- Volume 67 , Number 3
- Page: 310–2
Single-dose treatment for paucibacillary leprosy; clinical problems and management
To the Editor:
The advent of short-course chemotherapy has brought on a revolution in the treatment of leprosy at the same time indicating the possibilities of saving considerable manpower and resources. A single dose of rifampin, ofloxacin and minocycline (ROM-1 ) is reported to be as effective as 6 months paucibacillary multidrug therapy (PB MDT) for single skin lesion PB (SSL- PB) leprosy cases. In our earlier reports, clinical problems after ROM-1 in SSL-PB leprosy (4) and in PB leprosy with two to three lesions (2) were reported.
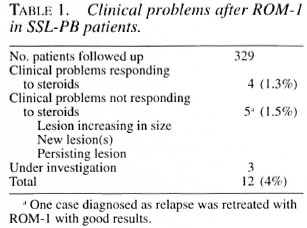
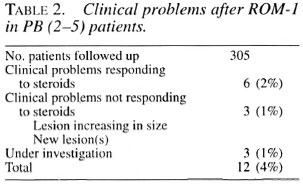
We present here our long-term observations on the clinical problems and events after ROM-1 in 329 SSL-PB patient (Table 1 ) and in 305 PB patients with 2 to 5 lesions [PB (2-5)] (Table 2). Efficacy of treatment was evaluated on the rate of clinical regression and occurrence of reaction and clinical events during follow up. Reappearance of the lesions in treated cases has profound implications for case management, disease transmission and control, in addition to the social factors. The feasibility and operational aspects are discussed separately elsewhere in this issue (1).
The patients were followed for a period of 42 months. Clinical problems encountered were of the following nature: 1) new lesions: 13 cases developed new lesions which were hypopigmcnted/erythematous in appearance, of small-to-moderate size and with hypoesthesia; 1 case had developed new hyperpigmented lesions and 3 had new nerve lesions; 2) increase in size of lesion/extension of lesion: 6 cases showed an increase in the size of the lesion which was marginal and anesthetic in nature; and 3) persistence of existing lesions: 5 cases had persistently raised erythematous lesions, 4 of whom continue to remain stationary. The phenomenon of delayed clearance of granuloma could be responsible for such clinical problems. Further follow up of these cases will help to confirm this phenomenon.
While considering the "clinical events," patients with type 1 reaction and neuritis who were managed in the conventional manner were excluded from the study.
Severity. Most of the clinical features observed in these cases were of mild-to- moderate nature.
Frequency. Clinical events were encountered over a period as early as 6 months after withdrawal of the treatment and delayed events were observed over a period of 42 months in both of the groups. One SSL-PB patient and two PB (2-5) patients had a recurrence of skin lesions despite a course of steroids.
Management. All of the patients with the clinical events described above were treated with a standard course of steroids (starting dose 40 mg daily) tapered gradually over a period of 5 to 6 months. Child patients were treated with a proportionate lesser dose. Four SSL-PB patients and 6 PB (2-5) patients responded satisfactorily while 8 (1.3%) cases who did not show satisfactory response and in whom the problems persisted were termed as "Clinical problems persisted." These patients have been kept under observation and are subjected to periodic clinical review. One patient among these eight cases with occurrence of a new lesion and no change in the initial lesion was diagnosed as a relapse. Since there was no response to a therapeutic trial with a standard course of steroids, the patient was retreated with the ROM-1 regimen 19 months after development of the new lesion. The clinical response after re-treatment was remarkable (Fig. 1).
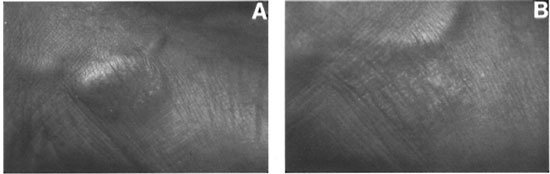
Fig. 1. Case 1. A = Betbre re-treatnent; B = 10 months after rc-treatmcnt with ROM-1.
A second patient who was treated with a standard course of steroids subsequently had to be put on only clofazimine in an anti-inflammatory dose in view of the raised and erythematous nature of the lesion on the face. Recently, this patient had to be given clofazimine and steroids together since the lesion was still raised and erythematous (Fig. 2). This patient is currently on clofazimine and steroids and is under observation.
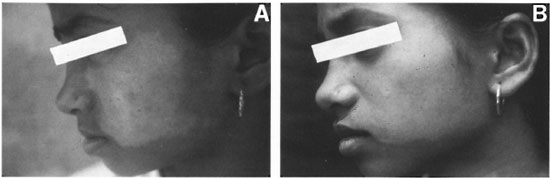
Fig. 2. Case 2. A = Showimg no response to steroids; B = presently on clofazimine and steroids.
Observations. These clinical events observed long after chemotherapy intervention seem to be arising as a result of immunological response to live bacilli or antigenic elements present cither in the skin or the nerves. Similar experiences have been encountered also in PB leprosy patients treated with conventional WHO-PB-MDT (5), which emphasizes the reasoning behind persisting antigens giving rise to such clinical events. The laboratory and immunological significance of the recurrence of skin and nerve lesions in ROM-1 treated cases and the lack of response in some of the cases to a standard course of steroids is a matter for research from a management point of view. The pathogenesis of such clinical events is not well understood. Whether these are true "relapses" remains to be seen and if so, they may need to be retreated with the ROM-1 regimen.
Out of the 24 cases who presented with clinical problems, 8 belonged to the adolescent age group, a group that is subjected to fluctuating hormonal levels of a physiological nature. The possibility of this phenomenon influencing the disease manifestation or such clinical problems needs to be investigated. The phenomenon of lesions on the face posing therapeutic difficulty also should be properly understood and answered. However, the management of the problem should be tackled in a rational manner without any empirical approach. Considering the nature of the clinical events in our experience, it appears that most of the events seem to be manageable. Their field implications arc discussed separately elsewhere in this issue (3).
- V. V. Pai
H. O. Bulchand
C. R. Revankar
R. Ganapati
Bombay Leprosy Project
Vidnyan Bhavan
11, V N Purav Marg
Sion-Chunabhatti
Mumbai 400 022, India
REFERENCE
1. Ganapati, R., Rkvankar, C. R., Pai, V. V. and Kinc.si i v, S. Single-dose treatment for paucibacil- lary leprosy; feasibility of long-term follow up. (Letter) Int. J. Lepr. 67(1999)308-309.
2. Pai, V. V., Rkvankak, C. R., Pai, R. R., Das M. and Ganapati, R. ROM single dose for PB leprosy with I to 3 lesions. (Abstract) Int. J. Lepr. 66(1998)2A.
3. Ri.vankak, C. R., Pai, V. V., Antony Samy, M. S. and Ganapati, R. Single-dose treatment for pau- cibacillary leprosy; field implications. (Letter) Int. J. Lepr. 67(1999)312-313.
4. Rkvankar, C. R., Pai, V. V., Bui.chano, II. O. and Ganapati, R. Delayed clinical problems in single lesion PB leprosy after single dose ROM. (Abstract) Int. J. Lepr. 66(1998)16A.
5. Sum y, V. P., Suchitra, K.. Upi.kkar, M. W. and Antia, N. H. Persistence of Mycobacterium leprae in the peripheral nerve as compared to the skin in multidrug treated leprosy patients. Lepr. Rev. 63(1992)329-336.