- Volume 68 , Number 2
- Page: 152–5
Epithelioid granuloma in the Iris of a lepromatous leprosy patient; an unusual finding
ABSTRACT
This case report depicts a case of histopathologically confirmed polar lepromatous (LL) leprosy with a bacterial index of 4+. He experienced recurrent episodes of erythema nodosum leprosum (ENL) in the first 5 years after diagnosis. Skin smears became negative after 6 years of dapsone monotherapy and have remained negative since that time. At 23 years after diagnosis, the patient had developed cataracts and underwent intracapsular cataract extractions with broad- based iridectomies. In one of the iris specimens, histopathologic examination revealed a focal granuloma composed of epithelioid cells. Subsequently a lepromin skin test showed a positive Mitsuda reaction with a borderline tuberculoid histopathology. This clearly illustrates the immunological upgrading of a polar lepromatous patient, perceived first in the iris tissue.RÉSUMÉ
Ce cas clinique décrit un exemple confirmé d'un patient atteint de lèpre lépromateuse polaire (LL), avec un index bactérioscopique 4+. E patient a connu des périodes à répétition d'érythème noueux lépreux (ENL) dans les 5 années qui ont suivi le diagnostic. L'examen du suc dermique devint négatif après 6 années de monothérapie à l'aide de dapsone et est resté négatif depuis lors. Vingt-trois années après le diagnostic, ce patient a développé une cataracte bilatérale qui a nécessité une extraction intra-capsulaire des 2 cristallins, accompagnée d'une iridectomie large. Dans l'une des biopsies d'iris, il a été trouvé à l'examen histopathologique un granulome composé de cellules épithélioïdes. Il a été ensuite effectué un test cutané à la lépromine, qui a montré une réaction de Mitsuda caractérisée par des lésions de type tuberuloïde borderline. Ce cas illustre clairement l'amélioration de l'immunité à médiation cellulaire d'un patient lépro- mateux polaire, découvert fortuitement en premier dans le tissu irien.RESUMEN
En esta comunicación se presenta el caso de un paciente con lepra lepromatosa polar (LL) histopatológicamente confirmada, con un índice bacilar de 4+ al momento del diagnóstico. En los primeras 5 anos siguientes a su diagnóstico el paciente presentó vários episódios récurrentes de eritema nodoso leproso (ENL). Los extendidos de linfa cutânea se hicieron negativos después de 6 anos de tratamiento con dapsona y así han permanecido desde entonces. Veintrités anos después, el paciente desarrolló cataratas intracapsulares que le fueron extraídas con iridectomías de base amplia. En uno de los especimenes de iris, el examen hitopatológico revelo un granuloma focal compuesto por células epitelioides. Una prueba con lepromina praeticada después, dio una reacción de Mitsuda positiva, con histopatología tuberculoide subpolar. Los resultados indican una clara conversion immunlógica del estado lepromatoso al estado tuberculoide en este paciente que fue percibida primero en el tejido del iris.Leprosy is still a major contributor to world blindness (2). Iridocyclitis is the most common cause of irreversible blindness in leprosy, and its etiology is poorly understood. In contrast to the reactions in the dermal and neural tissues in generalized leprosy, ocular tissues are more difficult to study because the internal ocular tissues cannot be biopsied without great risk to the eye. Therefore, information known about leprosy reactions elsewhere in the body must be applied to the eye. This is done with the understanding that these comparisons may not be accurate and that much research needs to be done on this ocular disease, both clinically and in the laboratory (6).
A few studies have investigated the histopathology of the iris in leprosy. Most of these studies have been on iris specimens obtained from lepromatous patients. In lepromatous leprosy, the iris and the ciliary body are found to be infiltrated with macrophages containing numerous Mycobacterium leprae (4). Epithelioid cells are the predominant cells found in the tuberculoid (BT-TT) side of the leprosy spectrum, and although these cell types may be seen in some borderline lepromatous (BL) patients they are never seen in lepromatous (LL) leprosy (3). We report here the unusual finding of an epithelioid granuloma in the iris of a lepromatous leprosy patient who had had several episodes of erythema nodosum lep- rosum (ENL) and iridocyclitis.
CASE REPORT
A 35-year-old man with a history of a hypopigmented patch on his right thigh for 6 years presented with classical symptoms of ENL at the Schieffelin Leprosy Research and Training Center in Karigiri, India, in 1975. Bilateral madarosis, crusting of the nose, glove-and-stocking type anesthesia, right ulnar paralysis and an ulcer on the left big toe were also present. He was treated for ENL and for the foot ulcer and started on 50 mg of dapsone daily. His skin smears had an average bacterial index (BI) of 4.00+. He had ENL again in 1978 and again in 1980.
Histopathological examination of a skin biopsy from the left elbow in 1978 showed the epidermis to be markedly flattened and atrophic. A dense layer of macrophages was seen just below the subepithelial layer. In one area there was a nodule composed of concentrically arranged spindle-shaped cells which showed numerous granular and intact bacilli. The deeper dermis had large collections of macrophages filled with numerous acid-fast bacilli (AFB). The histology confirmed the patient to be a case of polar lepromatous (LL) leprosy.
Treatment with dapsone was continued until June 1996, at which time he was started on World Health Organization multidrug therapy (WHO/MDT). A lepromin injection was given in June of 1996 but no reading was recorded at the end of 4 weeks since the patient did not present at the clinic. He was seen again after 2 months and the reading was negative. The patient completed 24 doses of MDT only in February 1999. Skin smears taken annually were negative from 1981 onward.
Ophthalmic history. The patient had 6/6 (in meters, corresponding to 20/20 in feet) vision in both eyes and bilateral madarosis when initially examined in 1975. Subsequently, in March 1980 he had iridocyclitis in both eyes which cleared up with topical steroid drops. In 1990 his vision had dropped to 6/36 in the right eye and 1/60 in the left eye. Both eyes had cataracts with old keratic precipitates on the back of the cornea and some amount of iris atrophy near the pupillary border. Since there was no recent history of any inflammatory reaction in the eyes and no clinically active ocular inflammation was discernable by biomicroscopy, an intracapsular cataract extraction was done with a broad based iridectomy in the left eye in November 1991. Recovery was uneventful and the patient had a corrected vision of 6/9.
The iris specimen which was removed after iridectomy was studied histopathologi- cally. The iris stroma showed sparse inflammatory infiltrate consisting of lymphocytes, histiocytes and pigmented macrophages. No AFB were seen. In June 1998, the vision in the right eye had deteriorated to only perception of light, and so a similar surgery as was done on the left eye was done on the right eye. The iris specimen sent for histopathological examination showed diffuse chronic inflammatory infiltrates consisting of lymphocytes, histiocytes, pigmented macrophages, vacuolated cells and occasional mast cells. In one area a focal granuloma composed of epithelioid histiocytes was seen adjacent to the anterior epithelium (The Figure). Acid-fast staining showed no bacilli. A lepromin test done a few weeks after the surgery showed a positive Mitsuda reaction (7 mm x 11 mm). The skin over the Mitsuda reaction was biopsied and examined histopathologically. A piece of skin taken from the back of the right arm was also studied histopathologically.
The Mitsuda skin reaction specimen showed a borderline tuberculoid type of histopathology with relatively circumscribed dense granulomatous inflammation composed of epithelioid aggregates, occasional giant cells, a moderate number of lymphocytes and a few macrophages containing AFB in the mid and upper dermis. The skin biopsy from the back of the right arm showed residual lepromatous granulomas- small focal collections of foamy macrophages with a few plasma cells and lymphocytes in the dermis around blood vessels and skin adnexa. Acid-fast staining revealed no bacilli.
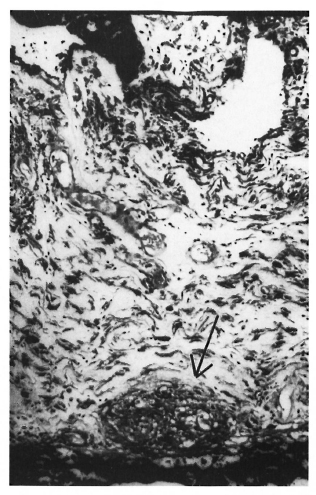
The Figure. Photomicrograph showing iris stromal tissue with a microgranuloma ( ) composed of epithelioid cells just above the epithelial lining of its posterior surface (H&E x200).
) composed of epithelioid cells just above the epithelial lining of its posterior surface (H&E x200).
DISCUSSION
This case depicts the most unusual finding of an epithelioid granuloma in the iris of a lepromatous leprosy patient. An epithelioid granuloma presenting in the iris of lepromatous patients (1-5-8) has never been described before.
The histopathology of the initial skin biopsy proved that the patient belonged to the polar LL group. ENL reactions had subsided completely after the skin smears had become negative for AFB. Lepromin testing in 1996, although not read in exactly 3 weeks, presented a negative Mitsuda reaction. When lepromin testing was repeated 2 years later, it showed a positive Mitsuda reaction. Histopathology of the Mitsuda reaction showed a borderline tuberculoid (BT) pattern. It is known that the histological pattern of the local Mitsuda reaction corresponds closely to the lesions due to the disease itself and its clinical classification (7). In this patient, the histopathology of a skin biopsy done at the time of the positive Mitsuda reaction showed characteristics of residual lepromatous granulomas.
These features testify to the rare occurrence of lepromin conversion in a polar lepromatous patient. Lepromatous leprosy patients after many years of chemotherapy and bacteriological negativity have been known to show positive Mitsuda reactions (10) and to relapse as borderline tuberculoid leprosy (9). As in these cases visible upgrading reactions were not noticed in this patient, presumably due to the low level of antigen in the almost resolved lesions, i.e., there was too little residual antigen to trigger a clinically apparent reversal reaction.
The appearance of the epithelioid granuloma in the iris of a histopathologically proven lepromatous leprosy patient further validates the fairly rare occurrence of polar lepromatous leprosy upgrading to a tuberculoid form of the disease. Whether MDT was responsible for this is a moot point, but this report clearly illustrates the immunological upgrading of a lepromatous patient, perceived first in the iris tissue.
REFERENCES
1. Daniel, E., Ebenezer, G. J. and Job, C. K. Pathology of the iris in leprosy. Br. J. Ophthalmol. 81 (1997)490-492.
2. FFytche, T. J. Importance of early diagnosis of ocular leprosy. (Editorial). Br. J. Ophthalmol. 73 (1989)939.
3. Job, C. K. Pathology of leprosy. In: Leprosy. 2nd edn. Hastings, R. C., ed. Singapore: Churchill Livingstone, 1994, p. 198.
4. Job, C. K., Ebenezer, G. J., Thompson, K. and Daniel, E. Pathology of eye in leprosy. Indian J. Lepr. 70(1998)79-91.
5. Jon, C. K. and Thompson, K. Histopathological features of lepromatous iridocyclitis; a case report. Int. J. Lepr. 66 (1998) 29-33.
6. Joffion, V. C. Ocular leprosy. In: Leprosy. 2nd edn. Hastings, R. C., ed. Singapore: Churchill Livingstone, 1994, p. 360.
7. Thomas, J., Joseph, M., Ramanujam, K., Chacko, C. J. K. and Job, C. K. The histology of the Mitsuda reaction and its significance. Lepr. Rev. 51 (1980)329-339.
8. Thompson, K. and Jon, C. K. Silent iritis in treated bacillary negative leprosy. Int. J. Lepr. 64 (1996)306-310.
9. Waters, M. F. and Ridley, D. S. Tuberculoid relapse in lepromatous leprosy. Lepr. Rev. 61 (1990) 353-365.
10. Waters, M. F. R., Ridley, D. S. and Lucas, S. B. Positive Mitsuda lepromin reactions in long-term treated lepromatous leprosy. Lepr. Rev. 61 (1990) 347-352.
1. M.S., D.O.. Head. Department of Ophthalmology;Schieffelin Leprosy Research and Training Center,Karigiri, Vellore District. Tamil Nadu, India 632106.
2. M.D., Head. Department of Histopathology and Experimental Pathology; Schieffelin Leprosy Research and Training Center,Karigiri, Vellore District. Tamil Nadu, India 632106.
3. M.D., Head, Branch of Medicine; Schieffelin Leprosy Research and Training Center,Karigiri, Vellore District. Tamil Nadu, India 632106.
4. M.D., F.R.R.C.Path., F.A.M.S., Emeritus Scientist, Schieffelin Leprosy Research and Training Center,Karigiri, Vellore District. Tamil Nadu, India 632106.
5. L.V.O., F.R.C.S.. F.R.C.Ophth., Consultant Ophthalmologist, St. Thomas' Hospital, Lambeth Palace Road, London SE1 7EH, U.K.
Received for publication on 6 July 1999.
Accepted for publication in revised form on 2 February 2000.