- Volume 68 , Number 3
- Page: 330–1
Childhood leprosy in Chandigarh; clinico-histopathological correlation
To the Editor:
Clinical features of leprosy in children may sometimes be confusing. Sensory testing is difficult in them and slit-skin smears (SSS) are usually negative (10). Histopathology may be unrewarding in early tuberculoid and indeterminate leprosy, and there may be a marked disparity between the clinical and histopathological features (7). It has been suggested that the clinical spectrum of leprosy is incomplete in the 0-14 year age group since most of the cases are indeterminate (I), tuberculoid (TT), borderline tuberculoid (BT), or mid-borderline (BB) and very few are borderline lepromatous (BL) or lepromatous (LL) (9). This study was carried out to define the histological spectrum of leprosy in children and to correlate it with the clinical spectrum.
From January 1990 to July 1999, we diagnosed 1360 new cases of leprosy. Of these, 61 (4.5%) were children in the age group 0-14 years. There were 40 males and 21 females with a M : F ratio of 1.9:1. Diagnosis in each case was established on the basis of a thorough clinical examination, histopathology and determination of bactériologie status by SSS from appropriate sites. A clinical diagnosis of I was made in 4 (6.6%) children, BT in 48 (78.7%), BL in 5 (8.2%), LL in 3 (4.9%) and pure neuritic in 1 (1.6%) child (The Table). Clinically there was no child with TT or BB disease.
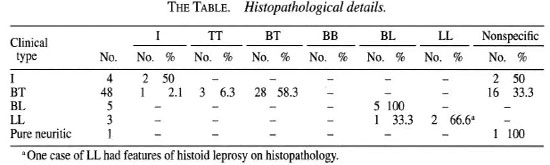
A skin biopsy was taken from the most representative lesion and stained with routine hematoxylin and eosin (H&E) and FiteFaraco stains. Histopathological findings were assessed according to the criteria laid down by Ridley (3). A clinico-histopathological correlation could be established in only 37 (60.6%) cases (The Table). Positive correlation was found in 2 (50%) cases with I, 28 (58.3%) with BT, 5 (100%) with BL and 2 (66.6%) with LL leprosy. Thus, a positive clinico-histopathological correlation was better noted in the more infiltrated lesions of BT and BL disease in comparison with the less infiltrated lesions of indeterminate leprosy. Three (6.3%) cases clinically diagnosed as BT leprosy were TT on histopathology and 1 (2.1%) case was I. One (33.3%) case of LL was BL and 1 (33.3%) was histoid leprosy on histopathology. Nonspecific features were seen in 19 (31.1%) cases-2 (50%) with I, 16 (33.3%) with BT and 1 (100%) case of pure neuritic leprosy in which a skin biopsy was taken from the area of sensory loss. Since the formation of a granuloma is indicative of good immunity (4), nonspecific features in as high as 19 cases reflect the poor immune system in children. Fite-Faraco stain was positive for acid-fast bacilli (AFB) in 7 (11.5%) skin biopsies-5 with BL and 2 with LL leprosy.
A discrepancy in clinical and histological parameters has been reported earlier in adults as well as in children (5-8). Sehgal and Joginder (5) have shown a positive clinico-pathological correlation only in 13/25 (52%) children in their series. Recently, it has been suggested that selection of the site for biopsy plays an important role in the histopathological diagnosis since clinically dissimilar lesions biopsied from the same patient can show different types of histopathology (2). This is unlikely to be responsible for the discrepancy in the clinical and histopathological diagnosis noted in children because they generally have only a few lesions and there is usually no difficulty in choosing the right lesion for biopsy.
Since we already know that indeterminate (I) leprosy can be a precursor of LL disease (1), it is important that we diagnose leprosy in children at an early stage. Our findings reiterate that clinical diagnosis still remains the mainstay for the detection of leprosy in children but, in certain situations, histopathology may help.
- Bhushan Kumar, M.D., N.N.A.M.S.
Ranju Rani, M.D.
Inderjeet Kaur, M.D., M.N.A.M.S.
Department of Dermatology, Venereology and Leprology
Postgraduate Institute of Medical Education and Research
Chandigarh 160 012, India
REFERENCES
1. Job, C. K., Baskaran, B., Joseph, J. and Aschhoff, M. Histopathologic evidence to show that indeterminate leprosy may be a primary lesion of the disease. Int. J. Lepr. 65 (1997)443-49.
2. Nadkarni, N. S. and Rege, V. L. Significance of histopathological classification in leprosy. Indian J. Lepr. 70(1999)325-332.
3. Ridley, D. S, Pathogenesis of Leprosy and Related Diseases. London: Butterworth & Co. Ltd., 1988, p. 97.
4. Robbins, S. L. and Kumar, B. Basic Pathology: Inflammation and Repair. Philadelphia: W. B. Saunders Company, 1987, pp. 28-61.
5. Sehgal, V, N. and Joginder. Leprosy in children: correlation of clinical, histopathological, bacteriological and immunological parameters. Lepr. Rev. 60(1989)202-205.
6. Sehgal, V. N., Korrane, R. V., Nayyar, M. and Sexena, H. M. K. Application of clinical and histopathological classification of leprosy. Dermatológica 161(1980)93-96.
7. Sehgal, V. N., Korrane, R. V. and Sehgal, S. Correlation of morphological, bacteriological, histopathological and immunological features of leprosy. J. Dermatol. 12(1985)243-250.
8. Sehgal, V. N., Rege, V. L. and Reys, M. Correlations between clinical, bacteriological and histopathological classification of leprosy. Int. J. Lepr. 45(1977)278-280.
9. Sehgal, V. N. and Sehgal, S. Leprosy in young urban children. Int. J. Dermatol. 27(1988)112-114.
10. Sehgal, V. N. and Srivastava, G. Leprosy in children.(Review). Int. J. Dermatol. 26 (1987)557-566.
Reprint requests to Dr. Kumar at the above address or FAX 91-0172-744401; email: kumarbhushan@hotmail.com