- Volume 66 , Number 1
- Page: 1–9
Delay in presentation and start of treatment in leprosy patients: a case-control study of disabled and non-disabled patients in three different settings in Ethiopia
ABSTRACT
The delay incurred by leprosy patients between the onset of symptoms and the start of treatment has not been well characterized. Because reducing this delay is likely to be the most productive of all activities aimed at preventing disability, we compared the various components of delay in disabled and nondisabled new leprosy cases in a case-control study. Disabled patients had a median overall delay of 26 months, while nondisabled patients incurred a delay of only 12 months. The total delay was divided into three components: a) the delay between the onset of symptoms and the first act of health-seeking behavior, which was significantly longer for disabled patients; b) the delay between the first action and the first visit to a recognized clinic, which was also significantly longer for disabled patients; and c) the delay between the first clinic visit and the start of treatment, which was important in some cases: in those patients whose delay was due to problems within the health services, disabled patients again had a significantly longer delay. The study also compared two rural areas of Ethiopia, one with high and one with low rates of disability in new cases. High rates of disability (and greater delay in starting treatment) were thus associated with high levels of stigma, being f rom the Christian rather than the Muslim community, and the use of traditional medicine. There was, surprisingly, no association with knowledge about the transmission, symptoms and curability of leprosy. Implications for health promotion activities are discussed.RÉSUMÉ
Le délai existant chez les malades de la lèpre entre le début des symptômes et a mise en traitement n'a pas été bien caractérisé. Parce que la réduction de ce délai est sans doute la plus efficace de toutes activités dirigées vers la prévention des incapacités, nous avons comparé les diverses composantes du délai chez des nouveaux malades avec et sans incapacités. Les malades avec incapacités avaient un délai médian de 26 mois, tandis que chez les malades sans incapacités ce délai n'était quede 12 mois. Le délai total a été divisé en trois composants: a) le délai entre le début des symptômes et la première action de recherche de soins, qui était significativement plus long pour les patients avec incapacités; b) le délai entre la première action et la première visite à une clinique reconnue, qui était aussi significativement plus long pour les patients avec incapacités; et c) le délai entre la première visite à une clinique et le début du traitement, qui était important dans certains cas: chez les patients dont le délai était dû à des problèmes au niveau des services de santé, les patients avec incapacités avaient à nouveau un délai signilicativement plus long. L'étude a aussi égions rurales d'Ethiopie, l'une avec des taux élevés d'incapacités parmi les nouveaux cas, l'autre avec des taux faibles. Les taux élevés d'incapacités (et un délai plus long avant le début du traitement) étaient donc associés à un stigma important, au fait d'être de la communauté chrétienne plutôt que de la communauté musulmane, et à l'utilisation de médicaments traditionnels. Il n'y avait, de manière surprenante, pas d'association avec les connaissances relatives à la transmission, les symptômes et la possibilité de guérir la lèpre. On discute les implications de tout cela pour les activités de promotion de la santé.RESUMEN
No está bien caracterizado el retardo entre la aparición de los sintomas en los pacientes con lepra y el inicio del tratamienlo. Debido a que la redueción en este retardo es probablemente la más productiva de las actividades orientadas a prevenir las alteraciones discapacitantes, nosotros comparamos los diferentes componentes del retardo en nuevos casos de lepra con y sin discapacidades. Los pacientes discapacitados tuvieron un retardo promedio de 26 meses, mientras que los pacientes sin discapacidad tuvieron un retardo de sólo 12 meses. El retardo total fue dividido en 3 componentes: (a) el retardo entre la aparición de los sintomas' y el primer intento de buscar ayuda médica (significativamente mayor en los pacientes discapacitados); (b) ei retardo entre Ia primera acción y Ia primera visita a una clínica reconocida (también significativamente mayor en los pacientes incapacitados), y (c) el retardo entre la primera visita a la clinica y el inicio dei tratamiento, lo cual fue importante en algunos casos: entre los pacientes cuyo retardo se debió a problemas dentro de los servicios de salud, los pacientes discapacitados fueron los que sufrieron el retardo más prolongado. El estudio también comparó dos áreas rurales de Etiopía, una con altas tasas de incapacidad entre los casos nuevos y otra con tasas bajas entre los mismos. Las tasas altas de incapacidad (y mayor retardo en el inicio del tratamiento) estuvieron asociadas con altos niveles de estigma y fueron predominantes más en la comunidad cristiana que en la musulmana y en las comunidades que hacen uso de la medicina tradicional. Sorprendentemente, no se encontró ninguna asociación con el conocimiento de la transmisión, los síntomas y la curabilidad de la enfermedad. Se discuten las implicaciones de las actividades relacionadas con la promoción la salud.Leprosy is a disease of the skin and peripheral nerves which can cause severe disability and disfigurement, leading to major social and economic problems for those affected by it. The damage to peripheral nerves often can be prevented or reversed in patients presenting early, but a significant number of cases already have irreversible nerve damage when they first come into contact with the health services. Thus, an important task in the prevention of disability (POD) is to determine the reasons why people may present late to the health services and then to design various interventions aimed at promoting early reporting and speedy diagnosis. If patients can be diagnosed at an earlier stage, it is likely that a significant amount of nerve damage could be prevented, more than could be prevented by any other intervention at a later stage (6).
In comparing different programs throughout the world, the rates of disability in new cases are important indicators of the effectiveness of case finding. Within Ethiopia, rates vary quite widely; for example, the proportion of new cases with grade 2 disability may be below 10% or above 20%.
Wrong beliefs about the disease, low awareness of modern treatment, stigma, and the influence of traditional healers or community leaders may each play an important role in the late reporting of new cases. These are complex factors and interact with each other in complex ways, but further knowledge of the importance of these and similar issues will be of help in improving health education activities and materials.
Few studies of the knowledge and attitudes of leprosy patients in Ethiopia have been done. Recently, however, a study carried out in Shoa looked into this issue (Assefa, Nash, Tefera; unpublished data, 1996). It showed that modern health service coverage and utilization in the country are at low levels (below 50%) and that traditional beliefs and practices are still widespread. They also found that patients may attend a general clinic, but then experience a delay in being referred to a leprosy clinic. A previous study in Shoa found a high degree of stigma, without much evidence of outside influence on traditional beliefs and practices (8).
MATERIALS AND METHODS
This case-control study compares three areas within Ethiopia (Hararge, in the southeastern part of the country; West Shoa, an area immediately west of the capital, Addis Ababa, and the ALERT Hospital in Addis Ababa). Disability rates for the last 10 years were reviewed. Patients attending clinics were interviewed using a pretested questionnaire. Cases were patients diagnosed between 1 January 1995 and the time of the clinic visit who had a disability grade (DG) of 2 at the time of diagnosis; controls were patients diagnosed during the same period who had a DG of 0 at diagnosis.
A total of 273 patients were included in the study; 105 cases and 168 controls from the three different areas were interviewed. One case gave such an extreme answer for the timing of his disease (a total delay of 48 years from first symptom to start of treatment) that he was excluded from the timerelated analyses.
In Hararge, patients from 45 clinics were interviewed. In West Shoa 50 clinics were visited. At ALERT, all new patients diagnosed during the course of the study in the ALERT outpatient department were examined by one of the researchers and were entered into the study if they were either cases (DG 2) or controls (DG 0). Leprosy suspects who come to ALERT are a very mixed group, coming from all over the country, seeking a variety of other forms of treatment.
Because of the fact that the ALERT patients are a very heterogeneous group, when the areas are compared statistically only the rural areas of Shoa and Hararge are compared. When cases and controls are compared, however, all patients are analyzed. Because the data are not normally distributed, the nonparametric Kruskal-Wallis method for comparing unpaired ranks was used, calculated using the computer program Epi-Info v5.1.
Quantification of various types of delay
The basis for the quantification of the different types of delay was the time line, which was part of the patient questionnaire. This is a device enabling the interviewer to document clearly the sequence and timing of the different events described by the interviewee. In this study, the timing of four specific events (as well as any other events mentioned by the patient) was noted (Fig. 1). The different periods of delay were calculated in months for analysis.
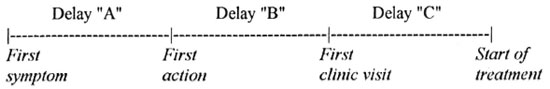
Fig 1. The time line; total delay is denoted Delay - "T"
The first symptom was noted according to the recall of the patient. The first action denotes the first act of health-seeking behavior by the patient, whether attendance at a clinic or a traditional form of treatment; it does not include discussions with family and friends or other activities, such as a change in work or dwelling, even if these are caused by the development of the disease.
The first clinic visit denotes a visit to a government or approved mission clinic where leprosy treatment may or may not be available; it does not include visits to private clinics, pharmacies or drug shops, although it was noted that these places may often correctly refer patients to the appropriate clinic. The start of treatment denotes the date of actually receiving the first dose of multidrug therapy (MDT).
RESULTS
Disability grades by area
The following rates of DG 2 in new cases have been taken from the annual reports for the last 7-10 years and averages have been calculated: Hararge 6.6%, ALERT 20.4%, and West Shoa 21.1 %. Rates for DG 1 were not compared because different methodologies to test sensation are employed in the different areas.
Description of sampled cases and controls
Table 1 describes the six study groups (cases and controls in the three areas). It can be seen that the most significant difference is in religion, with Hararge being a predominantly Muslim area and the other areas largely Christian. The Hararge sample is also less literate, older, and has a higher male: female ratio.
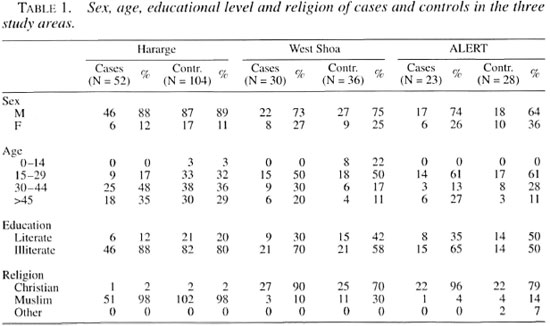
Within each area there are differences between cases and controls: thus, cases tend to be older than the controls (significant in all areas), less literate (in the ALERT sample only: p <0.05) and Christian rather than Muslim (in the ALERT and West Shoa samples only: p <0.05 and p <0,001, respectively).
Analysis of delay
Table 2 shows the total delay and the three components of delay experienced by both cases and controls. The figures from all three areas are pooled. There are highly significant differences in the delay at each stage except the last, from clinic visit to the start of MDT.
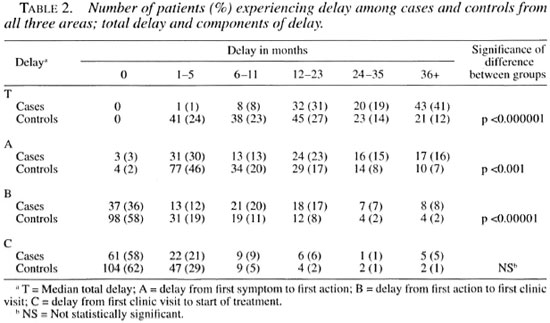
Table 3 gives the results of this comparison for each area on its own. The median values for each delay are shown to give a clearer picture than the mean, which is distorted by a few atypical values.
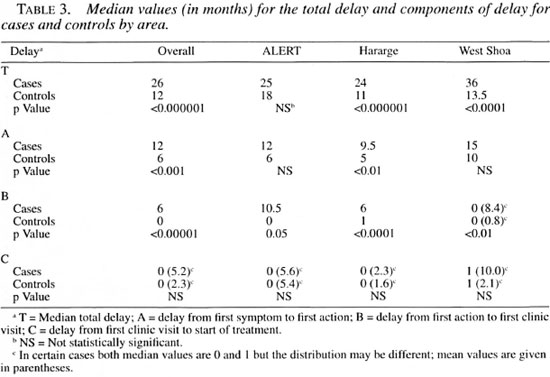
When the two rural areas (West Shoa and Hararge) are compared, it appears that, for cases, the median total delay (T) is significantly greater in Shoa (36 months) than in Hararge (24 months; p <0.01). For controls, the median total delay in West Shoa is also greater than in Hararge (13.5 versus 11 months), but this difference is not significant.
Controls in West Shoa have a higher median first component delay (A: between onset of symptoms and first action) than controls in Hararge (10 versus 5 months; p <0.005). The difference for cases (15 months in West Shoa, 9.5 months in Hararge) does not quite reach statistical significance.
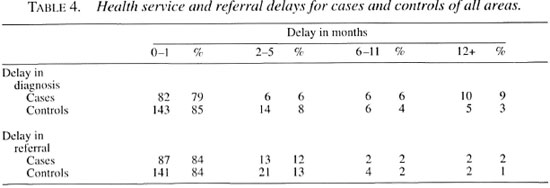
Health service delays (misdiagnosis and delays in referral)
Table 4 shows that delays due to failure to diagnose or to suspect leprosy within the health services are incurred by about 1 in every 5 patients, for both cases and controls. This is worrisome. One in every six patients takes longer than 1 month to act on months la referral for leprosy treatment; this may be the patient's own decision or it may relate to problems of access.
Case report. A 50-year-old woman first noticed an ulcer on her right foot in June
1991. She visited a nearby hospital after 3 months and was given some injections. Although these did not help, she continued toattend the same hospital for 3 years. When the ulcer became worse and she developedtypical skin patches of leprosy, she was diagnosed as a leprosy patient and started on treatment. The total delay was more than 5 years.
Case report. A 22-year-old man experienced numbness of the hands and feet and nasal blockage. After 1 year he went to a nearby hospital where he was advised to go to a leprosy clinic. However, he decided to go to a local healer who treated him for more than 1 year. After a delay of about 2 years he went to a leprosy referral hospital and was diagnosed. He was referred back to a peripheral clinic and then to another clinic before starting treatment, which added another 2 months to the delay.
Summary of delays
Figure 2 shows the components of delay for cases and controls in each of the three areas. Mean figures are used rather than the median values since the latter will not give the correct total delay. Taking all cases together, the proportion of the total delay attributable to each component is as follows: delay until first action, 53% (controls 61%); delay between first action and first clinic visit, 32% (controls 27%) and delay between first clinic visit and start of treatment, 15% (controls 12%).
Thus, disabled new cases have a significantly longer delay in presentation than those without disability. The total delay is longer (median 26 months versus 12 months), and each component of the delay (except final delay between visiting a clinic and starting treatment) is also longer. The first component of the delay, between onset of symptoms and the first action, is the major contributor to the overall delay. It is also concluded that leprosy patients, in general, present earlier in the Hararge area than in West Shoa, and that it is a difference in the first component of delay that accounts for most of the overall difference.
Reasons for delay in reporting by patients
In analyzing the data from the patient questionnaire, very few items show a significant difference between cases and controls or, in other words, suggest reasons for the delay in reporting. As mentioned earlier, cases tended to be older, less literate, and Christian. Gender was not associated with the disability grade at diagnosis. Other factors showing a difference between cases and controls are:
a) the presenting symptoms: Table 5 shows the different presenting symptoms for cases and controls. There is a significant, although clearly expected difference with controls much more likely to present with skin symptoms rather than symptoms of damage (χ 2 = 25-4< P <0.000005).
b) which action was taken as the first action: Table 6 shows the different activities performed first. Although traditional methods are widely used, a significantly greater number of controls never used traditional methods ( χ 2 = 13.9, p <0.005).
Case report: A 30-year-old woman developed numbness and ulcers on both feet in early 1992. A year later she went to a local healer and was advised to go to the nearby leprosy clinic. However, she did not do this but went to another clinic where she got some injections. After more than 2 years, she went back to the same local healer from whom she had received the same advice. This time she went to the leprosy clinic and started treatment almost 4 years after her first symptoms.
c) distance from the clinic: The distance from the patient's home to the nearest clinic was slightly less for controls than for cases (p = 0.011), but for both groups the median value is within the range of 1 to 2 hours.
d) other factors: A number of other factors were examined but no differences were noted between cases and controls. These factors included: 1) number of clinic visits in the previous year for other complaints; 45% of all patients had not attended a clinic in the previous year while 22% had attended more than twice, and 2) whether or not the patient knew other leprosy patients around the home area; 51 % of all patients knew of a leprosy patient living nearby. This figure varied in the different areas, but nowhere was there a significant difference between cases and controls (ALERT, 35%; West Shoa, 47%; Hararge, 58%).
e) knowledge and attitudes of patients: Various beliefs and attitudes were almost universal in this group of patients, taking cases and controls from all areas together:
Transmission. 84% believe that leprosy is inherited. Other possible causes mentioned are: bad spirits/curses, sent by God, sexual contact in the open air, infection/ contact (mentioned by only 6%).
Signs of leprosy. This question is confounded by the translation of the word leprosy as an Amharic word meaning to cut or mutilate (8). Thus, 75% of all patients gave loss of parts/deformities as the first sign of leprosy. This was even true of many patients who had given skin signs as the first symptoms that they had experienced them selves.
Can leprosy be cured? This question is also confounded by the confusion between bacteriological cure and reversal of the deformities of leprosy. In this sample, only 19% said they thought leprosy was curable.
Effect of health education. 8% of this largely illiterate group had seen a poster about leprosy, but those who had did not recall having learned anything from it. Radio had reached 10% in each area. In the Hararge area several patients reported hearing that leprosy is curable, but in West Shoa most patients could not recall any message given by the program.
DISCUSSION
Previous studies (1,5,7) have shown typical delays in Ethiopia, India and Nepal of around 1.5 to 2.5 years, and we have found a median overall delay of 26 months in disabled new cases but a median delay of only 12 months in those patients presenting without disability. Early case finding is known to be the most important factor in preventing disability from leprosy (6), and this is strongly confirmed by this study. Some similar studies have been done in other chronic diseases in Africa, for example, tuberculosis (2), but the symptoms in that case are more severe and make presentation more pressing so that direct comparison with leprosy is not possible.
We have shown that just over 50% of the delay occurs before the patient takes any action, and this requires specific and targeted health education for the general population. Disabled patients have a significantly longer delay before they take any health-seeking action: perhaps they have less knowledge or perhaps they have less initiative and are more fatalistic. The patients from the two rural areas studied were also very different in this respect, suggesting that local attitudes and culture are important factors. Former patients were a good source of advice for many patients, and this should be recognized and used in health promotion.
A further source of delay is the use of some form of traditional medicine, which overall accounted for just under one third of the delay. The ALERT patients had the largest delay at this point, perhaps because many are coming from areas of the country with less leprosy control work. Again, disabled patients were more likely to incur such a delay and to be delayed for a longer period, suggesting that they have greater faith in these forms of treatment and perhaps less knowledge of, or belief in, modern medicine. As can be seen most clearly in Figure 2, controls in West Shoa have the shortest delay of all patients at this point. However, it seems to be a common practice in Shoa to seek traditional remedies even after being diagnosed with leprosy, which may interfere with compliance in some cases. Thus, 4.5% of patients in Shoa incurred a delay of more than 6 months after diagnosis, as opposed to only 0.6% of patients in Hararge.
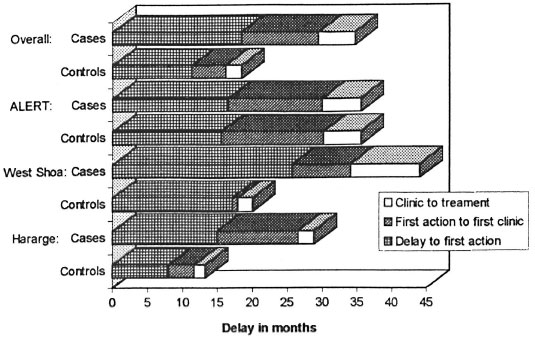
Fig . 2. Components of delay for cases and controls in the three areas studied.
Delay after attending a recognized clinic is a reason for concern. It accounts for over 10% of the total delay. Surprisingly, patients who already had a disability also incurred greater delay in being referred for leprosy treatment within the health services, perhaps due to stigma among staff.
Previous studies have indicated some of the reasons why leprosy patients in Ethiopia and elsewhere tend to be late in presenting, and the data presented here help to confirm those findings. An additional aspect of this study, which sheds more light on the reasons for late presentation, is the comparison of two areas with very different rates of DG 2 in new cases.
Stigma is a problem everywhere, but it is also very variable and appears to be decreasing in the Hararge area. There is decreasing social isolation of leprosy patients, both for activities such as farming and trading as well as social activities such as eating together and chewing "chat," a common leisure activity in the region. There is a local radio station and the leprosy hospital (Bisidimo) has had regular airtime to speak about leprosy. The impression is also given that this is a rather homogeneous and closeknit community, and information is discussed and disseminated by word of mouth more readily than in other parts of Ethiopia.
In West Shoa, on the other hand, stigma seems to remain very high and the patients are much more isolated. The people appear to be more independent in thinking, and new health-related information spreads slowly and is not easily accepted within the community. The Shoa area, in general, has numerous hot springs and these are widely utilized as healing or "holy" waters, often linked to nearby churches or monasteries. The Hararge area, in contrast, has very few of these sites and bathing in this hot water is much less common as a traditional form of treatment.
Stigma thus appears to vary between the two areas, but this is very difficult to measure. It also seems not to be closely related to the underlying beliefs about leprosy, which were similar in both areas. Thus, reducing stigma is far more complex than imparting knowledge and may relate to the way leprosy is managed by the health services and also the way in which patients are rehabilitated after cure (3).
Many beliefs (such as that leprosy is inherited, that it is not curable, that deformities are the main sign of leprosy) are equally strong in the two areas and indicate that, even in the face of these beliefs, patients can present early for diagnosis. Very few patients had been consciously influenced by health education messages; this suggests that health education campaigns must be more sophisticated and more carefully planned if they are to have any impact. The fact that many patients seek help from traditional practitioners suggests that they too should be involved in any program of public education (4).
It is clear that as leprosy services are integrated into the general health services the proper management of leprosy suspects must be addressed. Either clinic staff must be trained to make the diagnosis of leprosy, or they must have clear guidelines as to who must be referred and to whom. Because of the problems with referral, it would be ideal for diagnosis and the start of treatment to be done at the rural clinic, with examination by a specialist at a later stage.
Acknowledgment. We thank Dr. Peter Lever, Mr. Leon Bijlmakers and Ms Prisca Zwanikken of The Royal Tropical Institute (KIT), Amsterdam, The Netherlands, for their inspiration and help. We thank NSL and ALERT for funding and facilitating the field work, and our two research assistants, Ato Negussie H/Mariam and Ato Wondemu Kassye. ALERT is supported by ILEP members through NSL as coordinator.
REFERENCES
1. Becx-Bleumink, M. Priorities for the future and prospects for leprosy control. Int. J. Lepr. 61(1993)82-101.
2. Beyers, N, Gie, R. P., Schaaf, H. S., Van Zyl, S., Nel, E. D., Talent, J. M. and Donald, P. R. Delay in the diagnosis, notification and initiation of treatment and compliance in children with tuberculosis. Tuber. Lung Dis. 75(1994)260-265.
3. Frist, T. F. Employer acceptance of the Hansen's disease patient and other handicapped persons. Int. J. Lepr.48(1980)303-308.
4. Kaur, P.,Sharma, U. C, Pandey, S. S. and Gur-Mohan, S. Leprosy care through traditional healers. Lepr. Rev. 55(1984)57-61.
5. Rao, S., Garole, V., Walawalkar, S., Khot, S. and Karandikak, N. Gender differentials in the social impact of leprosy. Lepr. Rev. 67(1996)190-199.
6. Richardus, J. H., Finlay, K. M., Croft, R. P. and Smith, W. C. S. Nerve function impairment in leprosy at diagnosis and at completion of MDT a retrospective cohort study of 786 patients in Bangladesh. Lepr. Rev. 67 (1996) 297-305.
7. Schipper, A., Lubbers, W. J., Hogeweg, M. and De Soldenhoff, R. Disabilities of hands, feet and eyes in newly diagnosed leprosy patients in eastern Nepal. Lepr. Rev. 65(1994)239-247.
8. Tekle-Haimenot, R., Forsgren, L., Gebre-Mariam, A., Abebe, M., Holmgren, G., Heijbel, J. and Ekstedt. J. Attitudes of rural people in central Ethiopia towards leprosy and a brief comparison with observations on epilepsy. Lepr. Rev.63( 1992) 157-168.
1. M.D. Bisidimo Hospital. P.O. Box 22, Bisidimo, Harar, Ethiopia.
2. M.D. Box 165, Addis Ababa, Ethiopia.
3. M.D. Box 165, Addis Ababa, Ethiopia.
4. M.R.C.P. Box 165, Addis Ababa, Ethiopia.
5. ALERT, P.O. Box 165, Addis Ababa, Ethiopia.
Reprint requests to Dr. Paul Saunderson.
Received for publication on 3 September 1997.
Accepted for publication in revised form on 19 November 1997.
form on 19 November 1997.