- Volume 68 , Number 4
- Page: 417–25
Lucio's phenomenon: clinical and therapeutic aspects
ABSTRACT
We report four cases of necrotizing reactions of the Lucio's phenomenon type, an entity rarely observed in Brazil despite the high prevalence of leprosy. Clinical, histopathological and therapeutic aspects are described and compared to those reported in the literature for cases classified as diffuse, non-nodular lepromatous leprosy with Lucio's phenomenon.RÉSUMÉ
Nous rapportons quatre cas de réactions nécrosantes associées au phénomène de Lucio, une entité rarement rencontrée au Brésil en dépit d'une haute prévalence de lèpre. Les aspects cliniques, histo-pathologiques et thérapeutiques sont décrits et comparés à ceux rapportés dans la littérature de cas classés comme lèpre lépromateuse diffuse non nodulaire avec phénomène de Lucio.RESUMEN
Reportamos 4 casos de lepra con reacciones necrotizante tipo fenómeno de Lucio, una entidad raramente observada en Brasil no obstante la elevada prevalencia de la enfermedad. Se describen los aspectos clínicos, histopatológicos y terapéuticos de estos casos y se comparon con los reportados en la literatura sobre lepra lepromatosa difusa y fenómeno de Lucio.In 1852, Lucio and Alvarado described a necrotizing skin reaction associated with non-nodular diffuse leprosy. This reaction was later denoted by Latapi and Zamora in 1948 as Lucio's phenomenon after the identification of histopathological changes involving multiple, acute and necrotizing cutaneous vasculitis peculiar to pure and primitive diffuse leprosy (PPDL) (8, 9). Lucio's phenomenon is considered to be a type of leprosy reaction associated with necrosis of the arterioles whose endothelium is massively invaded by Mycobacterium leprae (10, 18).
Lucio's-Latapi leprosy and Lucio's phenomenon, common in Mexico and Central America but infrequent in other parts of the world (12, 20), have been assigned to the pole of high susceptibility to the bacillus. In Brazil, the prevalence of leprosy has been decreasing but is still high, with rates of 4.88 per 10,000 inhabitants in 1998 (Ministerio da Saude/Secretaria de Politicas de Saude/Departamento de Gestao de Politicas Strategicas. Relatorio de atividades da area tenica de Dermatologia Sanitaria. Ano de 1999; Brasilia, dezembro 1999), and with the country occupying second place in the world in number of cases. However, reports of Lucio's phenomenon are rare (4, 5, 12, 14). Genetic and regional factors and factors peculiar to M. leprae have been implicated as probable determinants of the etiopathogeny of these clinical manifestations (8, 9, 12, 20).
We report here a clinical description and the evolution of four cases of Lucio's phenomenon observed at the Service of Dermatology of the University Hospital, Faculty of Medicine of Ribeirão Preto, Brazil.
CASE REPORTS
Case 1. A 45-year-old male patient had been presenting with recurrent ulcerated lesions on the legs for 4 years. The lesions were treated with topical and systemic antibiotics. After a diagnosis of vasculopathy, he had been submitted 1 year before to left lumbar probable sympathectomy with no therapeutic success. He reported the reappearance of the ulcers 15 days before, extensively involving the lower and upper extremities, and related the worsening of the picture to the use of penicillin. He lived with a brother who was under treatment for leprosy. On the occasion of a hospitalization prior to his transfer to our service, the patient received a diagnosis of vasculitis probably caused by an infection or by medication and was treated with systemic antibiotics (clindamycin and lincomycin) as well as high doses of hydrocortisone (900-1200 mg/day/3 days).
Case 2. A 51-year-old male patient irregularly followed up at the hospital service reported epistaxis and recurrent sinusitis associated with destruction of the nasal cartilage of 2 years' duration. He also presented with nummular ulcers with hematic crusts on the legs, as well as atrophic hyperchromic lesions. During hospitalization for the treatment of an episode of sinusitis with ampicillin (4 g/day), the patient presented with a sudden worsening of skin ulcers and the onset of countless new lesions.
Case 3. A 65-year-old male patient with recurrent ulcers on the lower limbs for the last 20 years came to our service after the lesions had started to involve the thighs, buttocks, arms, shoulders and ears 15 days before. When hospitalized before being transferred to our service, he was treated with cephalothin (4 g/day) and prednisone (60 mg/day) for 6 days.
Case 4. A 45-year-old female reported fever and inflammatory signs on the right leg which were treated as erysipelas with penicillin. During this period she noted the progressive onset of lesions that became ulcerated, gradually involving the limbs in an ascending manner. Twenty years before she had abandoned treatment for leprosy after 2 years.
The initial physical examination revealed patients in regular general condition, with mild-to-moderate pallor, and absent or intermittent fever as in Cases 3 and 4. Dermatologic examination revealed madarosis, infiltration and mild-to-moderate erythema diffusely involving extensive areas of the trunk and limbs in addition to the face and earlobes. No nodules were observed in these patients. There were numerous, sharply marginated, reticulated, angular or jagged purpuric lesions which extended to form plaques and progressed to extensive ulcers covered with necrotic tissue (Figs. 1B and 1D). These lesions predominated in the upper and lower limbs, ascendingly and progressively involving the area from the extremities to the gluteal region, and even involving the genitals as observed in Case 3 who presented lesions of the scrotal and penile region. Similar lesions were present on the ears, although in much smaller numbers (Fig. 1A). Cases 1 and 3 presented with intense hand and foot edema and necrotic toes (Fig. 1C). Necrosis, ulceration and a purulent exudate were superimposed on several purpuric plaques, especially on the hands, legs and feet.
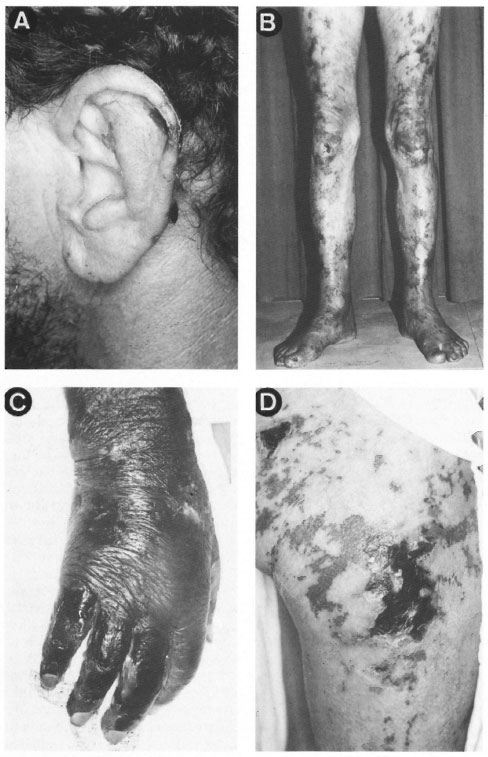
Fig. 1. Dermatological features observed in patients with Lucio's phenomenon: A = Ears showing necrotic-purpuric tissue in Case 1; B = lenticular and coalescent reticular purpuric lesions involving the lower limbs in an ascending manner in Case 2; C = marked edema of right hand with extensive necrotic tissue in Case 3; D = numerous sharply marginated, reticulated, angular or jagged purpuric plaques and necrotic ulcers on the thigh in Case 4.
Rare hemorrhagic blisters and nummular atrophic-cicatricial lesions, mainly occurring on the extremities, were observed together with generalized skin atrophy and xerosis in Case 2, as well as nasal collapse.
Neurologic examination showed symmetrical thickening, especially of the ulnar (cubital), common peroneal (popliteal) and greater auricular nerves. This alteration was accompanied by mild-to-moderate disorders of sensitivity on the distal extremities as well as mild atrophy of the thenar and hypothenar region.
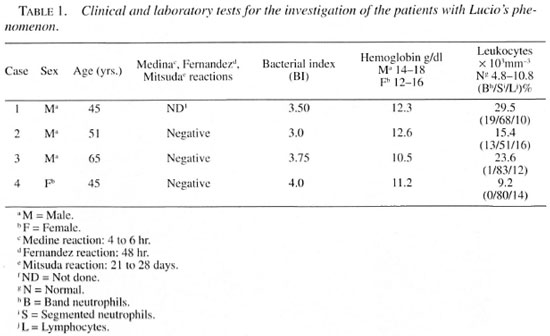
As shown in Table 1, investigation by complementary tests revealed positive bacilloscopy of slit-skin smears collected from the ears, elbows, knees and skin lesions of all patients, with a bacterial index (BI) ranging from 3.0+ to 4.0+. Blood counts revealed leukocytosis in Cases 1, 2 and 3, and absolute neutrophilia with a leftward shift in Cases 1 and 2. Anemia was observed in all cases but was more intense in patient 3 (Hb = 10.5 mg/dl). The Mitsuda skin test was applied by inoculating 0.1 ml of an integral standard suspension containing a 6 x 106 concentration of bacilli, supplied by the Lauro de Souza Lima Institute, Brazil. Readings were taken after 4 hrand 6 hr (Medina reaction), 48 hr (Fernandez reaction), and 21 to 28 days (Mitsuda reaction) after inoculation and the lepromin skin tests were all negative, as was also the pathergy test with physiological saline.
Other tests such as serology for syphilis, anti-HIV antibodies and tuberculosis were negative. Case 4 presented increased anti-streptolysin O titers of 797 U (normal upper limit: 200 U), and negative antiphospholipid antibodies.
Histopathology. The skin histopathology of the four reported cases showed the following common features: focal necrosis of the epidermis and of the superficial and deep dermis, and a mononuclear inflammatory infiltrate rich in foamy histiocytes, associated with a variable infiltrate of polymorphonuclear leukocytes, grouped around skin adnexa, nerve fibers and blood vessels. There was necrosis of the sweat glands and of some nerve fibers in the underlying subcutaneous tissue, varying in intensity among the skin biopsies of each patient. We observed signs of ischemia, fibrinous vasculitis, and thrombosis of small arteries with a focal deposit of fibrinoid material on the wall (Figs. 2A and 2B). Fite-Faraco staining demonstrated large numbers of acid-fast bacilli (AFB) forming clumps inside the macrophages, in the areas of necrosis, in nerve fibers, and in vascular endothelium (Figs. 2C and 2D). These pathological changes confirmed the diagnosis of leprosy of the lepromatous pole associated with vasculitis of the Lucio's phenomenon type.
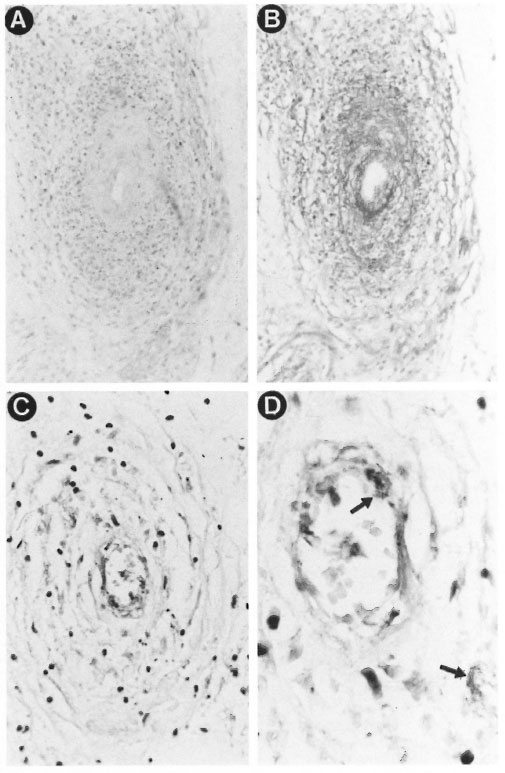
Fig. 2. Histopathological features observed in the cutaneous lesions of Lucio's phenomenon: A = Vasculitis with thickening of the vessel wall and infiltrate of mononuclear and polymorphonuclear leukocytes (H&E ×100); B = focal deposit of fibrinoid material on the vessel wall (PAS ×100); C = large numbers of acid-fast bacilli forming clumps in the vascular endothelium (Fite-Faraco ×400): I) = detail with clumps of the intact bacilli in the cytoplasm of the endothelial cells (Fite-Faraco ×1000).
Treatment. After the clinical diagnoses were established, the patients received the treatment indicated for leprosy for the control of the moderate-to-severe vasculitic process and for the concomitant infections.
The major therapeutic measures adopted in each case are summarized in Table 2. Cases 2, 3 and 4 received 50 mg of clofazimine and 100 mg of dapsone daily, and we decided to use rifampin (RPM), initially administered at the dose of 600 mg/day for 7 to 13 days, for patients 3 and 4 for the control of bacillemia and of secondary infection associated with the vasculitic process. The dose was later reduced to monthly doses of 600 mg according to the multidrug treatment schedule recommended by the World Health Organization (WHO/MDT). Ofloxacin (800 mg/day) was similarly used in Cases 1 and 3 after collection of exudate from the ulcers. Microorganisms such as Staphylococcus aureus, Pseudomonas aeruginosa, Proteus mirahilis, and Escherichia coli, among others, grew in several cultured samples; a phenomenon interpreted as a secondary infection by bacteria sensitive to the antibiotics used.
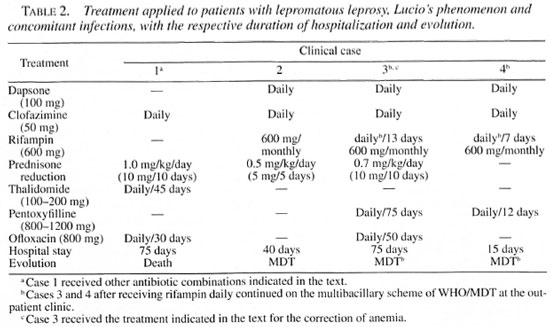
Combinations of systemic antibiotics, cephalosporins, aminoglycosides and quinolones were used sequentially for Case 1. Bacteremia by S. aureus, subsequently confirmed by blood culture in this patient, was not controlled by treatment and progressed to sepsis, possibly due to the persistence of an extensive and profound area of tissue necrosis. In contrast, Case 3 evolved satisfactorily despite a similar clinical picture of bacteremia and the associated presence of marked necrosis.
Case 4 was first treated with erythromycin (2 g/day) indicated for the continuation of treatment of erysipelas, and rifampin, dapsone and clofazimine were progressively and sequentially introduced.
Prednisone was prescribed for all patients except Case 4 at a daily dose of 0.5 mg to 1.0 mg/kg body weight, with a progressive reduction of 5-10 mg at 5-10-day intervals. Thalidomide at the dosage of 200 mg/day was used for Case I. Pentoxyfilline was indicated at the dosage of 800-1200 mg in combination with prednisone for Case 3, and alone for Case 4. Anemia, which was more marked in Case 3, was corrected with folic acid (5 mg), ferrous sulfate (250 mg) and B complex administered daily (Table 2).
Evolution. Case 1 showed progressive worsening. The vasculitis lesions progressed to deep and extensive areas of necrosis with dramatic exposure and destruction of hand and foot tendons. After 2 months, there was a clear deterioration of clinical condition with sustained fever, torpor and dyspnea, and staphylococcal septicemia was detected. The patient died with a clinical picture of uncontrollable hemorrhagic manifestations of the integument and of the digestive apparatus associated with sepsis and extensive areas of necrosis, indicative of a diagnosis of disseminated intravascular coagulation (DIC). Autopsy revealed pulmonary, renal and myocardial abscesses due to staphylococcal infection, opportunistic fungal infections of the trachea, and angio-invasive pulmonary aspergillosis, as well as lepromas of the spleen, liver and bone marrow.
Cases 2, 3 and 4 were controlled and maintained on the WHO/MDT schedule for leprosy at the outpatient clinic after discharge from the hospital. Case 2 evolved with ulcer healing and was discharged in good condition after 40 days of hospitalization, although he later appeared irregularly at the outpatient clinic. In Case 3, the intense involvement of the toes required bilateral surgical amputation of the 3rd, 4th and 5th toes. The surgical wounds and the vasculitic ulcers healed satisfactorily, and the patient was discharged after 75 days of hospitalization. In Case 4, the onset of new lesions was rapidly controlled, with consequent improvement and re-epithelialization of the ulcers. The patient was discharged after 18 days of hospitalization with only skin scars remaining in the previously involved areas.
DISCUSSION
The evolution of infection in leprosy is directly related to cell-mediated immunity, resulting in effective control of the disease in the tuberculoid (TT) form or, at the other extreme, in failure to contain bacillary multiplication and dissemination of the disease in the lepromatous (LL) form. A clinical variant of the anergic pole is Lucio-Latapi leprosy, or pure primitive diffuse leprosy (PPDL) (8, 9).
Probable genetic and climatic factors may have contributed to making Lucio-Latapi leprosy typical of the Pacific coast of Mexico (8, 9, 12, 20). Pereira, Jr. (10) commented about the correct recognition of this clinical form of the anergic pole of Lucio-Latapi leprosy which evolves without nodules and with extensive and diffuse skin involvement resulting in an infiltrated, succulent and apparently healthy aspect of the skin frequently accompanied by recurrent episodes of multiple necrotizing vasculitis represented by Lucio's phenomenon, with positivity to the Medina reaction. However, the clinical form closely similar to Lucio- Latapi leprosy with Lucio's phenomenon and a negative Medina reaction is considered to be properly designated as non-nodular diffuse leprosy.
The Medina reaction and pathergy test were negative in Cases 2, 3 and 4 (Table 1), as was also observed in the cases reported by Rea and Levan (17). Latapi and Zamora (9) emphasized the positivity to the Medina reaction and compared it to the Shwartzman-type reaction, suggesting a response of hypersensitivity to M. leprae, which may develop from probable synergic effects with cocci causing superimposed infections that would explain the similarity of the skin reactions obtained also with streptococcal and staphylococcal antigens (8, 9). This may possibly be another peculiarity of Lucio's leprosy occurring on the Pacific coast of Mexico, or a probable variability of the antigen composition of lepromin may account for the positive results of the Medina reaction reported by Latapi and Zamora (9).
The rapid and profound deterioration of these apparently healthy cases of non-nodular lepromatous leprosy, in addition to a fatal outcome, is not uncommon. Several reports have described marked and prolonged morbidity with a frequently fatal outcome, with the detection of other concomitant infections at autopsy and diffuse lepromatous leprosy involvement of various organs, such as liver, spleen, and bone marrow, similar to the first case reported here (4, 8, 11, 13).
The literature points out that patients with Lucio's phenomenon often do not receive specific treatment for leprosy, usually because of the absence of a diagnosis (6, 8, 9, 16, 17), as observed in the present series. The inverse occurs with the erythema nodosum type of reaction, more frequently observed after the first 6 months of treatment (7), suggesting a closer relationship with the presence of fragmented bacilli favored by the antibacterial treatment.
Specific treatment with sulfone usually leads to a satisfactory evolution of Lucio's phenomenon (9). Patients who are not controlled with sulfone treatment respond promptly to replacement with rifampin; whereas thalidomide does not lead directly to clinical improvement compared to the use of corticosteroids (17). Considering that thalidomide acts rapidly, improving the lesions and systemic symptoms in the erythema nodosum reactions of leprosy, this therapeutic response may contribute to the differentiation between Lucio's phenomenon and necrotizing erythema nodosum. The combination of sulfone, clofazimine and rifampin of the WHO/MDT scheme may be of rapid benefit, but it would be important to monitor the delicate equilibrium between bacillary death, the vasculitic process and the superimposed infections in addition to the control of leprosy itself.
Latapi and Zamora (9) pointed out the worsening of the vasculitis picture associated with the use of more active treatments such as antisyphilitics, iodides, and toxoids, and especially chaulmoogra, and considered this to be a Herxheimer-like crisis caused by treatment, at times requiring careful manipulation for control. This difficulty was clear in the first case reported here, despite therapeutic coverage for M. leprae, corticosteroids for vasculitis as well as the various combinations of broad spectrum antibiotics needed for the control of superimposed infections. The progression of the former vasculitis lesions, extensive and deep necrotic areas, the association of staphylococcal and opportunistic fungal infection, sepsis and DIC led to a fatal outcome. The abrupt death of the bacilli caused by the bactericidal effect of some of the antibiotics used against M. leprae may have first potentiated the vasculitic phenomenon by obstructive, inflammatory and micro-thromboembolic mechanisms at the endothelium level. We assume that the depressed specific cell immune response of the patient permitted the wide dissemination of the bacilli, which even reached endothelial cells. The rapid and massive bacillary death may also cause a Herxheimer-like phenomenon (9), if we consider the possible participation of immunocomplexes in this process due to the high bacillary antigen levels and the overproduction of specific immunoglobulins.
Microcirculatory flow may be impeded by activated platelet clumps, white blood cells, and damaged endothelium caused by massive bacillary parasitism. In this process, released vasoactive and vasoconstrictive compounds may additionally trigger the clotting cascade and microthrombosis. On the basis of the hemorheological properties and antiplatelet effects of pentoxyfilline, which result in the ability to improve the regional microcirculation especially in ischemic areas, the drug was indicated to aid the treatment of Lucio's phenomenon in Cases 3 and 4. Pentoxyfilline and its metabolites have been reported to have relevant actions at the level of blood viscosity and flow, in the mechanism of coagulation, in fibrinolysis, and to influence anti-aggregatory factors and inhibit thrombus formation. They also act on the immunomodulation of the inflammatory response, including increased neutrophil deformability and chemotaxis and decreased leukocyte adhesion to the endothelium, neutrophil degranulation and production of superoxides and of monocyte-derived tumor necrosis factor (19). All of these combined properties and the favorable clinical response suggest that pentoxyfilline is a drug of interesting application for the treatment of vasculitis of the Lucio's phenomenon type.
Fever and leukocytosis may be absent (17); however, the concomitance of extensive necrotic areas and the association with secondary infection observed in the present cases may justify these alterations. Despite the fever, the absence of the other manifestations such as painful and tender to touch skin nodules, arthritis, neuritis, iridocyclitis, etc., should be emphasized in order to aid the clinical differentiation between Lucio's phenomenon and necrotizing erythema nodosum.
The description of segmental necrotizing angiitis in Lucio's phenomenon, which first involves the lower and upper limbs in an ascending manner, and the alterations of small arteries with deposition of fibrinoid material and large numbers of AFB on the vascular endothelium observed in the present cases are similar to those reported in the literature (3, 9, 16-18, 20, 21).
In the histopathology of the cases reported here we observed a predominance of necrosis of the epidermis and dermis resulting from an ischemic process, from thrombosis of small vessels and from passive venous congestion, as well as vascular changes consisting of vessels with thickened walls, edema and partial or total occlusion of the lumen. An inflammatory infiltrate consisting of mononuclear and polymorphonuclear leukocytes surrounding the vessels and extending to the superficial, deep and subcutaneous dermis was also observed. We emphasize the presence of intact M. leprae on the vessel walls and in endothelial cells involved in the necrotic process, or in adjacent areas, possibly triggering the vasculitic process.
Although the clinical and histopathological features of Lucio's phenomenon have been described, the pathogenesis of this reaction still awaits elucidation. We suggest that in the present series the use of penicillin or its derivatives and of other potent antibiotics, as well as concomitant infections or abrupt and massive bacillary death in endothelial cells, caused the worsening and reappearance of the lesions, possibly suggesting a similarity to the observations of Latapi and Zamora (9). However, the true participation of drugs or superimposed infections and the interactions between bacillus, host and the triggering of the vasculitic reaction still remain to be established. Lucio's phenomenon may represent a unique state of hypersensitivity precipitated by nonspecific concomitant secondary infections, compared to the Shwartzman-type reaction (3, 9).
Deposits of mixed-type cryoglobulins (IgG, IgA, IgM, C3 and Clq) were observed in dermis vessels affected by vasculitis of the Lucio's phenomenon type, suggesting a mechanism mediated by deposits of immune complexes (15). Clearly, the bacillemia in endothelial cells associated with thrombotic phenomena is important, although the possible immunologic and genetic factors involved require further intense investigation (10 and Floury, el al. Poster presented at the 15th International Leprosy Congress, Orlando, Florida, U.S.A., 1993. Workshop 6: Pathology. Presented at the 15th International Leprosy Congress, Orlando, Florida, U.S.A., 1993).
A conflicting point is the involvement of large vessels, apparently an unusual occurrence in Lucio's phenomenon, resulting in extensive tissue loss and exposed tendons and in amputation of the extremities described in Cases 1 and 3, although a similar case has been reported in which there was involvement of large vessels in Lucio's phenomenon (2). Finally, in the differential diagnosis of Lucio's phenomenon, vasculitis of other origins should be considered, such as the antiphospholipid antibody thrombotic syndrome associated with lep- romatous leprosy (1). A search for antiphospholipid antibodies in our Case 4 was negative and was not performed in the other patients. The occurrence of these antibodies may be a secondary phenomenon since, except for Case 1, all other patients progressed with interruption of Lucio's phenomenon after specific treatment for leprosy, with no recurrence of the vasculitis process.
On the basis of the clinical and histopathological data documented for the present series, the patients were classified as having diffuse, non-nodular lepromatous leprosy with vasculitis of the Lucio's phenomenon type. We emphasize the rarity of Lucio's phenomenon, the differentiation from necrotizing erythema nodosum, its occurrence in the anergic pole of the disease when left untreated and of long duration, and the probable difficulty in the diagnosis of these clinical entities.
REFERENCES
1. Bakos, L., Correa, C. C., Bergmann, L., Bonamigo, R. R. and Muller, L. F. B. Antiphospholipid antibodies thrombotic syndrome misdiagnosed as Lucio's phenomenon. Int. J. Lepr. 64 (1996) 320-323.
2. Derbes, V. J., Samuels, M., Williams, O. P. and Walsh, J. J. Diffuse leprosy-case in a Louisiana Negro. Arch. Dermatol. 81 (1960) 210-224.
3. Donner, R. S. and Shively, J. A. The Lucio phenomenon in diffuse leprosy. Ann. Intern. Med. 67 (1967) 831-836.
4. Fleury, R. N. and Opromolla, D. V. A. Virchowian Hansen's disease, Lúcio's phenomenon, cryptococcoses (clinical conference). Hansenol. Int. 13 (1988) 47-56.
5. Furtado, T. A. The Alvarado form of leprosy; a case observed in Brazil. Int. J. Lepr. 27 (1959) 110-115.
6. Jopling, W. H. and Mcdougall, A. C. A doença. In: Manual de Hanseníase. São Paulo: Livraria Atheneu Editora, 1991, pp. 11-55.
7. Jopling, W. H. and Mcdougall, A. C. Reações lepróticas (estados reacionais). In: Manual de Hanseníase. São Paulo: Livraria Atheneu Editora, 1991, pp. 89-97.
8. Latapi, F. and Zamora, A. C. La lepra "manchada" de Lúcio (estúdio inicial clinico e histopatologico). In: Memória do V Congreso Internacional de la Lepra - Havana, 1948, pp. 410-413.
9. Latapi, F. and Zamora, A. C. The "spotted" Leprosy of Lucio (La lepra "manchada" de Lúcio); an introduction to its clinical and histological study. Int. J. Lepr. 16 (1948) 421-429.
10. Naafs, B. Leprosy reactions: new knowledge. Trop. Geogr. Med. 6 (1994) 80-84.
11. Obermayer, M. E., Bonar, S. C. and Rosenquist, R. Diffuse leprosy. J. Invest. Dermatol. 12 (1949) 243-248.
12. Pereira, A. C., Jr. Hanseníase de Lúcio. An. Bras. Dermatol. 68 (1993) 33-40.
13. Pursley, T. V., Jacobson, R. R. and Apisarnthanarax, P. Lucio's phenomenon. Arch. Dermatol. 116 (1980) 201-204.
14. Quinette, S. S., Marques, A. S., Rangel, E. R. and Rocha, G. L. Lepra de Lúcio. An. Bras. Dermatol. 52 (1977) 107-115.
15. Quismorio, F. P., Rea, T., Chandor, S., Levan, N. and Friou. G. Lucio's phenomenon: an immune complex deposition syndrome in lepromatous leprosy. Clin. Immunol. Immunopathol. 9 (1978) 184-193.
16. Rea, T. H. Lucio's phenomenon: an overview. Lepr. Rev. 50 (1979) 113-121.
17. Rea, T. H. and Levan, N. E. Lucio's phenomenon and diffuse non-nodular lepromatous leprosy. Arch. Dermatol. 114 (1978) 1023-1028.
18. Rea, T. H. and Ridley, D. S. Lucio's phenomenon: a comparative histological study. Int. J. Lepr. 47 (1979) 161-166.
19. Samlaska, C. P. and Winfield, E. A. Pentoxyfilline. J. Am. Acad. Dermatol. 30 (1994) 603-621.
20. Saul, A. and Novales, J. La lepre de Lucio-Latapi et le phenomene de Lúcio. Acta Leprol. 1 (1983) 115-132.
21. Turkel, S. B., Van Hale, H. M. and Rea T. H. Ultrastructure of the dermal microsvaculature in leprosy. Int. J. Lepr. 50 (1982) 164-171.
1. M.D., Ph.D.; Division of Dermatology, Department of Internal Medicine;
2. M.D., Ph.D.; Division of Dermatology, Department of Internal Medicine;
3. M.D., Ph.D., Division of Dermatology, Department of Internal Medicine;
4. M.D., Ph.D., Department of Pathology, University Hospital, Faculty of Medicine of ribeirão Preto, University of Sao Paulo, Av. Bandeirantes 3900, 14048-900 Ribeirão Preto, SP, Brazil.
Reprint request to Dra. Cacilda at the above address or FAX 55-16-633-1144; email: cacilda@usp.br
Received for publication on 7 August 2000.
Accepted for publication in revised form on 7 December 2000.