- Volume 68 , Number 3
- Page: 267–71
Histoid, a clinical variant of multibaciilary leprosy: report from so-cailed nonendemic areas
ABSTRACT
This is a hospital-based study of 25 biopsy-proven cases of histoid leprosy in the arid, northwest Rajasthan region of India. Over an 11 -year span, a total of 893 new cases of leprosy were diagnosed at our institution. These 25 histoid cases thus make up 2.8% of our new patients. Various clinical and laboratory observations are summarized and compared to other published series.RÉSUMÉ
Cet article présente une étude basé sur un hôpital de 25 cas de lèpre histioïde prouvée par examen histopathologique provenant du Rajasthan, une région aride du nord-ouest de l'Inde, à partir d'un centre hospitalier. Durant une période de 11 années, le diagnostic de lèpre, dans notre institution, totalisait 893 nouveau cas. Parmi eux, 25 cas étaient histoïdes, ce qui représente 2,8% de ces nouveau patients. Diverses observations cliniques et des données de laboratoire sont présentées et comparées aux séries déjà rapportées dans la littérature.RESUMEN
Este es un estúdio de 25 casos de lepra histioide realizado en un hospital situado en la árida region nor-occidental de Rajasthan en la India. A lo largo de 11 anos se han diagnosticado 893 casos nuevos de lepra en nuestra institución. Estos 25 casos de lapra histiode constituyen el 2.8% de los casos nuevos estudiados. En este reporte se resumen varias observaciones clínicas y de laboratorio y nuestros resultados se comparan con los de otras series publicadas.Histoid leprosy is a clinical expression of multibaciilary (MB) leprosy characterized by the occurrence of cutaneous and subcutaneous nodules and plaques with a distinctive histopathology (9). It was first described by Wade in 1960 (12). Since then there have been many reports with variable findings (2,5,6). The appearance of histoid lepromatous leprosy in children has also been reported (Ramanujam, K. and Ramu, G. Histoid variety of nodular-lepromatous leprosy-report of a clinicopathological study with follow up under treatment. Presented at the First Asian Congress on Dermatology, 1970.).
It has been reported to the extent of causing public health concern. So far, there has been no report exclusively on this entity from arid northwest Rajasthan, a so called nonendemic area for leprosy in India. The present paper records a detailed clinicopathological evaluation of 25 biopsy- proven cases of histoid leprosy in the arid northwest Rajasthan region of India.
MATERIALS AND METHODS
This study included 25 biopsy-proven cases of histoid leprosy who had attended or were attending the Department of Skin, STD, and Leprosy, Dr. Sampurnanand Medical College, Jodhpur, India, between January 1984 and December 1995. A detailed clinical history including age, sex, education, duration of disease, previous treatment taken, family history of contact, history of residence in endemic areas of leprosy, mode of development of the disease and domiciliary status of the patient, was taken. Clinical examination included the type, number and site of lesions, type of the disease and the neural involvement. For the retrospective cases, information was collected from the leprosy cards maintained for permanent records in our Urban Leprosy Clinic.
The bacteriologic and morphologic indices (BI and MI) were calculated for the slit-skin smears prepared from the histoid lesions and surrounding skin, both before and after 6 months of treatment. Hematoxylin and eosin (H&E)- and Ziehl-Neelsen- stained sections of the skin biopsy taken from the lesions were studied to establish the histopathological and bacteriological features. An ELISA for HIV screening was also carried out. The BI, MI, ELISA and detailed histopathological examination were performed for 12 new (prospective) cases only. All of the patients were put on multidrug therapy recommended by the World Health Organization (WHO/MDT) for multibaciilary (MB) leprosy.
Slit-skin smears were obtained by standard methods (4,9) from the softening center of the nodules of the prospective cases, both before and after 6 months of MDT, stained by standard Ziehl-Neelsen staining and revealed an abundance of acid-fast bacilli (AFB) intracellularly stuffing the cell as well-preserved, uniformly stained, long rods with tapering ends, longer than ordinarily seen leprosy bacilli.
RESULTS
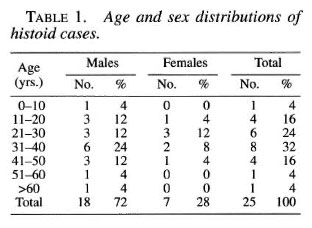
During the study period of 11 years, 893 new cases of leprosy had been registered in our leprosy clinic, and of them, 25 were cases of histoid leprosy; thus, the incidence of histoid leprosy among the leprosy patients was 2.79%.
The youngest patient was an 8-year-old male child; the oldest, a 72-year-old male (Table 1). There were 18 (72%) males and 7 (28%) females; thus, the male-to-female ratio was 2.57:1. Fourteen (56%) cases were between the ages of 21 and 40 years. Thirteen (52%) cases were previously untreated; 10 (40%) cases were irregularly treated for a duration ranging from 6 months to 5 years, and 2 (8%) cases were regularly treated with the duration of treatment ranging from 2 to 7 years. The mode of development in 17 (68%) was de novo and only 8 (32%) cases had transformed from other types of leprosy: 5 from lepro- matous (LL), 2 from borderline leproma- tous (BL) and 1 from mid-borderline (BB).
The majority (18; 72%) of the cases were residents of Rajasthan, 3 of whom had a history of staying out of Rajasthan in endemic areas (2 in South India and 1 in Bombay) for periods varying from 1 to 5 years. Seven (28%) were residents of other endemic states, including Bihar, Maharashtra and Ut- tar Pradesh (cases from Rajasthan were mainly from Jodhpur, Barmer and other neighboring districts). Sixteen (64%) cases were illiterate, another 6 (24%) had had a primary education, and only 3 (12%) had had higher education. The occupation of the cases in decreasing order of frequency was: farming, laborer, housewife, serviceman, student and semiskilled worker. Five (20%) cases had a history of contact in the family; two cases had more than one contact in the family. The contacts were father, mother, brother, uncle and niece. The type of leprosy in the contacts was LL in five and histoid and BL in one each. The duration of disease in contacts ranged from 1 to 20 years; in patients from 4 months to 6 years.
The BI and MI were analyzed in all these 12 prospective cases and results were as follows: a) The BI ranged from 2+ to 6+ in histoid lesions with a mean of 3.5+. However, in the surrounding normal skin the precise index could not be assessed accurately due to the paucity of the intracellular organisms, b) The MI of the histoid lesions varied from 41% to 90% with a mean of 69.5%; the MI of surrounding normal skin adjacent to the lesion could be analyzed even with a paucity of cells and ranged from 1% to 2%. c) The histopathological criteria as discussed by Sehgal and Srivas- tava (9) and Wade (11) were carefully followed for the diagnosis of all cases of histoid leprosy. Circumscription of histoid granuloma, the predominance of spindle cells and/or polygonal cells with a heavy density of AFB were among the major features.
In dermal or subcutaneous locations of a lesion, generally a pseudo-capsule surrounding the lesion formed by compression of the peripheral tissue of an expanding lesion was seen, and most cases showed a free subepidermal grenz zone (Fig. 1).
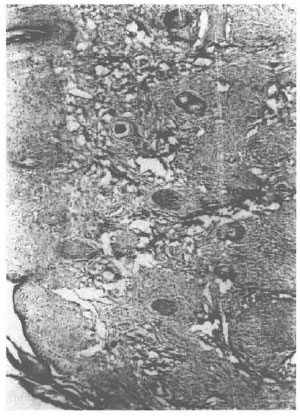
Fig. 1. Photomicrograph showing diffusely dispersed circumscribed nodular, cellular histiocytoidspindled cells in the dermis (H&E x40).
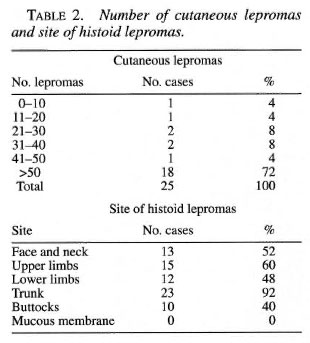
The histoid lepromas varied in number from 10 to uncountable; 18 (72%) cases had more than 50 lesions (Table 2). In 18 (72%) cases the lesions were only cutaneous nodules, and in seven (28%) the cutaneous nodules were present either with subcutaneous nodules or plaques. The cutaneous nodules were firm, shiny, stretched and situated over normal-looking skin. The lesions were situated on the trunk in 23 (92%) cases followed by upper limbs in 15 (60%), face in 13 (52%), lower limbs in 12 (48%) and buttocks in 10 (40%) (Table 2). Mucous membranes were not involved in any case but epistaxis was found in 14 (56%) cases. Nodules were present on the earlobes in only one case. The number of the lesions in a majority of cases (18; 72%) were more than 50, a finding inconsistent with Sehgal (7) whose cases with similar observations were only two (4%). The lesions were most commonly found on the trunk; whereas in a study by Sehgal (7) the most common site involved was the buttocks. However, the most common type of lesion in all the previous studies were cutaneous nodules. Most of the patients were of a lower socioeconomic group, a finding indicated by their occupation and education.
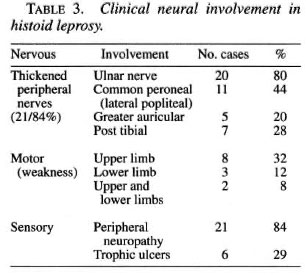
The history of five (20%) contacts within the family was quite high compared to 5% and 8% in other studies (1,7). Neural involvement in 21 (84%) and the occurrence of epistaxis in 14 (56%) were quite common in histoid leprosy. Erythema nodosum leprosum (ENL) in two (8%) cases was also not rare, unlike that observed earlier by Wade (11).
The confirming feature of histoid leprosy is, however, slit-skin smear examination which shows the abundance of uniformly stained AFB occurring equally singly, in clusters, or in globi.
Pertaining to our observations on the MI, ranging from 41% to 90%, 58.3% of the cases had an MI greater than 80%. After 6 months of treatment the MI decreased to less than 40% in all the cases and in eight (66.7%) cases it became 30%. These observations are in close agreement with earlier studies of Sehgal (7) in which the MI ranged from 46% to 90% and Singh, et al (,0) who reported an MI range of 20%-70%.
Histopathological examination revealed circumscribed spindle-shaped cells arranged in criss-cross or whorled patterns with many bacilli in all the cases (Figs. 1-3). The initial evaluation of the BI of histoid nodules revealed a range of 2+ to 6+ and after 6 months of treatment ranged from 2+ to 3+, which is in fair agreement with the earlier studies of Singh, et al. (10) and Sehgal (7). However, the studies of Bhutani, et al. (1) and Wade (11) showed a lowered BI in histoid leprosy cases.
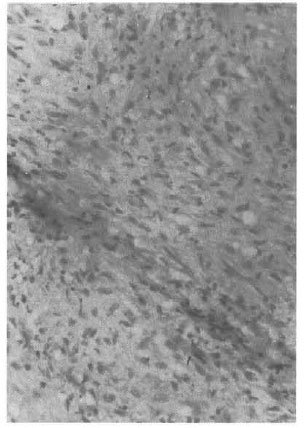
Fig. 2. Cytomorphological details of fibroblast like spindled histiocytes as predominant cellular com-ponent of histoid granuloma (H&E x80).
Fig. 3. Histiocytes studded with acid-fast bacilli (Ziehl-Neelsen stain x 100 ou immersion).
The slit-skin smear examination and the histopathological observations in all 25 cases in our study conformed with the characteristic histology of histoid granuloma. While there is a lowered immunity in histoid leprosy, an ELISA carried out for HIV screening was negative in all 12 cases. All cases responded very well to WHO/MDT. None of the cases who had completed 2 years of WHO/MDT showed any relapse in the follow-up period.
DISCUSSION
The present hospital-based study of clinically, bacteriologically and histopathologically confirmed cases of histoid leprosy revealed the incidence of histoid leprosy in this part of Rajasthan as 2.79%, in close agreement with the incidence data for other regions of India (7). There was a male preponderance, and adults between the ages of 21 and 40 were most commonly affected, as was also observed by Bhutani, et al (1), Singh, et al. (10) and Sehgal and Srivastava (8). The youngest patient reported so far is a 10-year-old child (3), but our study records a still younger patient of histoid leprosy. The male predominance could probably be due to increased chance of exposure to infectious cases at the workplace and while travelling.
A majority (13; 52%) of the cases were previously untreated, and the mode of development in 17 (68%) was de novo occurrence. These findings suggest that histoid leprosy may not necessarily be due to drug resistance, as has been previously postulated.
Ten (40%) patients had normal-looking facies, 10 (40%) had histoid facies which included the presence of nodules on the face, and 7 (28%) had facies with relics of LL, including infiltration, loss of eyebrows and depressed nose. Peripheral nerves were thickened in 21 (84%) cases; the majority of the cases had multiple nerve involvement. The ulnar nerve was the most common nerve involved in 20 (80%) cases (Table 3). Nerve tenderness was present in five (20%) cases. ENL was observed in two (8.0%) cases; one developed it after 6 months of treatment, the other after 1 year of therapy.
Slit-skin smear examination of the lesions showed numerous solid-staining bacilli. The BI of the histoid nodules before treatment ranged from 2+ to 6+. The MI of the cases before treatment ranged from 41%-90%, and it was greater than 80% in seven (58.3%) prospective cases. These observations in histoid leprosy are in close agreement with the observations of earlier workers (7).
Evaluation of histopathological criteria were very carefully observed in all cases and were precisely categorized based on the criteria laid down by Sehgal and Srivastava (9) and Wade (11). The histopathological examination of the H&E- and Ziehl-Neelsen- stained sections revealed complete circumscription of the dermal granulomas in 10 (83.3%) cases with a pseudocapsule formation in 8 (66.7%), 2 cases (16.6%) showed irregular connective tissue septae. The overlying epidermis was normal and intact in five (41.7%) and atrophic in seven (58.3%) cases. There was a free subepidermal zone in two (16.7%) cases. Spindle cells, which are a hallmark of histoid leprosy, were seen in 12 (100%) cases; in addition, polygonal cells were seen in three (25%) and foamy macrophages in five (41.7%) cases. The Ziehl-Neelsen-stained sections showed an abundance of uniformly stained long bacilli, both intra- and extra-cellularly.
In four (33.3%) sections, bacilli were present in histoid habitus, i.e., either singly or in groups along the long axis of the cell; in four sections (33.3%) the bacilli were present predominantly as globi and in the remaining four (33.3%) were present as both. Similar histopathological observations with minor variations have been observed by earlier workers (5,8,9,11,12).
REFERENCES
1. Bhutani, L. K., Bedi, T. R., Malhotra, Y. K., Kandhari, K. C. and Deo, M. G. Histoid leprosy in North India. Int. J. Lepr. 42(1974)174-181.
2. Malik, R., Khandpur, R., Chandra, K. and Singh, R. A. Clinico-pathological study of 244 cases of leprosy with special reference to histoid variety. Lepr. India 43(1977)400-405.
3. Price, E. W. and Fitzherbert, H. Histoid(high resistance)lepromatous leprosy. Int. J. Lepr. 34(1966)367-374.
4. Ramanujam, K. and Ramu, G. Wade's histoid lepromatous leprosy; report of a clinical study. Lepr. India 41(1966)293-297.
5. Ramos-Caro, F. A. Histoid lepromas. Cutis 30(1982)108-131.
6. Salodkar, A. D. and Kalla, G. A clinico-epidemio- logical study of leprosy in arid northwest Rajasthan, Jodhpur. Indian J. Lepr. 62(1995)161-166.
7. Sehgal, V. N. Histoid Leprosy. 2nd edn. New Delhi: Jaypee Brothers, 1993, pp. 3,6,14.
8. Sehgal, V. N. and Srivastava, G. Histoid leprosy-a prospective diagnostic study in 38 patients. Dermatológica 111(1988)212-217.
9. Sehgal, V. N. and Srivastava, G. Status of histoid leprosy-a clinical, bacteriological, histopathological and immunological appraisal. J. Dermatol. (Tokyo)14(1987)38-42.
10. Singh, V. V., Singh, G., Kaur, P. and Pandey, S. S. Histoid leprosy in Varanasi. Indian J. Dermatol. Venererol. Leprol. 49(1983)160-161.
11. Wade, H. W. Histoid variety of lepromatous leprosy. Int. J. Lepr. 31(1963)129-142.
12. Wade, H. W. The histoid leproma.(Abstract)Int. J. Lepr. 28(1960)469.
1. M.D., M.N.A.M.S., Professor and Head.
2. Senior Resident, Department of Skin, V.D.& Leprosy.
3. Professor and Head, Department of Pathology, Dr. S. N. Medical College, Jodhpur, India.
Reprint requests to Prof. G. Kalla, F4-12 Sugyajan,Jodhpur 342 003, India.
Received for publication on 12 January 1999.
Accepted for publication in revised form on 1 August 2000.