- Volume 67 , Number 2
- Page: 175–6
Histoid leprosy; report of three cases
To the Editor:
Histoid leprosy, originally described by Wade in 1960, is regarded as a distinct clinico-pathological entity, presenting as cutaneous or subcutaneous nodular- and/or plaque-like lesions arising from apparently normal skin and characterized histologically by tumorous collections of spindle- shaped cells arranged in criss-cross fashion, giving them a resemblance to neurofibromatosis (1).
CASE REPORTS
The three cases of histoid leprosy seen within 1 year were: a 25-year-old housewife (Case 1), a 28-year-old daily wage worker practicing earpiercing (Case 2), and a sugarcane cutter 32 years of age (Case 3). All three cases were of low socioeconomic status without any family history of Hansen's disease among close relatives or in their immediate neighborhoods. Cases 2 and 3 were from the Beed District of the state of Maharashtra, India, an area endemic for leprosy. None of the three patients had received any form of treatment for their disease when first seen. The durations of their symptoms were 6 months, 3 months and 2 months, respectively.
All three patients presented with asymptomatic, firm, well-defined, ½ cm to ½ cm, erythematous-to-skin-colored, oval-to- round, shiny papulonodules over the pinnae, forehead, face, neck, trunk and extremities (Fig. 1). A few nodules were subcutaneous in location while the majority were cutaneous. In addition, Case 3 showed lesions over the scrotum and glans including around the external urethral opening (Fig. 2), a very rare site for leprosy lesions. Associated features of lepromatous leprosy, including multiple peripheral nerve thickening and patchy glove-and-stocking anesthesia, were present. However, none of these three cases showed trophic ulcers or madarosis.
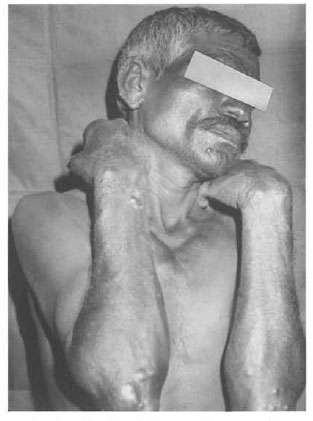
Fig. 1. Histoid nodules over the pinna, elhows
and forearms in Case 2.
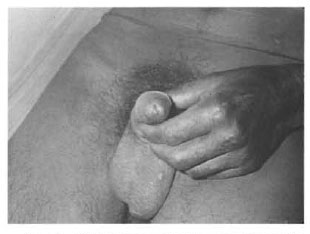
Fig 2. Nodules over the glans and serotum in Case 3.
Systemic examination of the three cases revealed no abnormalities. Routine blood and urinalysis, liver and renal function tests, blood VDRL and ELISA for HIV were all negative. Slit-skin smears from the nodules in all patients showed a bacterial index (BI) of 6+ (Ridley scale), and histopathology was consistent with the diagnosis of histoid leprosy with a thinned out epidermis, nodular infiltrate of spindle- shaped histiocytes arranged in whorls, and innumerable acid-fast bacilli found on Fite-Faraco staining.
All three patients were given multidrug therapy (MDT) recommended by the World Health Organization composed of once- monthly supervised 600 mg rifampin and 300 mg clofazimine orally, followed by daily 100 mg dapsone and 50 mg clofazimine. All three patients responded well to treatment with uneventful progress and a fall in their Bis, except for Case 2 who suddenly went into recurrent type 2 reaction after successful completion of 1 ½ years of MDT. He has been subsequently put on once-monthly 400 mg ofloxacin, 200 mg minocycline, and 500 mg clarithromycin along with nonsteroidal antiinflammatory drugs and tapering doses of oral steroids to control his reaction.
DISCUSSION
The term "histoid" was introduced because the condition resembles a tumor developing from spindle-shaped histiocytic elements. It closely resembles dermatofibroma and other histiocytic and fibrotic skin tumors (4). Although histoid leprosy is considered to be a forme fruste of leproma- tous leprosy, the salient clinical features that distinguish it from classical leproma- tous leprosy are that the nodules, being expansile and noninfiltrative, arise from apparently normal skin and there is no madarosis. In one series on histoid leprosy with significant facial involvement, the ears and nasal mucosa showed little change and the larynx was spared (5).
The notable histopathological findings are the presence of spindle-shaped histiocytes in the dermal infiltrate arranged in intertwining and whorled patterns. They contain numerous bacilli and their cytoplasm may be slightly vacuolated but lacks the marked vacuolation seen in lepra cells. The bacilli are intact and rod-shaped in contrast to the fragmented forms seen in conventional lepromatous cases (4). Other features, such as epidermal atrophy and a free subepidermal zone, are seen in both ordinary lepromatous and histoid forms of leprosy (5).
Immunohistochemistry studies in histoid leprosy reveal that the numbers of dendritic epidermal cells, identified by monoclonal antibodies against CD1, HLA-DR, CD45 and CD36, were reduced in histoid leprosy compared to both tuberculoid and lepromatous groups. This supports a modified hypersensitivity reaction of the cellular type which results in an inhibition of the lesional expansion but not in the destruction of the bacilli within the histoid lesion (2). A study to evaluate the role of mast cells in the histopathogenesis showed proliferation of mast cells and their degranulation mainly in the histoid nodule, as compared to the surrounding normal healthy skin in which mast cells were intact (3).
Bhutani, et al . (1) found 20 cases of histoid leprosy among 280 cases of leprosy over 3 years. There were 14 females and six males with ages ranging from 22 to 84 years and duration of disease ranging from 3 months to more than 14 years. Our cases showed a similar sex ratio although our cases belonged to a younger age group with a shorter duration of illness. However, all of our cases started de novo as histoid lesions as compared to seven which developed de novo and 13 which developed histoid lesions 5 months to 14 years after the onset of leprosy (1). They were fresh cases without any prior treatment history as compared to the study by Bhutani, et al . which found that only 75% had never received prior treatment. Lesions, cutaneous as well as subcutaneous, are mainly present over the back, buttocks and face and are less seen over the extremities (1). However, our Case 3 had shiny, cutaneous, well-defined papulonodules over his genitalia, including the peri-urethral meatus, probably hitherto unreported in the literature.
- Kshiteendra Kewal Krishna, M.D.,
D.N.B. (Dermatology, Venereology and Leprology)
Practising Consultant in Dermatology, Venereology and Leprology
A/3, Amar Classic, Hadapsar
Pune 411028, Maharashtra, India
REFERENCES
1. Bhutani, L. K., Bedi, T. R., Malhotra, Y. K., Kandhari, K. C. and Deo, M. G. Histoid leprosy in North India. Int. J. Lepr. 42(1974)174-181.
2. Kontochristopoulos, G. J., Aroni, K.. Panteleos, D. N. and Tosca, A. D. Immunohistochemistry in histoid leprosy. Int. J. Dermatol. 34(1995)777-781.
3. Kumar, R. Mast cells in histoid lesions. Indian J. Lepr. 59(1987)390-392.
4. Mansfield, R. C. Histoid leprosy. Arch Pathol. 87(1969)580-585.
5. Ramesh, V., Misra, R. S., Kachhawa, D. and Kulkarni, S. B. Giant lesions in histoid leprosy. Int. J. Dermatol. 66(1998)232-234.
Reprint requests to Dr. K. Krishna, 23 Sopan Bang Cooperative Housing Society, Pune 411001, Maharashtra, India.