- Volume 67 , Number 3
- Page: 237–42
Comparison of two methods of leprosy case finding in the circle of kita in mali
ABSTRACT
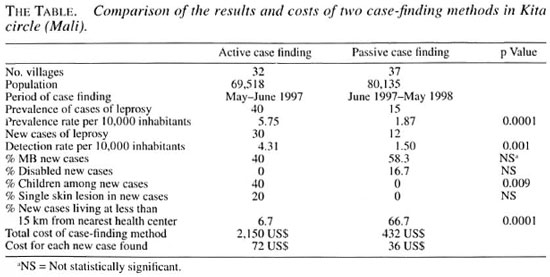
Kita is a health district of Mali, a leprosy-endemic country in West Africa. We conducted a comparative study of passive and active case finding of leprosy in this district in 1997. In May and June, a mobile team realized active case finding by visiting 32 villages of more than 1000 inhabitants. For 12 months, peripheral health center nurses did passive detection after information and education sessions about the signs of leprosy in the other 37 main villages of Kita. The active detection rate (4.31 per 10,000) was threefold higher than the passive rate (1.5 per 10,000) and allowed us to find earlier cases of leprosy. Active case finding identified children and single-lesion disease; the passive method did not. Cost for finding a new case was estimated at 72 US$ by mobile team detection and 36 US$ by passive case finding. Although the active method looked more expensive than the passive one, it was the only effective strategy to detect leprosy patients in remote and difficult-to-access areas. Based upon the results of the study, a flow chart is proposed for the choice of case-finding method when designing a leprosy elimination program.
RÉSUMÉ
Le district de Kita est une zone de santé du Mali, un pays où la lèpre est endémique en Afrique de l'Ouest. Dans ce district, nous avaons mené en 1997 une étude comparative de détection de nouveaux cas de lèpre, l'une passive et l'autre active. Durant les mois de mai et de juin, une équipe mobile a recherché activement les cas en visitant 32 villages de plus de 1000 habitants. Pendant 12 mois, de infirmières de centres de soins périphériques á la région ont réalisé une détection passive de nouveau cas après avoir mené des sessions d'infomration sur les signes de la lèpre dans 37 autres villages principaux du district de Kita. Le taux de détection par la méthode active (4,31 per 10 000) a été trois fois plus élevé que le taux obtenu par la méthode passive (1,5 pour 10 000) et nous a permis de trouver des cas plus précoces de lèpre. Le coût pour trouver un nouveau cas a été estimé à 72 SUS pour l'équipe mobile de détection et à 36 $US pour la détection passive de nouveaux cas. Bien que la méthode active ait semblé plus chère que la méthode passive, la première est la seule qui puisse efficacement détecter les patients souffrant de lèpre dans les zones reculées et difficiles à atteindre. Basé sur les résultats de cette étude, un organigramme est proposé pour aider au choix de la méthode de détection lors de l'élaboration d'un programme d'élimination de la lèpre.RESUMEN
Kita es un distrito de Mali, un pals con lepra endêmica del Africa occidental. En este distrito, en 1997 se hizo un estúdio comparativo sobre la detec- ción pasiva y activa de nuevos casos de lepra. En mayo y junio, un equipo móvil realizo la detección activa de casos visitando 32 poblaciones de más de 1000 habitantes. Durante 12 meses, enfemeras de centros de salud periféricos realizaron Ia detección pasiva de casos después de varias sesiones informativas y educa- cionales sobre los signos de la lepra, en ontras 37 poblaciones de Kita. La tasa de detección activa de casos (4.31 pr 10,000) fue 3 veces más alta que la tasa de detección pasiva (1.2 por 10,000) y permitió encontrar los casos de manera más temprana. El costo para el hal- lazgo de un nuevo caso fue de 72 dólares americanos en la detección activa y de $36 en la detección pasiva. Aunque el método activo resultó más costoso que el pasivo, fue la única manera efectiva de detección de casos en regiones remotas y de difícil acceso. Basados en estos resultados se propone un diagrama de flujos para escoger el método de detección de casos cuando se disena un programa de eliminación de la lepra.Leprosy is still an endemic disease in the member states of the Organisation pour la lutte contre les Grand Endemics (OCCGE), with a prevalence rate of 1.45 per 10,000 inhabitants in December 1996 (*). OCCGE, the coordination and cooperation organization for the control of major endemics, covers eight French-speaking countries of West Africa, including Mali. In Mali, a national leprosy control program (NLCP) has been carried out since 1992 (5). This NLCP, using the World Health Organization's recommended multidrug therapy (WHO/MDT), treated about 15,000 leprosy patients between 1992 and 1996. The WHO/MDT coverage rate reached 90% of registered cases in 1996. The prevalence rate of leprosy fell from 18.48 to 3.57 per 10,000 inhabitants during 1992-1996. Nevertheless, the detection rate remained at almost the same level, ranging between 1.37 and 2.11 per 10,000 inhabitants (5,6).
Meanwhile, in the countries of Benin and Burkina Faso, other member states of the OCCGE, active case finding of leprosy was set up in some areas (1,9). This resulted in a two- or threefold increase in the detection rate. So, we thought that the same level of the detection rate in Mali could be attributed to the passive case finding done through the NLCP. The poor effectiveness of that case-finding method could result in a constant and low detection rate. Mass campaigns for detection and treatment of leprosy patients during the dapsone monotherapy period (1960-1975) have been abandoned (7) because they were not cost effective and were opposite to the integration of leprosy control into the peripheral health services.
In 1997, we decided to carry out a comparative study of the passive and active methods of leprosy case finding. Our objectives were to measure the costs and results of these strategies and to propose recommendations to the OCCGE member states for the elimination of leprosy.
MATERIALS AND METHODS
Our study was a survey comparing the detection rates of two case-finding methods (passive and active). We estimated the detection rate with the passive case finding method at 1 case per 10,000 inhabitants and the detection rate with the active method at 4 cases per 10,000 population. The sample size for each method, in a one-tailed comparison test of two proportions and equal groups with an a risk of 5% and a power (1 - β) of 90%, would reach 65,000 persons.
We chose the Circle of Kita to carry out our study. Kita is a health district in the south of Mali. Total population of the Circle was about 274,000 inhabitants. We involved all villages of more than 1000 inhabitants in our survey. The villages were randomly separated into two groups. The passive detection method was allocated to a group of 37 villages with a total of 80,135 inhabitants. The active detection method was carried out in a group of 32 villages with 69,518 inhabitants.
The passive case-finding method consisted of: a) health education sessions about leprosy signs presented in villages by the nearest health center nurses; b) counselling of people with suspect signs of leprosy, referring them to the peripheral health center; c) examination of suspicious cases by nurses at the peripheral level of the health system; and d) confirmation of the leprosy diagnosis by a nurse specialized in leprosy at the district level.
The active case-finding method consisted of: a) health eduction sessions about leprosy signs presented in villages by a mobile team composed of a doctor and two nurses; b) nurse's examination of suspicious cases of leprosy immediately after the education session; and c) confirmation of the leprosy diagnosis by the mobile team doctor.
The WHO definition of a case of leprosy (a person with clinical signs of leprosy and requiring MDT) was used ("). A case of leprosy actively found was a person confirmed to be leprous after examination in his village by the mobile team members. A case of leprosy passively found was a person living in a village of the passive case- finding group and diagnosed as a leprosy patient in a health center during the 12 months following the education session.
The mobile team visited by car the 32 villages of the active case-finding group in May and June 1997. Nurses presented education sessions about the signs of leprosy in the 37 villages of the passive case-finding method during May 1997. Passive detection of cases was carried out in peripheral health centers from June 1997 to May 1998. Information on leprosy cases actively or passively found was written on questionnaires, and the data collected were analyzed with Epi-Info software. To estimate the costs of each method, we took account of the costs for the transportation of the mobile team by car and per diem of the team members during May and June 1997. For passive detection, we only took account of the costs of the nurses' trips by motorcycle to the villages of passive detection for the health education sessions.
RESULTS
Active case-finding results and costs. In the 32 villages with 69,518 inhabitants, the mobile team found 40 cases of leprosy. Four of them were already on MDT, 36 were requiring treatment and 30 were new cases of leprosy never treated before. There was no disabled patient among the new cases. Multibacillary (MB) patients were 40% of the new cases and children (less than 15 years old) also represented 40% of the new cases. Six patients (20% of new cases) had a single skin lesion; 93.3% of the new cases were living in villages more than 15 km from the nearest health center. The detection rate was 4.31 per 10,000 inhabitants and the costs to find a new case were estimated at 72 US$.
Passive case-finding results and costs. In the 37 villages with 80,135 inhabitants, peripheral health center nurses found 15 cases of leprosy between June 1997 and May 1998. Twelve of them were new cases of leprosy and the detection rate was 1.5 per 10,000 inhabitants. The percentages of MB leprosy and disabled cases were, respectively, 58.3% and 16.7%. There was no child or single lesion patient among the new cases of leprosy passively found. Passive case-finding costs were about 36 US$ per patient; 66.7% of the cases were living in villages less than 15 km from the closest health center (The Table).
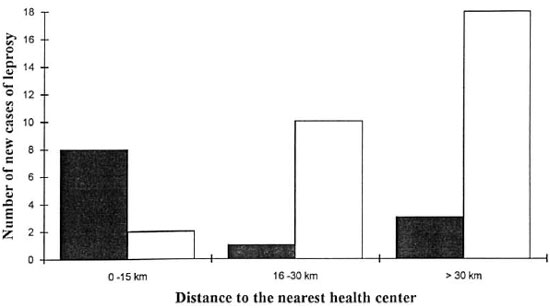
Fig. 1. Number of new cases of leprosy actively and passively found according to distance from closest health center.  = passive case Finding;
= passive case Finding;  = active case finding.
= active case finding.
Comparison of results and costs of the two methods. Comparing the results of the two methods, indicators showed that active case finding found earlier cases of leprosy with no disabilities, fewer MB patients and more cases among children. Active detection appeared more efficient, with a detection rate higher than the passive detection rate (p <0.001). Active case-finding allowed us to detect cases in remote areas; the proportion of new cases living near health centers was higher with the passive method and the difference with the active method was statistically significant (p <0.0001) (Fig. 1).
Active case finding looked more expensive than passive case finding. Nevertheless, it was a faster method of case finding, allowing the detection of more cases in 1 month than the passive method found in 12 months. Elsewhere, unlike the passive detection, the histogram of actively found new cases by age showed two spikes (nine new cases at 10-14 years and nine new cases at 35-39 years) (Fig. 2). Those spikes correspond to the ages of great incidence in leprosy classically described in the natural history of the disease (2-4).
DISCUSSION
The active detection rate was 2.5-fold higher than the national detection rate in Mali in 1997 (*). The effectiveness of the active case finding of leprosy by a mobile team confirms the findings of othei studies done in Benin and Burkina Faso (1,9). It also confirms the effectiveness of the leprosy elimination campaigns (LEC) supported by WHO in Madagascar and Guinea in West Africa. Leprosy at its beginning is a painless disease and its skin lesions do not make people go for a medical examination. This is particularly true when the health center is far from villages. In our survey, we found that less than 25% of passively found new cases came from areas more than 30 km from a health center. In a village 60 km from the nearest health center, we actively detected 15 new cases of leprosy. None of them had tried to travel to the health center for a medical visit. We think that when the distances between villages and health center are more than 15 km, only active case finding detects new cases of leprosy.
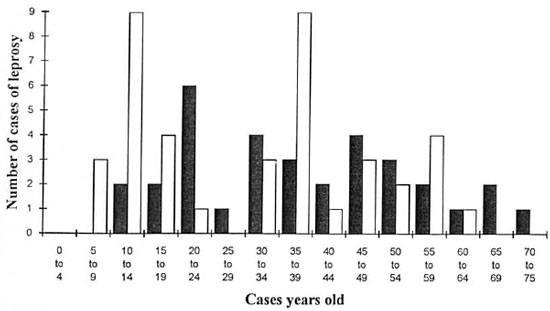
Fig. 2. Number of cases of leprosy actively and passively found according to age.  = passive case finding;
= passive case finding;  = active case linding.
= active case linding.
An advantage of active case finding of leprosy is earlier detection, with more pau- cibacillary (PB) cases requiring short treatment and more single-lesion cases that can be treated by a single dose of rifampin- ofloxacin-monocycline (ROM). An earlier active detection also prevents the occurrence of disabilities and leprosy reactions. These advantages could compensate for the more expensive active case finding compared to the passive method. For better cost-effectiveness of active case finding, this method could be applied in remote or difficult-to-access areas and only repeated every 2 or 3 years rather than yearly.
A criticism of active case finding in leprosy is based on the risk of intake of self- healing cases. These self-healing cases- indeterminate form of leprosy-could lead to an overdiagnosis of new cases. However, the safety of current treatments of leprosy with WHO/MDT (10) makes acceptable that overdiagnosis. It is better to overdiagnose some self-healing cases than to have a few patients become disabled.
Passive detection of leprosy is a better strategy for health services integration. It could easily be combined with other components of primary health care (extend program of immunization, tuberculosis control program, etc.). For a better quality of leprosy diagnosis and considering the mobility of health staff at the peripheral level, passive detection requires a program of training and retraining of nurses and permanent supervision of the peripheral health staff at the district level. To be efficient, passive detection should be preceded by information and education campaigns about the signs of leprosy. When considering the costs of information campaigns, training, retraining and supervision activities, the low cost of passive case finding could reach the cost of active case finding.
The costs, advantages and inconveniences of each method made us propose a flow chart for the choice of a case-finding method (Fig. 3). This chart is based upon the prevalence rate of leprosy, MDT coverage, and the average radius of the attraction circle of each peripheral health center. We proposed the flow chart to the NLCP managers of each member state of the OCCGE and hope that it could be used in setting plans for the elimination of leprosy.
CONCLUSION
Our comparative study of two methods of case finding in leprosy showed that active detection is more efficient, allowing treatment of earlier cases of leprosy and the prevention of disabilities. The more expen sive active method could be compensated by carrying out active case finding in only remote and isolated areas and repeating these activities at intervals of 2 or 3 years, according to the prevalence of leprosy. Passive detection of leprosy cases should be accompanied by education sessions. For the elimination of leprosy, the two case finding strategies should be combined in most countries endemic for leprosy.
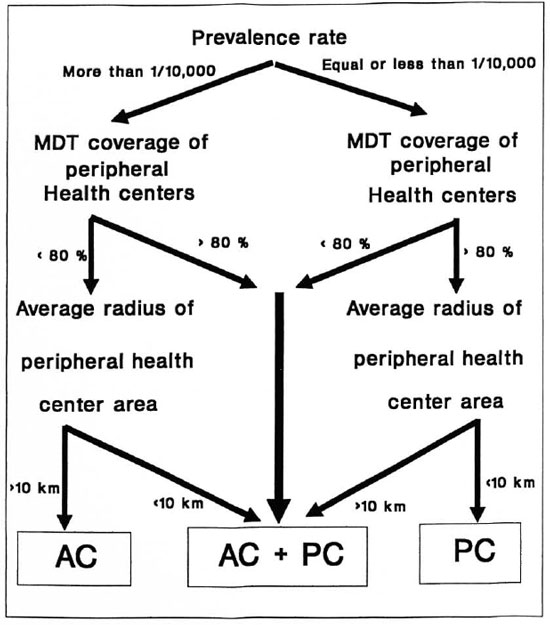
Fig. 3. Proposed flow chart for choosing a leprosy case-finding method in integrated health systems. AC = active case finding; AC + PC = combined active and passive case finding; PC = passive case finding.
Acknowledgment. This study received financial support from the Francophone Research Fund (FFR) through the Associated Francophone Laboratory no. 304 of AUPELF-UREF. We gratefully acknowledge the FFR and the peripheral and district health staff of Kita Circle in Mali who made this study possible.
REFERENCES
1. Guedenon, A., Anac.onou, S., Ahouandogbo, F., Foundohou, J., Chabot, M. and Josse, R. Evolution of the leprosy endemicity in Benin (19821992). (Abstract) Int. J. Lepr. 61 (Suppl.) (1993) 63A.
2. Jeanselme, E. La Lèpre. Paris: Donin, 1934.
3. Languillon, J. Précis de Leprologie. Paris: Masson, 1986.
4. Sansarricq, H. La Lèpre. Paris: AUPELF- UREF/EUipses, 1995.
5. Tiendrebéogo, A., Blanc, L. and the Eight Leprosy Programme National Managers of Member States of OCCGE. MDT for leprosy in 8 francophone countries of West Africa; ten years' implementation. (Abstract) Int. J. Lepr. 61 (Suppl.) (1993) 43A.
6. Tiendrebéogo, A., Guedenon, A., Zerbo, P.-J., Djakeaux, S., Berthé, A., Benani, Y. C., Souley, K., Sylla, P. M. and Tignokpa, N. Lèpre et lutte antilépreuse en 1994 dans les huit pays membres de l'OCCGE. Med. Afr. Noire 43 (1996) 107-111.
7. Tiendrebéogo, A., Keita, F., Timite, B. and the National Leprosy Control Managers of OCCGE Member States. Evolution de la lèpre dans les pays membres de l'OCCGE entre 1960 et 1993 (étude comparative de cartes épidémiologiques). OCCGE Info. 102-103 (1995) 10-16.
8. Tiendrebéogo, A. and National Leprosy Control Programme Managers of OCCGE Member States. Lèpre et lutte antilépreuse dans les 8 pays membres de l'OCCGE de 1935 a 1997. (Abstract) Int. J. Lepr. 66 (1998) 59A.
9. Tiendrebéogo, A., Sow, O. S., Dembei.eî, S. M., Sawadogo, O., Ouédraogo, K., Bidé, L. and Millan, J. Evaluation de l'élimination de la lèpre au Burkina Faso. Acta Leprol. 11 (1998) 7-16.
10. World Health Organization. A guide to eliminating leprosy as a public health problem. Geneva: World Health Organization, 1995. WHO/LEP/95.1.
11. World Health Organization. A guide to leprosy control. Geneva: World Health Organization, 1989.
1. M.P.H.; Observatoire de la Lèpre en Afrique, P.O. Box 251, Bamako, Mali.
2. M.D., Observatoire de la Lèpre en Afrique, P.O. Box 251, Bamako, Mali.
3. M.D., Institut Marchoux, P.O. Box 251, Bamako, Mali.
4. M.D.; District Health Center, Kita, Mali.
5. M.D., District Health Center, Kita, Mali.
Reprint requests to A. Tiendrebéogo at the above address or FAX: 223-22-95-44.
Received for publication on 22 March 1999.
Accepted for publication on 16 June 1999.