- Volume 67 , Number 3
- Page: 270–8
Risk factors for erythema nodosum leprosum
ABSTRACT
A retrospective study of new borderline lepromatous and lepromatous patients reporting for multidrug therapy (MDT) for leprosy at the Anandaban Leprosy Hospital, Kathmandu, Nepal, over an 8-year period was conducted to determine the prevalence of erythema nodosum leprosum (ENL), the time and frequency of reactions, and clinical and laboratory parameters associated with ENL. An overall prevalence of ENL in this cohort of 19% was found. One third of these reactions occurred in patients before MDT was given, one third in the first 6 months and one third after 6 months of treatment. Nearly 1 in 10 of the ENL reactions occurred in patients who had completed 2 years of MDT; 45% of patients with ENL had more than one episode. Data collected at the patients' first presentation was used to identify four major risk factors. Patients with lepromatous disease, skin infiltration or a bacterial index (BI) of >4+ were at significantly increased risk. Patients older than 40 were at significantly decreased risk of ENL. There was a linear relationship in the risk of ENL with an increasing BI and an inverse relationship to increasing age. These observations should enable clinicians to recognize patients at first presentation who will be likely to develop ENL.RÉSUMÉ
Une étude rétrospective des nouveaux cas souffrant de lèpre lépromateuse et borderline lépromateuse, se déclarant afin d'être traités par la poly-chimiothérapie (PCT) à l'hôpital Anandabane contre le lèpre à Katmandou au Népal, pendant une période de 8 années, fut effectuée afin de déterminer la prévalcnce de l'éry- thème noueux lépreux (ENL), la durée et la fréquence de ces réactions, et les paramètres cliniques et de laboratoire associés à l'ENL. Une prévalence générale de l'ENL dans cette cohort fut déterminée être de 19%. Un tiers de ces réactions se sont produites avant la mise en œuvre de la PCT, un tiers pendant les 6 premiers mois qui ont suivi le début du traitement et un tiers après les premiers 6 mois de traitement. Environ 1 sur 10 des réactions de ENL furent observées chez des patients qui étaient sous PCT depuis plus de deux années; 45% de ces paitents ayant des ENL eurent plus d'un épisode. Les données collectées durant la première consultation des patients furent analysées et permirent d'idenifier 4 facteurs de risque majeurs. Les patients avec maladie lépromateuse, infiltration cutanée ou un indice bactérioscopique (IB) de >4+ présentaient un risque d'ENL significativement plus élevé. Les patients âgés de plus de 40 ans avaient un risque significativement diminué de développer l'ENL. Il y avait une relation linéaire entre le risque de développer un ENL et un IB croissant et une relation inverse avec l'âge. Ces observations devraient permettront d'aider les cliniciens à reconnaître dès la première consultation les patients qui vont probablement développer l'ENL.RESUMEN
Se hizo un estudio retrospectivo de los casos nuevos de lepra leproniatosa y lepromatosa subpolar que fueron tratados con poliquimioterapia (PQT) en el Hospital Anandaban de Kathmandu, Nepal, a lo largo de un periodo de 8 anos, para determinar la prevalência de eritema nodoso leproso (ENL), el tiempo y la frecuencia de las reacciones y los parâmetros clínicos y de laboratorio asociados con ENL. Se encontro una prevalência global de NEL en este cohorte de 19%. Un tercio de estas reacciones ocurrieron en los pacientes antes de iniciar el tratamiento con PQT, un tercio en los primeros 6 meses de tratamiento, y un tercio des- pués de 6 meses de tratamiento. El 10% de las reacciones ENL ocurrieron en pacientes que habian completado 2 anos de tratamiento; 45% de los pacientes con ENL habian tenido más de un episodio reaccional. Los datos colectados de la primera entrevista con los pacientes se usaron para identificar los 4 factores de riesgo principales. Los pacientes con lepra lepromatosa y con indices bacterianos (BI) de >4+ fueron los de mayor riesgo. Los pacientes mayores de 40 anos fueron los de menor riesgo. La relación entre el riesgo de ENL y el incremento en el BI fue lineal pero la relación fue inversa entre el riesgo de ENL y la edad de los pacientes. Estas observaciones podrían permitir a los clínicos reconocer, en la primera entrevista, a los pacientes en riesgo de desarrollar ENL.Erythema nodosum leprosum (ENL) is an acute inflammatory condition affecting lepromatous leprosy patients. The condition is characterized by the appearance of multiple, tender, red, skin nodules accompanied to a variable extent by fever, edema, vasculitis, neuritis and iritis. The frequency of ENL appears to be lower in patients on multidrug therapy (MDT) compared with patients on dapsone monotherapy (3). This may be due to the antiinflammatory properties of clofazimine, which is particularly well absorbed into the skin, although it may also be that earlier treatment has reduced the proportion of highly smear-positive patients, and this may explain a decline in ENL prevalence.
ENL is an important clinical complication in leprosy which must be promptly and effectively treated. To recognize which patients are at high risk of developing this condition, we have used the pre-treatment clinical and laboratory data from more than 500 new patients to identify factors contributing to a high risk of ENL. Using these results, it is possible to set simple criteria at diagnosis for those patients who need to be monitored for ENL during and after their leprosy chemotherapy.
MATERIALS AND METHODS
We examined the hospital records of all 649 previously untreated borderline lepromatous (BL) and lepromatous (LL) cases registered as regular MDT patients between 1989 and 1997. Only patients who were regular attendees at the Anandaban Leprosy Hospital clinics were included.
All data were collected at the patients' first consultation. This included age, sex and clinical classification based on the Rid- ley-Jopling classification (7). Confirmation of clinical classification by histopathology was available in only a minority of cases. The number of years since the appearance of the first symptoms as reported by the patients was recorded as a measure of the length of the untreated disease. The cumulative disability index (DI) of each patient according to the World Health Organization (WHO) classification system (16) was also recorded. In addition, the number of body areas (BA) with disease were noted based on the number of BA with either skin patches or enlarged nerves. This was based on a scale with a maximum of 9, consisting of 4 for the trunk divided sagitally anterior and posterior, 4 for the limbs, and 1 for the head (13). The total number of patches, enlarged nerves, presence of skin infiltration and nodules were also recorded. The mean bacterial index (BI) was calculated from slit-skin smears taken from a minimum of four sites, including a clinical lesion. The morphological index (MI) was calculated as the percentage of solid-staining bacilli seen in 200 acid-fast bacilli (AFB). IgM anti- phenolic glycolipid-I (PGL-I) antibodies were measured as described previously (9).
Erythema nodosum leprosum (ENL) was defined clinically as the appearance of multiple tender or painful erythematous nodules in the skin accompanied by fever and malaise.
Statistics. The differences in the range of quantitative variables between different patient groups were tested by means of the Mann-Whitney U Test.
Chi-squared contingency tables were used to calculate the unadjusted odds ratios (OR) and the 95% confidence intervals (95% CI) for differences in the prevalence of ENL between patients with and those without individual clinical or laboratory parameters. The unadjusted OR and 95% CI for the differences in the prevalence of multiple episodes of ENL between patients with and without individual clinical or laboratory parameters were also calculated.
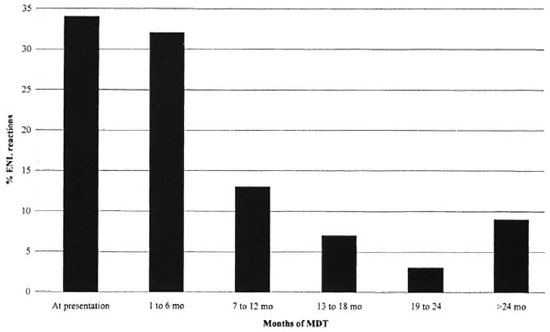
Fig. 1. Time of occurrence of ENL in 108 patients under MDT treatment.
Adjusted OR and 95% CI were calculated by logistic regression to assess the significance of individual factors. Only risk factors with unadjusted OR significantly more or less than 1.0 (except for age and sex) were included.
RESULTS
Of the 649 patients, 86 were excluded for reasons of defaulting, transfer to another center, or incorrect diagnosis or classification. The records of the remaining 563 patients were examined for baseline (i.e., at diagnosis) clinical, bacteriological and serological data as well as a history of ENL.
The 563 patients consisted of 422 (75%) male and 141 (25%) female patients with an age range of 3 to 85 years. There were 351 (62%) borderline lepromatous (BL) and 212 (38%) lepromatous (LL) patients. All the patients received WHO/MDT multi- bacillary (MB) treatment.
The patient group had an average of seven body areas with disease (range 1-9); among these were 273 (48%) patients who had disease in all nine body areas. The patient group had an average of four nerves enlarged (range 0-12); 535 (95%) patients had at least one enlarged nerve. Skin nodules and infiltration were present in 98 (17%) and 366 (65%) of the patients, respectively. Of patients with a disability grading at presentation, 305 (66%) had established disability (that is, a disability index greater than 0). Three-hundred-twenty- eight (58%) patients presented more than a year after the appearance of the clinical symptoms. Skin smears (BI) were positive in 470 (83%) patients, negative in 85 (15%), and not done in eight. The MI was positive in 89, negative in 168, and not done in 306 patients. PGL-I antibodies were positive in 320 (70%), negative in 135 (30%), and not done in 108 patients.
Among the 563 patients, 108 (19%) had an ENL reaction during the study period. Patients were self-referring outpatients and were generally admitted for treatment of the reaction. About 20% of ENL cases had neuritis and 5% had iritis. The severity of the ENL reaction varied and treatment was varied appropriately, with milder cases (about one-third) treated with nonsteroidal antiinflammatory drugs and those with more severe ENL or neuritis treated with steroids and/or thalidomide. There was an average of two episodes of ENL per patient: 49 (45%) patients had a single episode, 27 (25%) two, 13 (12%) three, 6 (5%) four, 2 (2%) five and 5 (5%) had more than 5 episodes of ENL.
Thirty-five (34%) of the ENL cases had no previous antileprosy treatment at the time of reaction; 34 (32%) had ENL reaction in the first 6 months of MDT, 14(13%) between 7 and 12 months after the beginning of MDT, 8 (7%) between 13 and 18 months of treatment, 3 (3%) between 19 and 24 months, and 10 (9%) after 2 years of MDT (Fig. 1).
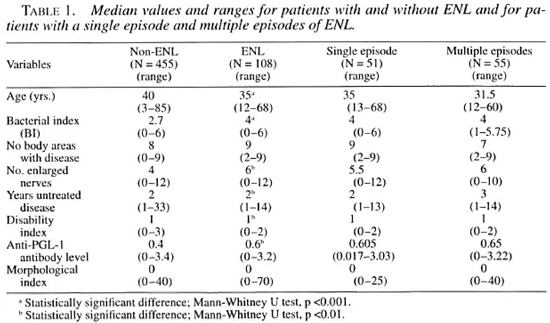
Table 1 shows median values of variables in patients with and without ENL and in patients who had single and multiple episodes of ENL. Patients who had ENL were significantly younger, had a higher BI, a higher level of anti-PGL-I antibodies, more enlarged nerves, longer periods of untreated disease and less established disability than did patients without ENL. There were no significant differences in the median values between patients with single episodes of ENL and those with multiple episodes of ENL. However, those who had multiple episodes of ENL were younger, had more enlarged nerves, and had a higher level of anti-PGL-I antibodies than did those who had only a single episode of ENL.
The differences in the prevalence of ENL according to the presence or absence of individual clinical or laboratory parameters were assessed (Table 2). LL patients had a significantly higher prevalence of ENL (33%) than did BL patients (11%, p <0.001).
Patients with a BI of >4+ had a significantly higher prevalence of ENL (32%) than did patients with a BI of <4+ (14%, p <0.001). Patients with more than five enlarged nerves had a significantly higher prevalence of ENL (27%) than did those with the number of enlarged nerves <5 (14%, p <0.001). Patients with skin nodules (21%) had a significantly higher prevalence of ENL than did those without nodules (13%, p <0.05). Patients with diffuse skin infiltration had a higher prevalence of ENL (26%) than did those without (6%, p <0.001). Patients who were IgM anti- PGL-I antibody positive (21%) were more likely to develop ENL than were those who were antibody negative (13%).
The prevalence of ENL was not significantly different between male and female patients, between patients older than 40, and those <40, between patients who had untreated disease for more than 1 year, and those who reported less than 1 year of untreated disease. It was also not significantly different between patients with established disability and those with a positive MI and those with a negative MI, nor between those with disease in all body areas and those with less diffuse disease.
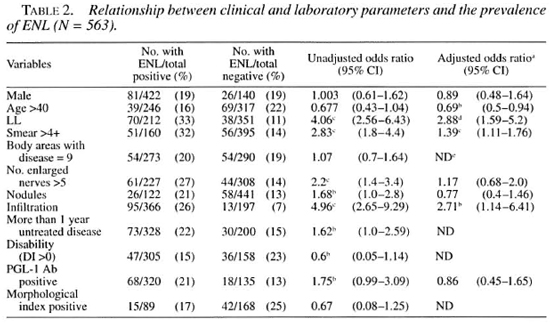
A clear association was found between the increasing BI and the prevalence of ENL (p <0.001) (Fig. 2). Likewise, there was a trend for the prevalence of ENL to decrease in older patients (Fig. 3), but this did not reach statistical significance.
Logistic regression analysis. The unadjusted OR suggested a significant effect of eight factors on the prevalence of ENL: a) an LL classification, b) a smear >4+, c) more than five enlarged nerves, d) the presence of nodules or e) infiltration, f) more than 1 year of untreated disease, g) the absence of disability, and h) seropositivity for anti-PGL-I antibodies (Table 2). Logistic regression was used to estimate the adjusted effect of each factor controlling for the significant confounding effects which we found to be present. Age greater than 40, an LL classification, a smear >4+, more than five enlarged nerves, the presence of nodules or infiltration, and anti-PGL-I antibody seropositivity were found to be significant confounders of each other and so were included in the logistic regression analysis. Other factors (body areas, length of untreated disease, disability and positive MI) which had nonsignificant unadjusted OR were excluded.
After adjustment, a significant increase in the risk of ENL is found for only three factors: LL classification (OR = 2.88), skin infiltration (OR = 2.71) and smear >4+ (OR = 1.39). Age greater than 40 was significantly associated with a decreased risk of ENL (OR = 0.69). The risk of ENL decreased linearly in the model as age increased. The risk of ENL increased linearly as the BI increased.
An analysis of risk factors for multiple episodes of ENL was also performed (Table 3). Unadjusted OR identified five factors associated with an increased risk of multiple episodes of ENL: a) an LL classification, b) a smear >4+, c) more than five nerves enlarged, d) the presence of skin nodules or e) infiltration. Age more than 40 was associated with a significantly decreased risk of ENL. When the same logistic regression model was applied to the outcome of multiple episodes of ENL, only an LL classification (OR = 4.6) and smear >4+ (OR = 1.42) were associated with increased with multiple episodes of ENL were corn- risk of multiple episodes of ENL, while pared with those of patients with single older patients were at significantly lower episodes of ENL in logistic regression risk (OR = 0.55). When factors in patients analysis, only the LL classification was associated with increased risk (OR = 2.94, p = 0.052).
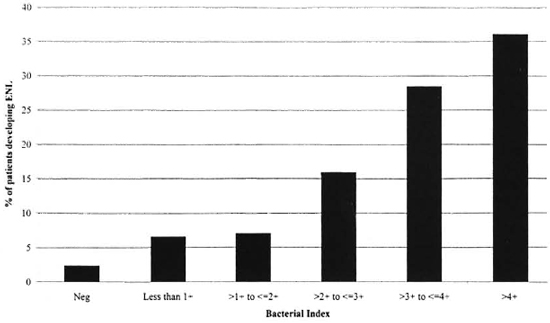
Fig. 2. Relationships between the bacterial index and the prevalence of ENL.
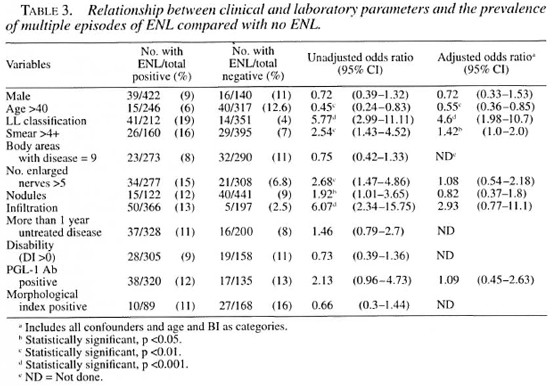
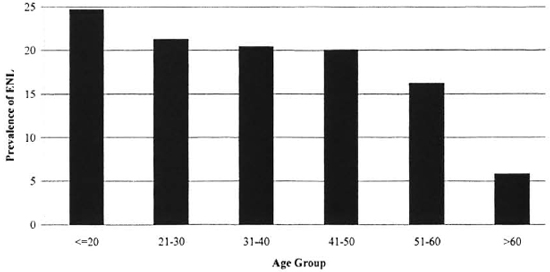
Fig. 3. Relationship between age and the prevalence of ENL.
DISCUSSION
This study has described a relatively high prevalence of ENL ( 19%) among new, previously untreated, borderline leproma- tous (BL) and lepromatous leprosy (LL) patients treated with MDT. This reflects prevalence in a specialist leprosy hospital to which patients suffering from ENL will be referred from all over Nepal. Before the introduction of MDT, as many as 50% of LL and 30% of BL patients developed ENL (x). The introduction of WHO/MB MDT has reduced both the frequency and severity of ENL, and this reduction may be attributable to the clofazimine component of MDT since MB patients treated with drug regimens without clofazimine continued to express high levels of ENL (3). In a field program in Ethiopia, incidence rates of 2.7% and 11.1% were found in BL and LL patients, respectively, treated with MDT (2).
ENL has been recognized to frequently recur in the patients it affects. In the present study, nearly half the patients with ENL had more than one episode. While ENL has previously been recognized as occurring late, during or even after treatment, this study indicates that 9% of ENL reactions will occur after the completion of MDT. It should be noted that in each case this was the first re- actional event in these patients.
ENL has been recognized to be more frequent in LL patients than in BL patients (6). In the present study, LL patients had a significantly higher prevalence of ENL (33%) than did BL patients (11%, p <0.001). Due to variation in classification between centers, the prevalence of ENL in BL patients may differ somewhat from that described here, but it will always be less frequent than among LL patients.
Patients with highly positive smears (mean BI >4+) were also found to be at a 39% higher risk of ENL. This accords with previous studies implicating a high BI in ENL patients (4). It has been hypothesized that a high bacterial antigen load will lead to immune complex formation which, in turn, will cause vasculitis and tumor necrosis factor-alpha (TNF-α) secretion from macrophages, which typify the immunological picture of ENL (6-11).
Histologically, bacteria in ENL have become downgraded and granular (6); hence we found no association between bacterial viability as measured by the solid-staining ratio (MI) and ENL. Previous studies (u) have suggested that ENL is more common when the MI is <5%, i.e., when there is a large number of dead bacilli. This could explain the prevalence of ENL relatively late in both dapsone monotherapy (5) and in the present study where 9% of the reactions occurred for the first time in patients who had completed 2 years MDT.
Related to a high mean BI is diffuse skin infiltration, which was associated in our study with a 2.7-times greater risk of ENL. Widespread diffusion of Mycobacterium leprae antigens in the skin could explain the occurrence of crops of ENL nodules in the skin. The occurrence of ENL in parts of the skin with previous lepromatous infiltration has been observed previously (5).
The finding of a lower prevalence of ENL among older patients and of a significant decline with increasing age (Fig. 3) is of importance to leprosy management. This is supported by an earlier study (4) which found that more patients aged 15-44 developed a reaction than did older patients or patients with a lower BI. Another study (12) found that patients with an onset of leprosy in the second decade of life were more likely to develop ENL. Our data based on age at first presentation could reflect a difference in the age of disease onset between ENL and non-ENL patients. The relationship between age and risk of ENL could reflect either an age-associated decline in immunity or an increased prevalence in young or adolescent patients.
Previous studies have implicated pregnancy, puberty, intercurrent illness, vaccination and stress to be associated with the development of ENL (5). There may, in addition, be a genetic basis for the development of ENL. Individuals with a genetic polymorphism in the promoter region of the tumor necrosis factor gene ( TNF2 ) are at higher risk of developing lepromatous leprosy (10). This gene polymorphism may also be associated with increased levels of TNF, a finding in the sera of ENL patients (11).
Patients with LL have a high concentration of mycobacterial antigen in their tissues and make high levels of both IgM and IgG antibodies. The formation of immune complexes and the activation of the complement pathway along with release of inflammatory mediators may explain the pathology and clinical symptoms associated with ENL (15). During ENL episodes, a fall in circulating IgM anti-phenolic glycolipid antibody levels has been noted, which returns to pre-reactional levels after the patient has recovered (1), suggesting that IgM anti-PGL-I may form immune complexes with the abundant PGL in the tissues. In this study, the scropositivity for anti-PGL-1 antibodies was associated with an increased unadjusted OR (Table 2). However, in the logistic regression model, probably due to the strong association between the antibody level and the BI, the adjusted OR for antibodies did not reach statistical significance.
In summary, this study has shown important characteristics of ENL reactions in patients being treated with MDT. Clinicians need to be aware that a significant number of ENL reactions will occur after completion of MDT. In addition, patients younger than 40 with LL disease, skin infiltration and a mean BI of >4+ are at a significantly higher risk of ENL and should be monitored throughout MDT. Shortening of the WHO/MDT MB regimen from 2 years to 1 year may also influence both the prevalence and timing of ENL reactions.
Acknowledgment. This work was supported by The Leprosy Mission International. The authors would like to thank the staff and patients of Anandaban Hospital for their cooperation in this study. This material was presented at the 15th International Leprosy Congress, Beijing, China, September 1998 (Abstract CL30) (Int. J. Lepr. 66:24A, 1998).
REFERENCES
1. Andreoli, A., Brett, S., Draper, P., Payne, S. N. and Rook, G. A. W. Changes in circulating antibody levels to the major phenolic glycolipid during erythema nodosum leprosum in leprosy patients. Int. J. Lepr. 53 (1985) 211-217.
2. Becx-Bleumink, M. and Berhe, D. Occurrence of reactions, their diagnosis and management in leprosy patients treated with multidrug therapy: experience in the leprosy control program of ALERT in Ethiopia. Int. J. Lepr. 60 (1992) 173-184.
3. Cellona, R. V., Fajarix), T. T., Jr., Kim, D. I., Hah, Y. M., Ramsoota, T., Sampattavanich, S., Carrillo, M. P., Abalos, R. M., delà Cruz, E. C., Ito, T. and Yuasa, Y. Joint chemotherapy trials in lepromatous leprosy conducted in Thailand, The Philippines and Korea. Int. J. Lepr. 58 (1990) 1-11.
4. Groenen, G., Janssens, L., Kayembe, T., Nollet, E., Coussens, L. and Pattyn, S. R. Prospective study on the relationship between intensive bactericidal therapy and leprosy reactions. Int. J. Lepr. 54 (1986) 236-244.
5. Pfaltzgraff, R. E. and Bryceson, A. Clinical leprosy. In: Leprosy. Hastings, R. C., ed. Edinburgh: Churchill-Livingstone, 1985, pp. 166-178.
6. Ridley, D. S. Pathogenesis of Leprosy and Related Disorders. London: Wright, 1988, pp. 123-130.
7. Ridley, D. S. and Jopling, W. H. Classification of leprosy according to immunity; a five-group system. Int. J. Lepr. 34 (1966) 255-273.
8. Ridley, D. S. and Waters, M. F. R. Significance of variations within the lepromatous group. Lepr. Rev. 40 (1969) 143-152.
9. Roche, P. W., Britton, W. J., Failbus, S. S., Ludwig, H., Theuvenet, W. J. and Adiga, R. B. Heterogeneity of serological responses in paucibacil- lary leprosy: differential responses to protein and carbohydrate antigens and correlations with clinical parameters. Int. J. Lepr. 58 (1990) 319-327.
10. Roy, S., McGuire, W., Mascie-Taylor, C. G. N., Saiia, B., Hazra, S. K., Hill, A. V. S. and Kwait-kowski, D. Tumor necrosis factor promotor polymorphism and susceptibility to lepromatous leprosy. J. Infect. Dis. 176 (1997) 530-532.
11. Sarno, E. N., Grau, G. E., Vieira, L. M. M. and Nery, J. A. Scrum levels of tumour necrosis factor- alpha and interleukin-1β during leprosy reactional states. Clin. Exp. Immunol. 84 (1991) 103-108.
12. Scollard, D. M., Smith, T., Bhoopat, L., Thee- tranat, C., Rangdaeng, S. and Morens, D. M. Epidemiologic characteristics of leprosy reactions. Int. J. Lepr. 62 (1994) 559-567.
13. van Brakel, W. H., de Soldenhoff, R. and Mc- Dougall, A. C. The allocation of leprosy patients into paucibacillary and multibacillary groups for multidrug therapy, taking into account the number of body areas affected by skin or nerve lesions. Lepr. Rev. 63 (1992) 231-245.
14. van Voorhis, W. C., Kaplan, G., Sarno, E. C., Horwitz, M. A., Steinman, R. M., Levis, W. R., Noguiera, N., Hair, L. S., Guttas, C. R., Ar- rick, B. A. and Cohn, Z. The cutaneous infiltrates of leprosy; cellular characteristics and the predominant T-cell phenotypes. N. Engl. J. Med. 307 (1982) 1593-1597.
15. Wemambu, S. N. C., Turk, J. L., Waters, M. F. R. and Rees, R. J. W. Erythema nodosum leprosum: a clinical manifestation of the Arthus phenomenon. Lancet 2 (1969) 933-935.
16. WHO Expert Committee on Leprosy. Fifth report. Geneva: World Health Organization, 1977. Tech. Rep. Ser. 607.
1. B.Sc. (Hons.); Mycobacterial Research Laboratory, Anandaban Leprosy Hospital, P.O. Box 151, Kathmandu, Nepal.
2. M.D., Mycobacterial Research Laboratory, Anandaban Leprosy Hospital, P.O. Box 151, Kathmandu, Nepal.
3. Ph.D., Mycobacterial Research Laboratory, Anandaban Leprosy Hospital, P.O. Box 151, Kathmandu, Nepal.
Reprint requests to Paul Roche, Ph.D. at the above address or FAX: 977-1-290-538; e-mail: roche@umn.mos.com.np
Received lor publication on 28 December 1998.
Accepted for publication in revised form on 20 May 1999.