- Volume 66 , Number 1
- Page: 49–51
A case of lymphocytic vasculitis with infiltration of dermal nerves resembling indeterminate leprosy
In an effort to increase the utility of the JOURNAL in continuing medical education, in this section we welcome contributions dealing with practical problems in leprosy work. Submissions to this section will undergo minimal editorial changes and may well contain controversial points. Letters to the Editor pointing out other viewpoints are welcome.
There have been reports of several skin diseases which can histopathologically resemble leprosy. Secondary syphilis,(1) lupus vulgaris, lichen planus and morphea(2) are some of them. In this communication a patient with lymphocytic vasculitis histopathologically resembling indeterminate leprosy is recorded.
CASE REPORT
A 71-year-old male patient reported to the outpatient department of the St. Thomas Hospital, Chettupattu, India, with a complaint of having live erythematous skin patches with minimal loss of sensations in the medial aspect of the left thigh, gradually increasing in size for a period of about 1 month. There was no itching. He felt numbness of both feet of unknown duration. There was no history of taking any drugs or any other relevant findings in the present or past history.
On physical examination there was a cluster of live skin lesions in the medial aspect of the left thigh. They were erythematous macules with vague borders, the largest of which measured 5 cm × 1.5 cm. No definite loss of sensations was detected either in the macular lesions or in the lower extremities. Routine blood and urine examinations were within normal limits. The nerve trunks were not enlarged. A clinical diagnosis of fixed drug eruption or allergic dermatitis was considered. Two biopsies, one from the largest and another from a smaller lesion, were done for further study.
Histopathologic sections from both lesions showed an almost identical picture. The epidermis showed flattening of rete ridges. There was dense perivascular infiltration by lymphocytes (Figs. 1 and 2) which obviously was the predominant feature of the lesion. In addition, diffuse infiltration of collagen bundles of the dermis by lymphocytes was present. Neutrophils and nuclear fragments were absent. The most interesting finding was the involvement of neurovascular bundles by the inflammation. A few nerves found in the mid-dermis showed perineuria] and possible intraneural infiltration by lymphocytes (Figs. 3 and 4). Nearly 20 additional sections were made and were stained with a modified Fite's stain for Mycobacterium leprae. (3) Acid-fast bacilli (AFB) were not found in any of them. A histopathological diagnosis of lymphocytic vasculitis was made.
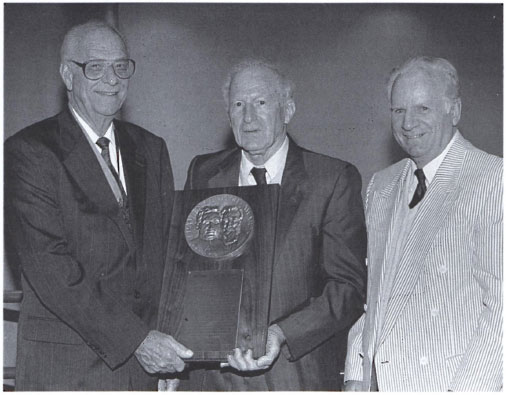
Fig . 1. Photomicrograph showing dense collections of lymphocytes selectively found around dermal blood vessels. Diffuse infiltration of dermis with lym-phocytes is also present (II&E ×50)
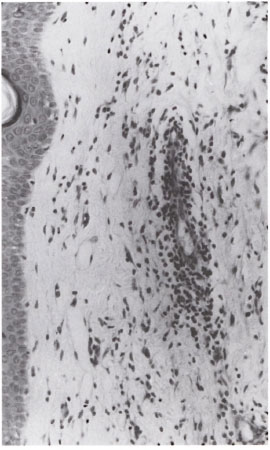
Fig . 2. Higher power view of Figure I to show dense focal perivascular infiltration by lymphocytes.Note absence of neutrophils and nuclear debris (H&E×150).
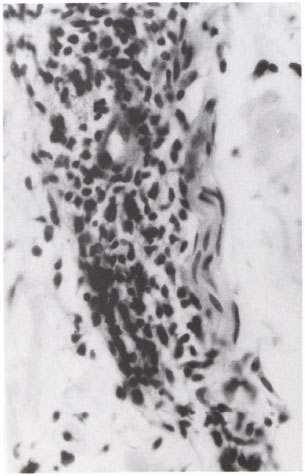
Fig . 3. Photomicrograph to show neurovascular bundle inflammation. The lymphocytes selectively involve and invade the blood vessel. The part of the nerve that adjoins the blood vessel is incidentally involved (H&E ×500).
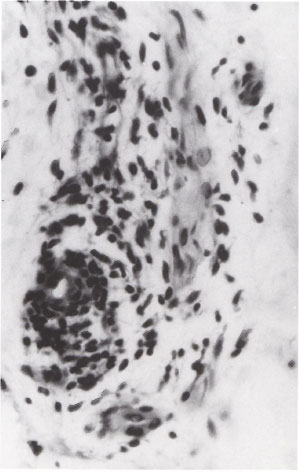
Fig . 4. Photomicrograph showing perineurial and possibly intraneural infiltration by lymphocytes H&E ×500).
The patient was not offered any specific treatment. The lesions disappeared completely and spontaneously in about 6 months.
DISCUSSION
Perineurial and endoneural infiltration of dermal nerves by lymphocytes is generally accepted as an important diagnostic feature of leprosy.(4) The perineurial and possible intraneural infiltration of dermal nerves in this patient was suggestive of indeterminate leprosy (Figs. 3 and 4) which might have resolved spontaneously. However, the selective involvement with invasion of the blood vessel walls by lymphocytes (Figs. 1 and 2), the absence of AFB despite careful examination under an oil immersion lens of over 20 sections stained for M. leprae, the multiplicity of lesions (five in number) with clustering, make it highly unlikely. It was clearly evident that the nerve involvement was only incidental (Fig. 3).
Lymphocytociastic vasculitis was ruled out because there were no neutrophils or nuclear debris in the inflammatory infiltrate. Unlike lymphocytociastic vasculitis, lymphocytic vasculitis is not a specific clinicopathologic entity but a reactive process.(5) Purpura pigmentosa chronica, fixed drug eruption, utricarial vasculitis, allergic vasculitis, and the vasculitis of Sjogren's syndrome are some of the conditions known to have lymphocytic vasculitis. Except in purpura pigmentosa chronica, the vasculitis in other conditions is transient. In this patient the history and clinical findings do not subscribe to a definite diagnosis of any of the above conditions. Therefore, a histopathologic diagnosis of lymphocytic vasculitis of undetermined etiology was offered.
All lesions with histopathological evidence of perineuria! and possible intraneural inflammation of dermal nerves are not due to leprosy. Further, it is possible that the lymphocytes apparently found in the nerve could be superimposed (Fig. 4) and only an electron-microscopic study could disprove or confirm the intraneural presence of these occasional inflammatory cells. In conditions which produce lymphocytic vasculitis, the accompanying nerve in the neurovascular bundle may be incidentally involved by the inflammatory infiltrate as found in this patient (Figs. 3 and 4). The presence of AFB inside the dermal nerves or in the subepithelial region or in arrector pili muscle cells or in the region of sweat glands should be looked for to make a definite diagnosis of indeterminate leprosy. In cases in which AFB are absent, granulomatous inflammation of the nerve is the other finding that may help us to arrive at a diagnosis of leprosy if it suits the clinical picture.
- Charles K. Job, M.D., F.R.C.Path.
J. Jayakumar, M.B.B.S., DTM&H.
M. Aschhoff, M.D.
St. Thomas Hospital and Leprosy Centre
Chettupattu 606 801
Tamil Nadu, India
Acknowledgment. We are grateful to Miss K. Jayanthi for secretarial assistance, to Mr. K. Rajanna for the technical work and to ALM International. Greenville, South Carolina. U.S.A., for financial support.
1. Job. C. K., Anandhan, G., Jayakumar, J. and Aschhoff. M. A case of secondary syphilis with a remarkable resemblance in histopathologic appearance to indeterminate leprosy. Int. J. Lepr. 62 (1994)433-435
2. Jacob, M., Chacko, C. J. G., Arunthathi. S. and Chandi, S. M. Significance and interpretation of nerve changes in skin biopsies when present in association with common dennatological conditions. (Abstract) Int. J. Lepr. 52(1984)755.
3. Job. C. K. and Chacko, C. J. G. A modified Fite's stain for demonstration of M. leprae in tissue sections. Indian J. Lepr. 58(1986)17-18.
4. Fine, P. E., Job. C. K., Lucas. S. B., Meyers, W. M., Ponnighaus, J. M. and Stern. A. C. J. Extent, origin and implications of observer variation in histopathol-ogical diagnosis of suspected leprosy. Int. J. Lepr. 61(1993)270-282
5. Massa. M. C. and Su. W. P. D. Lymphocytic vasculitis: is il a specific clinicopathologic entity? J. Cutan. Pathol. 11(1984)132-139.