet. Gynecol. 87(1980)471-479.
5. Duncan, M. E., Melsom, R., Pearson, J. M. H. and Ridley, D. S. The association of pregnancy and leprosy. I. New cases, relapse of cured patients and deterioration of patients on treatment during pregnancy and lactation-results of a prospective study of 154 pregnancies in 147 Ethiopian women. Lepr. Rev. 52(1981)245-262.
6. Duncan, M. E. and Oakey, R. E. Estrogen excretion in pregnant women with leprosy: evidence of diminished feto-placental function. Obstet. Gynecol. 60(1982)82-86.
7. Duncan, M. E. and Pearson, J. M. H. Neuritis in pregnancy and lactation. Int. J. Lepr. 50(1982)31-38.
8. Duncan, M. E. and Pearson, J. M. H. The association of pregnancy and leprosy. III. Erythema nodosum leprosum in pregnancy and lactation. Lepr. Rev. 55(1984)129-142.
9. Duncan, M. E., Pearson, J. M. H. and Rees, R. J. W. The association of pregnancy and leprosy. II. Pregnancy in dapsone resistant leprosy. Lepr. Rev. 52(1981)263-270.
10. Duncan, M. E., Pearson, J. M. H., Ridley, D. S., Melsom, R. and Bjune, G. Pregnancy and leprosy: the consequences of alterations of cell mediated and humoral immunity during pregnancy and lactation. Int. J. Lepr. 50(1982) 425-435.
11. Hardas, U., Survey, R. and Chakrawarti, D. Leprosy in gynecology and obstetrics. Int. J. Lepr. 40(1972)399-401.
12. King, J. A. and Marks, R. A. Pregnancy and leprosy; a review of 52 pregnancies in 26 patients with leprosy. Am. J. Obstet. Gynecol. 76(1958)438-442.
13. Luft, B. J. and Remington, J. S. Effect of pregnancy on resistance to Listeria monocytogenes and Toxoplasma gondii infections in mice. Infect. Immun. 38(1982)1164-1171.
14. Lyde, C. B. Pregnancy in patients with Hansen's disease. Arch. Dermatol. 133(1997)623-627.
15. Maurus, J. N. Hansens' disease in pregnancy. Obstet. Gynecol. 52(1978)22-25.
16. Rosk, P. and McDougall, A. C. Adverse reactions following pregnancy in patients with BL leprosy. Lepr. Rev. 46(1975)109-114.
17. Ryrie, G. A. Pregnancy and leprosy. Br. Med. J. 2 (1938)39-40.
18. Shetty, V. P., Suchitra, K., Upelakar, M. W. and Antia, N. H. Higher incidence of viable Mycobacterium leprae within the nerve as compared to skin among multibacillary leprosy patients released from multidrug therapy. Lepr. Rev. 68(1997)131-139.
19. Tajiri, I. Leprosy and childbirth. Int. J. Lepr. 4(1936)189-194.
20. Varner, M. W. Auto-immune disorders and pregnancy. Semin. Perinatol. 15(1991)238-250.
21. Wkgmann, T. G., Lin, H., Guilbert, L. and Mosmann, T. R. Bidirectional cytokine interactions in the maternal-fetal relationship: is successful pregnancy a TH2 phenomenon? Immunol. Today 14(1993)353-356.
1. M.D., M.R.C.P., London School of Hygiene and Tropical Medicine, Keppel Street, London WC1E 7HT and Hospital for Tropical Diseases, 4 St. Pancras Way, London NW1 OPE, United Kingdom.
2. M.B.B.S., Bhi-Nimwas, Salimpur Ahra, Patna 800 003, India.
Received for publication on 24 April 1998.
Accepted for publication in revised form on 12 November 1998.