- Volume 67 , Number 2
- Page: 150–3
Review of leprosy control activities in yemen
ABSTRACT
Leprosy control activities in Yemen are reviewed historically and up to the present time. Since 1983 the World Health Organization's multidrug therapy has been used in the National Leprosy Control Programme. Current activities are carried out in 63 leprosy clinics distributed all over the country and staffed by trained primary health care workers and medical assistants. In Yemen leprosy prevalence has declined f rom 1400 per 10,000 population in 1990 to 647 in 1997. Over the same period, new case detection rates per 10,000 population increased f rom 185 to 517. A backlog of leprosy cases continues to transmit the disease in Yemen.RÉSUMÉ
Nous avons revu les actions passées et présentes de lutte contre la lèpre au Yémen. Depuis 1983, la polychimiothérapie recommendée par l'Organisation Mondiale de la Santé est utilisée dans le cadre du Programme national de lutte contre la lèpre. Actuellement, les actions de luttes sont effectuées dans 63 cliniques spécialisées réparties dans tous le pays, avec un personnel médical entrainé et des assistants médicaux. Au Yémen, la prevalence de la lèpre a décliné de 1400 pour 10 000 habitants en 1990 à 647 en 1997. Pendant le même laps de temps, le taux de détection de nouveaux cas pour 10 000 habitants a augmenté de 185 à 517. Un groupe occulte de cas de lèpre continue de propager la maladie au Yémen.RESUMEN
Se hace una revisión histórica sobre las actividades del programa de control contra la lepra en Yemen. Desde 1983 se usa la poliquimioterapia sugerida por la Organización Mundial de la Salud para el control de la enfermedad y las actividades dei programa se llevan a cabo actualmente en 63 clínicas distribuídas en todo el Pais y en ellas participan tanto el personal médico calilicado como sus asistentes. En Yemen, la prevalência de la lepra ha disminuido de 1400 por 10 000 habitantes en 1990, a 64 por 10 000 en 1997. En el mismo periodo, la detección de casos nuevos aumentó de 185 a 517. Seguramente algunos de los casos antiguos de lepra continúan transmitiendo la enfermedad en Yemen.Before 1923, Dr. J. C. Young, head of the Keith Falconer (Scotland) Mission, established a leprosy ward as a branch of the Mission hospital at Sheikh Othman, Aden. This ward was reorganized in 1923, and in 1926 leprosy work was established as a branch of the Aden settlement of infectious diseases hospital (10). In 1932 the Mission undertook the leprosy work and a new leprosy hospital was opened accommodating 25 patients O in which leprosy patients were treated with sodium hydnocarpate (Alepol) and chaulmoogra oil. This hospital continued working until the early 1940s (9). In 1956 an organized outpatient leprosy control activity started in Aden, during which time the patients were treated with dapsone/DDS (Avlosulfone) twice a week for 2 years. At this time, clinics in Aden, Sana'a, Taiz and Mukalla were the only places which provided basic medical care for leprosy patients (5).
Before 1964, leprosy patients were isolated and kept in unsanitary houses (1). Between 1964 and 1973, Taiz and Mukalla were the only places known for giving organized medical care to leprosy patients, treating them with dapsone monotherapy. From 1973, leprosy work was carried out by the Missionaries of Charity in Taiz, Hodeidah and Al-Suknah. These activities were later taken over by the government. Until 1974, all patients were given dapsone monotherapy treatment (2). Later on rifampin was added daily for the first 3 to 6 months. From 1983 multidrug therapy (MDT) as recommended by the World Health Organization (WHO) was officially adopted by the National Leprosy Control Programme (NLCP) (8 and Al-Qubati, Y. Together for elimination of leprosy. 1993 Arabic manual).
In 1989 an agreement between the Yemen Ministry of Public Health (MOPH) and the German Leprosy Relief Association (GLRA) was signed to strengthen the activities of the NLCP This led to greatly improved control efforts. A pilot program was started in 1990 to serve the total population of 5,119,960 in Dhamar, Taiz, Ibb and Hodeidah (3). In the following years the NLCP activities were extended to the rest of the country.
In 1992, a local nongovernment organization called the Yemen Leprosy Elimination Society (YELEP) was established to support and maintain the activities of the NLCP (Al-Qubati, Y. Together for elimination of leprosy. 1993 Arabic manual).
MATERIALS AND METHODS
The NLCP activities are now carried out in 63 leprosy clinics distributed all over the country. These clinics are run by primary health care workers (PHCWs) and/or medical assistants (MAs) who were trained at the NLCP headquarters. They suspect the leprosy cases, refer them to the supervisors who visit the clinics on regular pre-scheduled dates, hold the patient cards and give health education to the patients and their families. To keep them motivated, incentives are given to them by the NLCP for each activity such as case finding, case holding, release from treatment and defaulter retrieval. Monthly supervision is carried out by the dermatologists appointed at NLCP headquarters in Taiz. These dermatologists are especially trained in leprosy at the NLCP headquarters and at ALERT in Ethiopia and the Schieffelin Leprosy Research and Training Center in Karigiri, India. During their supervision, they confirm the diagnosis of cases suspected by the PHCWs and MAs, check the regularity of treatment, revise records, prescribe orthopedic shoes for deformed patients, train PHCWs and MAs for MDT services, and give health education to leprosy patients.
Mass community surveys to study the problem of leprosy have been very difficult to make due to many reasons. The most important factor is the high cost of such surveys competing with other priorities within the Yemen MOPH. The second most important reason is the fact that leprosy patients are self-selected groups, not representing the whole population (J). Population-based studies to determine the epidemiological indicators of leprosy have not yet been conducted in Yemen. Therefore, we were forced to rely on the information collected by the NLCP over the past 8 years, and we also reviewed the NLCP supervision reports, cards and registers from 1990 to 1997.
RESULTS AND DISCUSSION
In Yemen leprosy declined from a peak of 1400 cases with a prevalence rate of 1.1 per 10,000 population in 1990 to 647 cases with a prevalence rate of 0.37 at the end of 1997 (The Table, Fig. 1). In most endemic countries similar declines in prevalence were observed with the number of countries showing prevalence rates above 1 case per 10,000 population having been reduced from 122 in 1985 to only 55 at the beginning of 1997 (11)• The decline in the prevalence trend was related to the increased activity of the control programs in Yemen as well as in other countries. The period of MDT is fixed for 2 years for MB cases and 6 months for PB cases during the review period. However, the registered prevalence rate had been found to be high in some governorates such as Al-Mahara, Hadramout and Shebwa (Fig. 2), which have special geographic, economic and social situations, and in which MDT services were poor until 1996 when it was initiated by a WHO Special Action Programme for the Elimination of Leprosy (SAPEL).
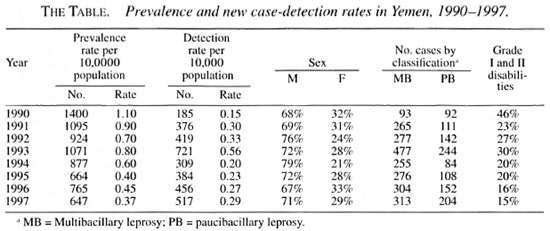
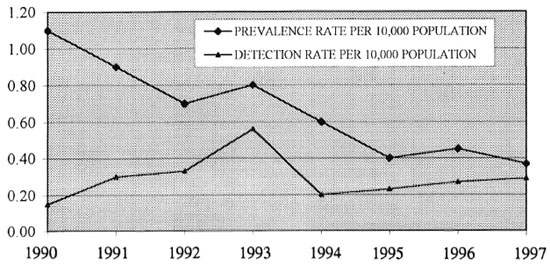
Fig 1. Prevalence and new case-detection rates in Yemen, 1990-1997.
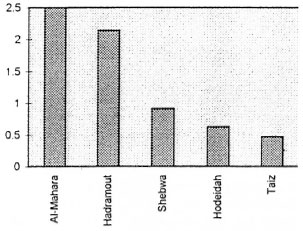
Fig . 2. Leprosy prevalence rates in Yemen at the end of 1997.
A gradual increase in the annual new case detection rate has been seen during the last 8 years (The Table, Fig. 1) with a peak of new cases detected in 1993. This resulted from the extension of the NLCP to five new governorates after the unification of Yemen. Other factors affecting the increase in the annual detection rate was the increased motivation of field workers through special
programs jointly executed by GLRA, YELEP, and the WHO, which led to the increase of MDT coverage geographically until it reached uncovered or poorly covered difficult remote areas in the desert of the empty quarter or in high mountains with many deep wadies. Unfortunately, most of these new cases had Grade II deformities because they had acquired the disease several years before they were detected, due to their living in difficult outreach areas with a lack of knowledge about the disease, social stigma and the uneven distribution of-health services. It is now expected that the number of new cases will probably remain at the same level for a few years to come until the effect of MDT is expected to halt the transmission of the disease. This is also expected in many endemic countries (l2).
The gender distribution of leprosy patients showed that 72% are males and 28% are females (The Table). This is a bit higher than the sex distribution in most parts of the world, where male preponderance is often observed at the rate of 2:1 (8). Our figures could be explained in two ways: a) the relative lack of women may have resulted from the fact that medical examination of women in Yemen is incomplete and less satisfactory due to social behavior and women have less chance for health services, and b) other factors with perhaps a true effect are religious restriction of free mobility of females and the wearing of a veil which could result in less exposure to the infection. Males, in general, are exposed to greater risks of infection as a result of their more exposed life style (8).
To simplify the classification of leprosy, we adopted the WHO classification of MB and PB, according to the number of the lesions and nerves involved, as ascertained from the patients' individual records. These data revealed that the proportion of MB cases was 66.3% and PB cases, 33.7%, i.e., 2:1 (The Table).
It was noted that the Grade I and II disabilities collectively equaled 46% in 1990 and then decreased gradually to 14.9% in 1997 (The Table). These percentages clearly indicate the importance of field control activities which include case finding, case holding and health education at the community and individual levels which were very effective in early case detection and the prevention of any leprosy complications.
The distribution of total cumulative new cases for each governorate between 1992 and 1997 showed that the three major governorates, with a high case load were Taiz (31%), Hadramout (24%) and Hodeidah (21%). The high case load in these governorates, and especially in Taiz (where the NLCP headquarters is located), is due to the fact that these governorates have a better health infrastructure and that cases in the surrounding governorates preferred to seek medical care in these governorates, sometimes to escape the social stigma attached to the disease in their communities.
CONCLUSION
A backlog of leprosy cases will continue to supply the pool of leprosy with new cases and to reactivate the transmission of the disease. Without field control activities and good health education programs the prevalence of leprosy will continue at a high level in Yemen.
REFERENCES
1. Al-Qubati, Y. Leprosy in Yemen. World Health 49(1996)18-19.
2. Al-Qubati, Y. and Al-Kubati, A. S. Dermatologists combat leprosy in Yemen. Int. J. Dermatol. 36(1997)920-922.
3. Al-Qubati, Y. and Al-Nabiiani, M. G. Formulation of a new leprosy control program in Republic of Yemen as a cooperation between GLRA and MOPH. (Abstract) Int. J. Lepr. 61(1993)45A.
4. Bryceson, A. and Pfaltzgraff, R. E. Leprosy . Edinburgh: Churchill Livingstone, 1990, p. 203.
5. Fawdry. A. L. Notes on leprosy in Aden. Lepr. Rev. 30(1959)114-117.
6. Global evaluation of the introduction of multidrug therapy (MDT). Lepr. Epidemiol. Bull. 4(1990)1-57.
7. Jakkman, P. and Smith, W. C. S. Evaluation of a multidrug therapy programme of leprosy control. Lepr. Rev. 65( 1994)289-296.
8. Noordeen, S. K. The epidemiology of leprosy. In: Leprosy . Hastings, R. C., ed. Edinburgh: Churchill Livingstone, 1985, pp. 15-28.
9. PETRIE, P. W. R. Leprosy work in Aden settlement. Lepr. Rev. 5(1934) 11-12.
10. Phipson, E. S. Aden and its leprosy problem. Lepr. Rev. 5(1934)4-10.
11. WHO Action Programme for the Elimination of Leprosy. Status report updated. Geneva: World Health Organization, 1997. WHO/LEP/97.4.
12. WHO Study Group. Epidemiology of leprosy in relation to control. Geneva: World Health Organization, 1985. Tech. Rep. Ser. 716.
1. M.Sc., Director; National Leprosy Elimination Progranune, P. O. Box 55722, Taiz, Republic of Yemmn. FAX 967-4-224019; e mail nlep@y.net.ye
2. National Leprosy Elimination Progranune, P. O. Box 55722, Taiz, Republic of Yemmn. FAX 967-4-224019; e mail nlep@y.net.ye
Received for publication on 8 July 1998.
Accepted for publication in revised form on 23 March 1999.