- Volume 68 , Number 3
- Page: 291–8
Knowledge and attitude of health professionals in relation to the integration of leprosy control into the general health service in Ethiopia
ABSTRACT
Since the introduction of multidrug therapy for leprosy patients, the integration of leprosy control in the general health service (GHS) system has been an issue of debate. In Ethiopia, the present policy stresses integrated management of diseases. In spite of the policy, however, leprosy control was a vertical program until 1998 in most parts of the country. A descriptive cross-section study was conducted in the southern region of Ethiopia from October 1996 to March 1997 to determine the levels of involvement of the GHS staff and to identify obstacles to their involvement in the management of leprosy patients. Through a written questionnaire, data were collected from 240 GHS staff, including doctors, nurses and health assistants. It was found that 6% of the GHS staff was involved in leprosy control activities, mainly case finding and health education. Negative attitudes toward leprosy workers were held by 13% of the GHS staff while 40% had intermediate attitudes and the remaining 47% had positive attitudes. Statistically significant differences were found with regard to the level of knowledge among different health professionals, type of health institutions and years of service. The levels of involvement, knowledge and attitude of GHS staff showed that lack of integration and training were core problems. Hence, policy makers should give due attention to promoting the involvement of the GHS staff by integrating the program into the GHS system using the approach already in place in certain parts of the country.RÉSUMÉ
Depuis l'introduction de la poly chimiothérapie chez les patients lépreux, l'intégration du contrôle de la lèpre dans le système des services de santé généraux (SSG) a fait l'objet de nombreuses discussions. En Ehtiopie, la loi actuelle met l'emphase sur un traitement et une prévention intégrée des maladies. Cependant, en dépit de cette loi, lo contrôle de la lèpre était un programme vertical jusqu'en 1998 dans la plupart des régions du pays. Une étude descriptive fut conduite dans la région septentrionale de l'Ethiopie de octobre 1996 à mars 1997 pour déterminer les niveaux d'engagement du personnel des SSG et pour identifier des obstacles à leur engagements pour les soins aux patients lépreux. A l'aide d'un questionnaire, des données furent recueillies provenant de mambres des équipes des SSG, incluant des médecins, des infirmières et des assistants de santé. Il fut trouvé que 6% du personnel des SSG est impliqué dans des activités de contrôle de la lèpre, principalement de dépistage des cas et la sensibilisation à l'hygiène. Des attitudes négatives envers le personnel de santé travaillant avec des patients lépreux furent trouvées chez 13% du personnel de SSG tandis que 40% eurent des attitudes intermédiaires et 47% des attitudes positives. Des différences stastiquement significatives furent trouvées en ce qui concerne le niveau des connaissances parmi les différents professionnels de la santé, et en fonction du type d'institution médicale et des années de service. Les niveaux d'engagement, de connaissance et d'attitude du personnel des SSG ont montré que le manque d'intégration et d'éducation étaient des problèmes majeurs. Ainsi, le législateur concentrer son action en vue de promouvoir l'engagement du personnel des SSG en intégrant le programme contre la lèpre dans le système des SSG, en utilisant une approche déjà en place dans certaines parties du pays.RESUMEN
Desde la introduction de la quimioterapia para el tratamiento de la lepra, la integration del programa de control de la lepra al sistema general de salud (SGS) ha sido un tema de amplio debate. Aunque la política actual en Etiópia recomienda el manejo integrado de las enfermedades, hasta 1998 el control de la lepra fue un programa vertical en la mayor parte del país. Con el fin de promover la integración, de octubre de 1996 a marzo de 1997 se hizo un estúdio transversal en la region del sur de Etiópia para determinar los niveles de participación del personal dei SGS y para identificar los obstáculos que pudieran estorbar su participación en el manejo de los pacientes con lepra. Los datos se colectaron de 240 trabajadores del SGS, incluyendo doctores, enfermeras y asistentes de salud. Se encontró que 6% dei personal del SGS estuvo comprometido en actividades de control de la lepra, principalmente en el descubrimiento de casos y en education de la salud. Dentro de los trabajadores de la lepra, 13% del personal del SGS mostró actitudes negativas, 40% actitudes intermedias, y 47% actitudes positivas. También se encontraron diferencias estadísticamente significativas en el nivel de conocimiento de los profesionales de la salud, que fueron dependientes de la institución de su adscripción y de sus anos de servicio. El nivel de participación, conocimiento y actitud de los trabajadores del SGS, revela que los problemas fundamentals son la falta de integración y de entre nameinto. Los estrategas de las políticas de salud deben promover la participación del personal del SGS en el programa de control de la lepra, siguiendo el modelo que ya está en práctica en algunas regiones del pais.The social picture of leprosy has changed over the last decades. It is being regarded more and more as any other public health problem which can be managed in any general health service. All countries have officially adopted the outpatient clinic as the base for treating leprosy, while old stigmatizing leprosaria are being phased out. This approach deserves strong support from health personnel and others at all levels in order to guarantee patients adequate treatment as well as self respect (6).
After the considerable progress made in the control of leprosy through the implementation of multiple drug therapy (MDT) during the last decade, the prevalence of the disease decreased dramatically. Based on the very encouraging results from MDT within the last decade, the World Health Assembly (WHA) in 1991 resolved to eliminate leprosy (prevalence below 1 per 10,000 people) as a public health problem by the year 2000 (7).
The concept of integrating vertical projects into the basic health services is gaining wide acceptance based on the consideration that integration will lead to much more efficient use of staff, transportation and financial resources (4).
In some endemic countries leprosy control programs are still vertical from the national to the operational level, with specialized staff and clinics which are separated from other health services. This type of service has its own limitations, leading to restricted achievement in leprosy control. The most frequently reported limitations are insufficient coverage, lack of comprehensive and continuous health care, insufficient use of resources, stigma and dependency on donors (2). In order to overcome these limitations, the general health services (GHS), which usually provide better coverage of the population than vertical programs, must be involved.
Since the implementation of MDT, the integration of leprosy control into the GHS has gained much wider acceptance. Integration means that leprosy control activities become the responsibility of the GHS, i.e., a multipurpose, permanent and decentralized health service, that is as close to the community as possible (2). To a great extent this is based on the best utilization of resources because with the decreasing number of registered cases, vertical programs have become less efficient. However, integration of leprosy services with the general medical services should be to the advantage of the patients (1).
At present with the policy of decentralization in Ethiopia, leprosy and its control have become the responsibilities of the regional health bureaus (Ethiopia Ministry of Health. Health policy of the transitional government of Ethiopia, September 1993). In spite of the policy, the control program was vertically organized in most parts of the country until 1998. There are several factors which need investigation before completely handing over the program to the GHS in order to avoid the negative effects on patient management. Based on these facts the aim of this study was to determine the levels of involvement of the GHS staff in leprosy control and to identify obstacles to their involvement in the management of leprosy patients in the Southern Nations Nationalities and Peoples Region (SNNPR) of Ethiopia.
MATERIALS AND METHODS
The involvement of the GHS staff in the management of leprosy in SNNPR was assessed using a descriptive cross-sectional study between October 1996 and March 1997. The region has a population of 11.3 million within nine zones and five special woredas/districts. A total of 2476 health workers consisting of 224 (9%) medical doctors, 446 (18%) nurses and 1806 (73%) health assistants were working in 10 hospitals, 31 health centers and 381 health stations of the region (SNNPRG Health Bureau Planning and Programming Service. Health and Health-Related Indicators in SNNPR, March 1997).
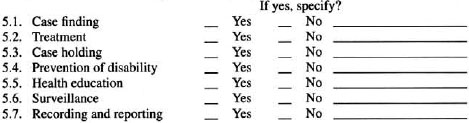
Using a multistage sampling, a total of 250 health workers in the GHS were selected from five zones to complete a written questionnaire. The questionnaire was prepared in English (All health professionals involved in the study attended their formal training in English.) and pretested for better clarity and understanding on 25 health workers who were not included in the actual study. During the administration of the written questionnaire, one of the investigators was present to clarify each question for the respondents. Variables such as type of health institution, profession, gender, years of service, level of involvement in various leprosy control components (case finding, treatment, case holding, health education, prevention of disability, surveillance and recording and reporting), attitude variables related to willingness to be involved in different leprosy control components, and knowledge variables, such as cardinal signs of leprosy, ways of transmission, drugs used for treatment, duration of treatment and causes of disability, were used in the questionnaire (see Annex).
Data from the written questionnaire were coded, entered into a computer and analyzed by frequency, percentage and the chisquared test for difference using the EPIINFO version 6.04 micro software package. Scorings for involvement, attitude and knowledge were given as 0 for a negative and 1 for a positive response. Based on seven questions the score for involvement ranged from 0-7 [not involved (0), partially involved (1-2) and involved (3-7)], while five questions for attitude ranged from 0-5 [negative (0-2), intermediate (3-4), and positive (5)], and six questions for the level of knowledge ranged from 0-6 [low (0-1), medium (2-3) and high (4-6)].
RESULTS
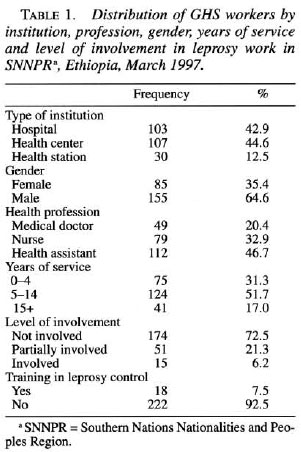
Two-hundred-forty health workers, 96% of the planned sample size, completed a written questionnaire. The proportions of doctors, nurses and health assistants were 20.4%, 32.9% and 46.7%, respectively, while that of female and males were 35.4% and 64.6%, respectively. The distribution of demographic variables as shown in Table 1 indicates a mean year of service of 8.9 years with a range of 1-30 years, and 31.3% had a working experience of less than 5 years. Among the health workers who participated in the study only 6.2% were involved in leprosy control and 7.5% obtained in-service training in leprosy. The figure of 15 (21.3%) shown on the partial involvement is mainly related to case finding and health education activities. Of the total health workers, 7.5% had had special training in leprosy.
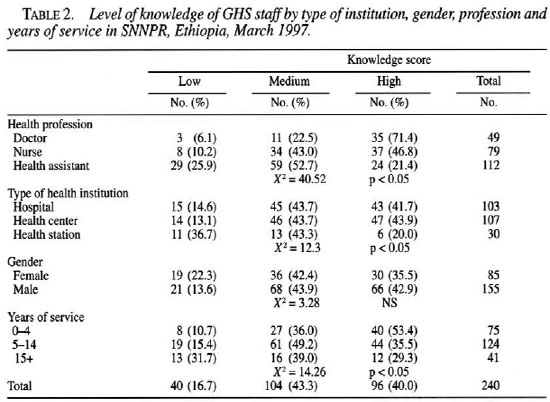
The knowledge score among all health workers resulted in 16.7%, 43.1% and 40.2% as low, medium and high level, respectively. As shown in Table 2, the level of knowledge is high in doctors and health workers with less than 5 years of experience which is significantly different when compared to other groups (p <0.05). Fifteen health workers (14 health assistants and 1 doctor) explained leprosy transmission as hereditary. All of these health assistants are working at health stations.
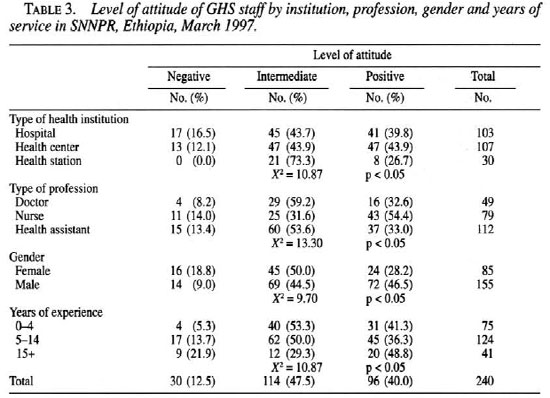
The attitude score results in 12.5%, 47.5% and 40.0% as negative, intermediate and positive level, respectively. Variation in attitude as shown in Table 3 indicated a significant difference (p <0.05) among different health institutions, professions, gender and years of experience. The level of attitude in health stations was 0% and 73.3%, negative and intermediate, respectively.
DISCUSSION
Ninety-six percent of the planned sample responded to the written questionnaire, which is enough to make conclusions and recommendations of the total planned sample size. Ten health workers (1 doctor, 1 nurse and 8 health assistants) did not participate in the study due to their continuous absence during the study time.
Only 6.2% of health workers are involved in leprosy control activities because of the lack of an integrated program in the region. The current involvement is mainly related to the participation in case finding, treatment and health education in heath institutions where monthly vertical leprosy control activities are attached. This tendency is almost similar to other areas with vertical programs.
Almost 60% of the health workers have a low-to-medium knowledge level, which can be attributed to little attention given during formal training and lack of practice after training. This shows that there is a need for increasing their level of awareness about leprosy through training for those in the GHS and incorporation of detailed leprosy education in the curricula for those in medical and paramedical schools (3,5).
Forty-seven percent of the health workers have an intermediate attitude level. This can be improved by increasing their knowledge through training, by involving them in managing leprosy patients, and by regular supervision.
The absences of a negative level and a 73.3% intermediate attitude level at health stations can be attributed to the attachment of leprosy clinics to the majority of these institutions. The high percentage of the intermediate level attitude can be improved through emphasis on in-service training.
Even though most nurses have a more positive attitude than doctors and health assistants, a further analysis by gender revealed that there are higher percentages of negative attitudes among female nurses, which can be explained by the main attachment of female nurses to hospitals where there is little activity in leprosy control.
The high level of knowledge among doctors compared to other groups may be explained by their formal training.
As the years of service increase there is an increasing tendency for a low level of knowledge and an increased negative attitude toward leprosy management (Table 3). Involving these health workers in leprosy control activities before they forget what they learned during their formal training and giving them in-service training and additional refresher courses may increase their awareness and attitude levels
In conclusion, the overall results showed a lower level of involvement of the GHS staff in the management of leprosy patients, which is mainly associated with the isolated structure for the leprosy control program and a lack of training. Therefore, leprosy work should be integrated gradually into the GHS so as to increase accessibility, improve case detection, and decrease disability rates supported by a clear policy for all groups involved in each different activity. As part of the integration process, inservice training using the existing, experienced, vertical program staff should be organized to increase the practical knowledge and overcome some of the negative attitudes toward leprosy work. In addition, for the management of difficult cases/complications and rehabilitation some service providers should take special training. These service providers can be linked to referral facilities where specialized services (not vertical) are delivered. In the long run, more emphasis should be given to leprosy work in teaching institutions during the basic training of health workers. For the successful implementation of the integration, all these activities should be followed up by regular supervision.
Acknowledgment. We would like to thank NSL for financial support, KIT for technical assistance and ALERT for institutional support. The authors would like to acknowledge Dr. Pieter Feenstra who reviewed the paper and encouraged its publication. Finally, our gratitude is extended to the Ethiopian Ministry of Health officials at different levels, respondents of the questionnaire, research assistants, and the Southern Region Health Bureau for their continuous support throughout the study.
REFERENCES
1. Becx-Bleumink, M. New developments in ALERT Leprosy Control Program and the issue of integration. Ethiop. J. Health Develop. 1(1984)49-55.
2. Feenstra, P. Leprosy control through general health services and/or combined programs. Lepr. Rev. 64(1993)89-96.
3. Feenstra, P. Sustainability of leprosy control services in low endemic situations. Trop. Geogr. Med. 46(1994)65-71.
4. Roos, B., van Brakel, W. H. and Chaurasia, A. K. Integration of leprosy control into basic health services; an example from Nepal. Int. J. Lepr. 63(1995)422-429.
5. Warndorff, D. K. and Warndorff, J. A. Leprosy control in Zimbabwe; from a vertical to a horizontal program. Lepr. Rev. 61(1990)183-187.
6. World Health Organization. A guide to eliminating leprosy as a public health problem. Geneva: World Health Organization, 1995.
7. World Health Organization. Wkly. Epidemiol. Rec. 1993.
1. M.D., M.P.H., Pathfinder International, Addis Ababa, Ethiopia.
2. M.D., SNNPR., Tuberculosis, Leprosy and Blindness Control Program Coordinator, Awassa, Ethiopia.
3. B.Sc., M.Sc., Head, Planning Department, Ethiopian Health and Nutrition Research Institute, Addis Ababa, Ethiopia.
4. M.D., Former SNNPR Tuberculosis, Leprosy and Blindness Control Program Coordinator, Awassa, Ethiopia.
5. M.D., Tuberculosis Control Program Coordinator, Shshemene General Hospital, Shshemene, Ethiopia.
Reprint requests to Dr. Mengistu Asnake, P. O. Box 12655, Addis Ababa, Ethiopia or e-mail: Masanake@pathfind.org
Received for publication on 24 September 1998.
Accepted for publication in revised forni on 23 August 2000.
*This study is dedicated to Dr. Melesse W/Dawit. He died unexpectedly on October 26,1998 from an accident. Melesse was one of the investigators for this study. A profound professional, he obtained his M.D. in 1984 from Donska State Medical Faculty, former U.S.S.R., and worked in several levels of the Ministry of Health in Ethiopia. He played a major role in integrating leprosy into the GHS by participating in several working groups at the national and regional levels.
ANNEX
QUESTIONNAIRE FOR GENERAL HEALTH SERVICE STAFF IN LEPROSY PATIENT MANAGEMENT INTRODUCTION: The following questions are used to get ideas on the involvement of the general health service staff on leprosy patient management. Therefore, please fill the answers on the boxes and spaces given for each question. Your answers and suggestions are quite valuable and confidential.
Study number: 
1. Name of health institution
 Hospital
Hospital
 Health Center
Health Center
 Health Station
Health Station
2. Health Profession
 Medical Doctor
Medical Doctor
 Nurse
Nurse
 Health Assistant
Health Assistant
3. Years of service  years
years

LEVEL OF INVOLVEMENT
5. Are you envolved in the management of leprosy?
ATITUDE
6. Is it possible to manage leprosy like any other disease in the general health service?
__ Yes __ No
7. Are you willing to be involved in diagnosing leprosy cases at your health institution?
__ Yes __ No
8. Are you willing to treat leprosy patients?
__ Yes __ No
9. Are you willing to manage leprosy patients with deformities or ulcers?
__ Yes __ No
10. Are you willing to trace patients who do not come for treatment?
__ Yes __ No
KNOWLEDGE
11. Which of the following are cardinal signs of leprosy? (more than one answer is possible)
a. Anesthetic skin lesions
b. Ulcer
c. Enlarged and/or tender peripheral nerves
d. Deformities
e. Presence of M. leprae
12. What are the possible ways of transmission of leprosy?
13. What are the three drugs used for treatment of leprosy?
1. 
2. 
3. 
14. What is the maximum duration of treatment in multibacillary leprosy?
15. Is leprosy curable? __ Yes __ No
16. What is/are the possible causes of disabilities in leprosy?
a. Long duration of treatment with MDT
b. Hereditary cause
c. Variation of body defense
d. None of the above
TRAINING
17. Did you receive special training on leprosy? __ Yes __ No
If yes, where? When? For how long?
18. Would you need additional training if you were to be involved in leprosy control?
__ Yes __ No
19. Comments/Suggestions: Regarding the involvement of GHS staff in leprosy management
Date: 