- Volume 68 , Number 2
- Page: 172–6
Survey of newly diagnosed leprosy patients in native and foreign residents of Japan
Editorial opinions expressed are those of the writers.
The World Health Organization (WHO) estimates that there were only 800,000 leprosy patients in the world who needed chemotherapy at the beginning of 1998.1 About 690,000 new cases were detected during 1997. A characteristic geographic feature of leprosy is that almost all of the patients live in developing countries, such as India, Brazil, Indonesia, Bangladesh. Japanese patients newly diagnosed with leprosy in Japan have been decreasing, and patients who come from foreign countries to work in Japan have been more important in leprosy control.1-4
In this paper, we analyze the patterns of newly registered leprosy patients over the past 19 years in a low-endemic country, Japan.
METHODS
We sent a questionnaire to a number of dermatological clinics and leprosaria in Japan to gain detailed data on new leprosy patients. Information about new leprosy patients was also obtained from journals, presentations, and private communications at all opportunities. We define new leprosy patients as newly registered patients in Japan, but not already registered or relapsed patients.
The questionnaire included details on age, nationality, family history, skin involvement, neurological impairment, bacterial findings, and treatment. We adopted the Ridley-Jopling criteria for the types of leprosy because multibacillary (MB)-paucibacillary (PB) criteria have been modified repeatedly. We analyzed the decreasing rate of leprosy patients by year, age group, and immunological type of leprosy.
RESULTS
We analyzed new leprosy patients diagnosed from 1981 to 1999 in Japan. As shown in Figure 1, 378 Japanese patients (229 males, 149 females) and 102 foreign patients (74 males, 26 females, 2 sex unknown) were registered over this 19-year period. The number of Japanese patients in each 5-year period was 187 (1981-1985), 119 (1986-1990), 48 (1991-1995), and 24 (1996-1999, 4 years), and the number has been decreasing steadily. But the numbers of foreign patients in each 5-year period were 7, 10, 45, and 40, respectively, i.e., they have been increasing. The number of foreign patients was greater than the number of Japanese patients in the latter half of the period, 1991-1999. The male/female ratio was 229/149 in Japanese patients and 74/26 in foreign patients. The male/female ratio has decreased among Japanese but has increased among foreigners.
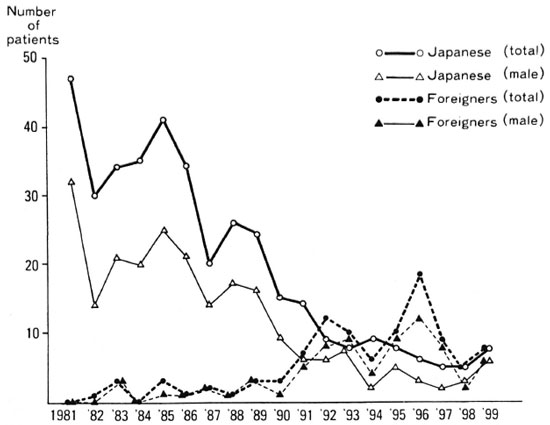
Fig. 1. Newly registered leprosy patients in Japan (1981-1999).
The age distribution of Japanese patients between 1981-1990 ranged widely from preteens to persons in their 90s as shown in Figure 2. Although their distribution between 1991-1999 ranged from those in their 20s to those in their 90s, it shifted to older ages (older than 60), and very few patients younger than 40 were registered. There were only 17 foreign patients registered in the first half of the period, but 85 patients, including 72 (84.7%) between the ages of 20 and 40, were registered in the latter half of the period.
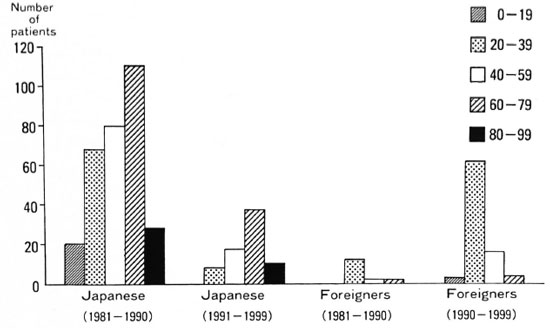
Fig. 2. Age distribution of new leprosy patients in Japan (1981-1999).
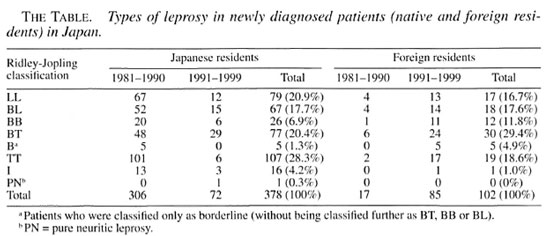
We divided the patients into seven types according to the Ridley-Jopling classification (The Table). The BL, BB, BT, and B classifications were predominant among both Japanese (175 cases, 46.3%) and foreigners (65 cases, 63.7%). There was one Japanese case classified as pure neuritic leprosy in 1998.
DISCUSSION
In 1953, the Japanese leprosy prevention law was revised to prolong the mandatory and forced hospitalization of persons with Hansen's disease, a policy that had been in effect since 1931, Over the years, the inappropriateness of the segregation policy was realized and forced segregation was practically discontinued in the 1960s. In 1996, the Japanese leprosy prevention law was abolished.
Leprosy is known to occur at all ages, ranging from early infancy to very advanced age. Furthermore, disease occurrence by age is often related to age at'detection rather than age at onset of disease. The occurrence of leprosy, presumably for the first time, is not uncommon even after the age of 60. A pattern observed in low-endemic areas where the disease is dying out is that the bulk of cases are advanced in age. This shift to the right as seen in age distribution graphs has been observed in Japan, the United States, and northern Europe. Japanese patients have evidently decreased and elderly patients have become dominant as shown in this paper. As the disease declined, there has been a gradual increase in the mean age at onset of the disease. The percentage of Japanese patients over 60 increased from 45.1% to 65.3% between the first and second half of our study period but dropped from 11.8% to 4.7%, respectively, among foreigners.
In Japan, foreign patients from developing countries are younger than those from developed countries. The reason for the increase in young foreign patients may be that it is harder for elderly people to find work in Japan. The phenomenon of the increase in elderly leprosy patients seems to be consistent with the dying out of the disease in Japan. These aged new patients passed their childhood while leprosy was endemic in Japan, and although they were at risk of infection with Mycobacterium leprae in their childhood, they probably kept their high level of immunity against M. leprae. However, when they aged they may have developed clinical leprosy because of a lowered level of immunity against M. leprae. Almost all active leprosy patients in Japan have been under control, and it has now probably become uncommon for Japanese people to be infected with M. leprae.
Therefore, newly registered patients have significantly diminished among the younger generations. Recent newly registered patients have decreased (0.04/100,000 and 0.003/100,000 in 1981 and 1997, respectively). These results suggest that leprosy is dying out in Japan. On the other hand, the number of foreign patients has increased, and was five times the number in the latter half of the study period (1991-1999) as compared to the first half (1981-1990). The number of foreign patients has increased, because the number of foreign workers from developing countries has increased, and most of them are in their 20s to 40s. Foreign workers, especially from developing countries, come to Japan to work in order to get money. About 230,000 Brazilians and 100,000 Filipinos work in Japan. Japanese-Brazilians can easily get a work visa, and their number has increased since 1989. Forty-three leprosy patients (42.3%) came from Brazil, a highly leprosy-endemic country. Other patients came from Bangladesh, Paraguay, and other highly endemic countries. Male workers from endemic countries are registered. Although they often have to work hard, they do not have enough food and live in small rooms. Most of them might have had contact with leprosy patients in infancy in their own countries, but their leprosy was detected in Japan.
Male Japanese patients amounted to 60.6%, but the ratio of males to females was almost the same in the latter half of the period. Although leprosy affects both sexes, in most parts of the world males are affected more frequently than females, often in the ratio of 2:1.5 This ratio approaches 1:1 as the number of patients decreases. The patterns of age and sex distribution of Japanese patients are very similar for both sexes, except for the small number of females. In foreign patients, males were dominant because most workers were male.
Cases that are found in areas in which leprosy is dying out are said to be predominantly lepromatous leprosy.5 But, our study revealed the dominance of borderline (BL, BB, BT, B) patients among the Japanese. This might rcfiect the immunological unstableness among the aged against M. leprae.
Leprosy is expected to be overcome in the early 21st century. It is important to survey and follow up leprosy in Japan because developing countries may have the same problems in the near future.
Acknowledgment. We are grateful to Prof. Richard C. Goris for critical comments. This work was partially supported by a grant-in-aid (11670844) from the Japanese Ministry of Education, Science, Sports and Culture.
- Norihisa Ishii, M.D., Ph.D.
Leprosy Research Center
National Institute of Infectious Diseases
4-2-1 Aobacho
Higashimurayama
Tokyo 189-0002, Japan
- Masahito Onoda, M.D.
Yasuyuki Sugita, M.D., Ph.D.
Department of Dermatology
Yokohama City University School of Medicine
Yokohama, Japan
- Masakazu Tomoda, M.D., Ph.D.
National Leprosarium Nagashima Aisei-en
Okayama, Japan
- Motoaki Ozaki, M.D., Ph.D.
Department of Dermatology
Amagasaki Prefectural Hospital
Hyogo, Japan
1. WHO Wkly Epidemiol. Rec. 73 (1998) 305-312.
2. Ishii, N., Sugita, Y. and Nakajima, H. [Epidemiological study of leprosy from 1993 lo 1997 in Japan.] Jpn. J. Dermatol. 109 (1999) 763-767.
3. Kikuchi. I. Hansen's disease in Japan: a brief history. Int. J. Dermatol. 36 (1997) 629-633.
4. Ozaki, M. and Tomoda, M. [Decrease of newly registered leprosy patients in Japan-epidemiological study of leprosy as non-endemic disease.] Jpn. J. Dermatol. 103(1993) 1867-1876.
5. Noordeen, S. K. The epidemiology of leprosy. In: Leprosy. Hastings, R. C., ed. Edinburgh: Churchill Livingstone, 1994, pp. 29-45.
Reprint requests to Dr. Ishii's present address: N. Ishii, M.D., Ph.D., Director, Department of Bioregulation, Leprosy Research Center, National Institute of Infectious Diseases, 4-2-1Aobacho, Higashimurayama, Tokyo 182-0002, Japan, or FAX 81-42-391-8776; e-mail: norishii@nih.go.jp