- Volume 68 , Number 1
- Page: 65–7
Assessment of skin temperature by palpation in leprosy patients: interobserver reliability and correlation with infrared thermometry
To the Editor:
In patients with neuropathic feet there is a high risk of complications such as ulceration or ncuro-osteo-arthropathy (Charcot deformity). Pain as an early sign for this is not perceived because of loss of sensory function. Local hyperemia is also an early sign. This hyperemia can be recognized as a local or diffuse warm foot. Benbow and Armstrong made it clear that an elevated skin temperature is highly predictive of future ulceration and is directly correlated with the location of acute neuro-osteoarthropathy (1,2). Bergtholdt and Brand recommended temperature assessment as an instrument in providing the patient with a participatory role in early injury recognition and in the rehabilitation program (3-4). In these studies, skin temperatures were assessed using either liquid-crystal contact thermography or infrared dermal thermometry. In the normal clinical practice, however, skin temperature is assessed by palpation. Therefore, we wanted to test the interobserver reliability of assessment of skin temperature by palpation and the correlation with infrared thermometry.
The study included all leprosy patients with a neuropathic foot visiting the outpatient leprosy clinic of the Amsterdam Medical Center, Amsterdam, The Netherlands, during three consecutive months in 1996. Twentγ-five patients (13 males, 12 females) with 49 feet (one patient had a below-knee amputation) were assessed. The mean age was 53.3 ± 14.9 years. All patients had peripheral sensory and motor function loss and a dry skin as a result of autonomic nerve dysfunction. The group was heterogeneous with respect to the complications of their neuropathic feet: ulceration or neuroosteo-arthropathy.
For objective skin assessment we used an infrared thermometer (Genius 3000A Thermometer; Sherwood Medical Nederland B.V.). A special device was attached to the top of it to obtain a constant distance of 0.5 cm between the thermometer and the skin. Skin temperature was assessed using the following procedure: patients were sitting for 10 min in a normal chair with their bare feet resting on a towel on the floor. (In a previous study we determined that after removing socks and shoes 10 min are required to get a steady state of skin temperature in neuropathic feet; unpublished observations.) Two examiners assessed skin temperature by palpation using the following scoring system: -2 (very cold), -1 (cold), 0 (normal), +1 (warm) +2 (very warm). The precise way to do this palpation was not defined, neither were the terms "warm" and "cold." The examiners palpated the way they had experienced to be the best for themselves. They scored a foot as "warm" in comparing the different parts of the foot, the rest of the leg and the other side, taking into account other clinical features such as color and presence of edema. Because of the possibility of complications in both feet together, we assessed absolute values of temperature (as did Armstrong and Benbow) and not the difference in temperature between the left and right feet. The second examiner marked the localization on the foot, where a third examiner assessed skin temperature by infrared thermometry. This localization was either the place of "abnormal" skin temperature or (in the case of no differences) over the dorsal side of the medial arch. Skin temperature of the hands of the two examiners was not assessed, nor was the temperature of the room in which the study took place because we wanted to imitate the normal clinical practice situation in which temperatures of the examiner's skin and of the environment may vary and are not known.
The assessment of skin temperature by palpation by both examiners is shown in Figure 1. In this figure the left and right feet are taken together. Calculation of kappa was done for both feet separately: 0.83 for right feet and 0.74 for left feet, which is a high level of agreement.
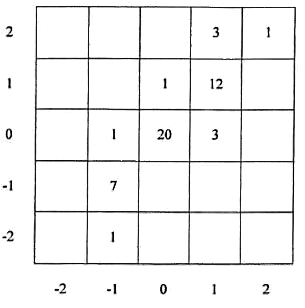
Fig. 1. Correlation between palpated skin temperature scores of the two examiners; left and right foot are shown together.
Correlation palpation and infrared thermometry is shown in Figure 2. Each patient is shown by four points: two feet assessed by two examiners. Statistical analysis with Spearman's rank correlation does not allow the use of four points per person because those four points are dependent. We, therefore, calculated correlation for one point for each patient; we did this in three different ways: a) by using the mean objective skin temperature of the left and right feet and the mean palpated skin temperature of the left and right feet for the two examiners; b) for left and right feet separately; and c) separately for the two examiners. Spearman's rank correlation coefficient in all three situations was 0.82 (p <0.002), which is a significant and good correlation. We did the same statistical analysis for differences in temperature between the left and right feet. Spearman's rank correlation coefficient between palpation and thermometry of these differences was 0.81 (p <0.000).
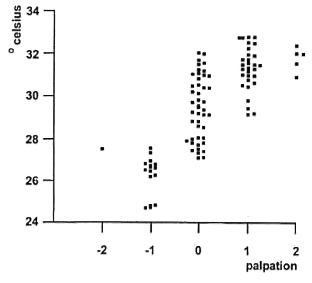
Fig. 2. Correlation between skin temperature scores assessed by palpation and by infrared thermometry. Each person is presented by four points: two feet (except for the patient with a below-knee amputation) and assessed by two examiners.
The same study was done in a control group of healthy persons without foot problems. In this group there was no agreement (kappa for the two examiners was negative), and there was no correlation between palpation and thermometry (Spearman's rank correlation coefficient was 0.36; p = 0.125). There was no difference in mean temperature between healthy persons and leprosy patients who were palpated as being "normal" (leprosy group mean 29.3ºC ± 1.4; control group mean 28.9ºC ± 1.3).
Our study indicates that assessment by palpation of neuropathic feet in leprosy patients can be done reliably when performed by experienced clinicians. To be effective as a preventive tool, however, palpation of skin temperature should be performed by people who can do so very frequently. In that case every change in skin temperature can be followed immediately by preventive measures.
Therefore, it should be investigated whether palpation of skin temperature of neuropathic feet is equally reliable when it is done by less-experienced health workers, members of the patient's family and/or the patient him/herself. The results of such an investigation may provide a guideline for a therapeutic program for leprosy patients in order to prevent further complications of their neuropathic feet.
- Agnes F. Hoeksma, M.D.
Specialist in Rehabilitation Medicine
Department of Rehabilitation Medicine
- William R. Faber, M.D., Ph.D.
Dermatologist
Professor of Tropical Dermatology
Department qf Dermatology
Academie Medical Center University of Amsterdam
PO. Box 22660
1100 DD Amsterdam, The Netherlands
REFERENCES
1. ARMSTRONG, D. G. and LAVERY, L. A. Monitoring healing of acute Charcot's arthropathy with infrareddermal thermometry. J. Rehab. Res. Dev. 34 (1997)317-321.
2. BENBOW, S. J., CHAN, A. W., BOWSHER, D. R., WILLIAMS, G. and MACFARLANE, I. A. The prediction of diabetic neuropathic plantar foot ulceration by liquid-crystal contact thermography. Diabetes Care 17(1994)835-839.
3. BERGTHOLDT, H. T. Temperature assessment in the insensitive foot. Phys. Ther. 59 (1979) 18-22.
4. BERGTHOLDT, H. T. and BRAND, P. W. Temperature assessment and plantar inflammation. Lepr. Rev. 42 (1976)211-219.
Reprint requests to Mrs. A. F. Hoeksma, M.D., Slotcrvaart Zickenhuis, Departmentof Rchabilitation, Louwesweg 6, 1066 ECAmsterdam, The Netherlands.