- Volume 66 , Number 1
- Page: 29–33
Histopathological features of lepromatous iridocyclitis; a case report
ABSTRACT
A peripheral iridectomy specimen which included a portion of the ciliary body f rom an advanced lepromatous leprosy patient was studied histopathologically. The lepromatous granuloma in the iris was similar in content and appearance to that of skin lesions. It appeared that even in this advanced lepromatous patient the dilator muscles of the iris were preserved. This study agrees with the earlier observation that the dysfunction of the iris in lepromatous disease is most probably the result of autonomic nerve destruction. Further, it is possible that the lepromatous involvement of the iris may reflect the histopathological changes in the ciliary body.RÉSUMÉ
Un échantillon d'iridectomie périphérique qui comprenait une partie du corps ciliaire en provenance d'un malade présentant une lèpre lépromatcuse avancée a été étudié du point de vue hsitopathologique. Le granulome lépromateux dans l'iris était semblable en contenu et en apparence à celui des lésions cutanées. Il est apparu que, même chez ce patient lépromateux à un stade avancé, les muscles dilatateurs de l'iris étaient préservés. Cette étude concorde avec l'observation antérieure que le dysfonctionnement de l'iris dans la lèpre lépromatcuse est très probablement le résultat delà destruction du nerf autonomique. De plus, il est possible que l'implication lépromateuse de l'iris soit le reflêt des modifications histopathologiques dans le corps ciliaire.RESUMEN
Se estudió la histopatología de un espécimen de iridectomía periférica el cual incluyó una porción del cuerpo ciliar de un paciente con lepra lepromatosa avanzada. El granuloma lepromatoso en el iris fue similar en contenido y apariencia a los granulomas de la piel. No obstante lo avanzado de este caso lepromatoso, los músculos dilatadotes del iris estuvieron preservados. Este estudio está de acuerdo con la observación temprana de que la disfunción del iris en la enfermedad lepromatosa es probablemente el resultado de la destrucción del nervio autónomo. También es posible que la afección lepromatosa del iris pueda reflejar los cambios histopatológicos en el cuerpo ciliar.One of the important organs affected in leprosy is the eye, and lepromatous iridocyclitis frequently produces irreversible blindness (11). Clinically, "iris pearls" described as "microlepromas" have been identified in the pupil area and they are detected usually only by slit-lamp microscopy (3). Anterior and posterior synechiae are common complications of iritis which lead to severe visual handicap.
Tissues from the iris and the ciliary body of patients are not easily available for examination and, therefore, histopathological and electron-microscopic studies of these structures in leprosy are very few (1,4,7,9). Hence, the pathology and pathogenesis of eye lesions in leprosy are poorly understood. The lesions are not recognized early enough, and care of the eye is usually neglected until it is too late. In this communication a detailed account of the pathological appearance of iridocyclitis in an advanced lepromatous leprosy patient is recorded.
Case report. A 65-year-old male patient diagnosed clinically as lepromatous leprosy of approximately 12 years' duration reported a year ago with pain in the left eye. He had already had 10 years of dapsone monotherapy. On examination there were extensive, grossly infiltrated lepromatous lesions all over the body, face and extremities. There was lagophthalmos of the left eye, and a fleshy, inflamed pterygium was present. There was bilateral episcleral injection and fine corneal edema, although the intraocular pressure was not raised. There was a marked flare in the left anterior chamber, and dense cataracts were present in both eyes. Visual acuities were light perception only of the right and left eyes. The patient also had poor hearing, was febrile, and was distressed by his condition. After starting multidrug therapy (MDT) prescribed for multibacillary patients by the World Health Organization (15), topical and systemic antiinflammatory treatment, the pterygium (which was suspected to contain a high bacterial load) was excised and the findings were published (6). Three weeks later, when his left intraocular inflammation had improved, cataract surgery was done in that eye on the premise that although it was the eye with less visual potential it would give some immediate benefit. It was planned that the right eye, having better potential for visual recovery, could be operated on when his general condition was improved.
After his left cataract surgery, the patient defaulted (having had only 2 months of MDT). He returned a year later requesting right cataract surgery. At this point, his skin lesions appeared to have resolved, and he was in much better general condition. However, his bacterial index (BI) was 6+, albeit 80% of the bacilli had a granular morphology. The lens with cataract from the right eye was removed and a peripheral iridectomy at the 1 o'clock position was carried out. The cataract surgery was uncomplicated. A piece of the iris and the lens were sent for histopathological examination. The patient was again started on MDT and he and his son were counseled regarding the need to complete his treatment.
Histopathological examination. The iris tissue was fixed in 10% neutral formalin, processed for paraffin sections, 5-µm sections were cut and stained with hematoxylin and eosin (H&E) and a modified Fite's stain for acid-fast bacilli (AFB) (10).
The iris tissue showed marked thickening and edema. In some areas there were large collections of inflammatory cells infiltrating and replacing almost the entire connective tissue stroma. They consisted mostly of macrophages, some of which had a pink granular cytoplasm, but a large majority of them were foamy. Several of them had taken up melanin granules and appeared brownish-black. There were also neutrophils, lymphocytes and plasma cells (Fig. 1). An acid-fast stain showed many macrophages packed with AFB (Fig. 2) and in some melanin granules were present along with AFB. The infammatory granuloma extended up to the posterior surface of the iris which had an outer layer of heavily pigmented, hypertrophied epithelium (Fig. 1) and an inner layer consisting of pigmented myoepithelial cells which functioned as dilator muscle cells and were not easily seen. The integrity of the posterior epithelial surface was apparently preserved. In some other portions of the iris there was chronic inflammation with scattered macrophages, many of which contained AFB, pigment-filled cells, lymphocytes and plasma cells. Numerous vessels having a thick collagenous adventitia, characteristic of those found in the iris, were also present (Fig. 3).
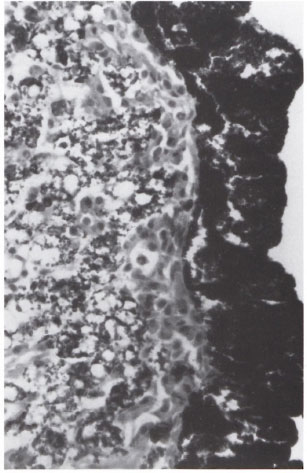
Fig. 1. Photomicrograph showing intact posteriorpigmented epithelium of the ids and iris stroma completely replaced by lepromatous granuloma composedof plasma cells, neutrophils, lymphocytes and foamymacrophages containing melanin granules. The granuloma extends up to the posterior surface of the iris (H&E x500).
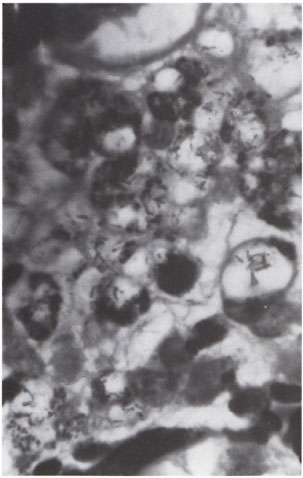
Fig . 2. Photomicrograph showing macrophages containing numerous acid-fast bacilli in addition to melanin granules (modified Fite ×1000).
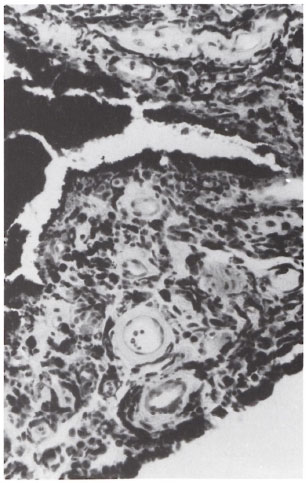
Fig . 3. Photomicrograph showing the stroma of theiris with its characteristic thick-walled blood vessels, infiltrated by chronic inflammatory cells (H&E ×500).
In another area of the section a strand of smooth muscles surrounded and infiltrated by lepromatous granuloma was seen (Fig. 4). The interstitial tissue of the muscle tissue showed scattered melanocytes containing melanin pigment, a feature of the circular portion of the ciliary muscle (2). The iris specimen was obtained during a peripheral iridectomy procedure and was obviously from the root of the iris, including the ciliary body and having a portion of the ciliary muscle. An acid-fast stain showed a few clumps of intracellular AFB inside the ciliary muscle cells (Fig. 5).
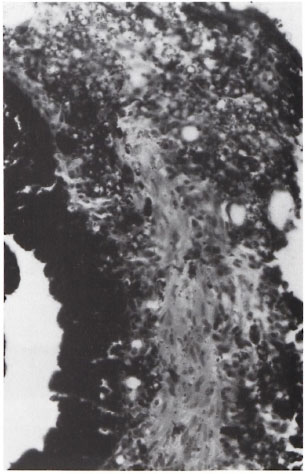
Fig 4. Photomicrograph showing pigmented posterior hning epithelium and a bundle of ciliary muscles surrounded and infiltrated by lepromatous granuloma(H&E ×250).
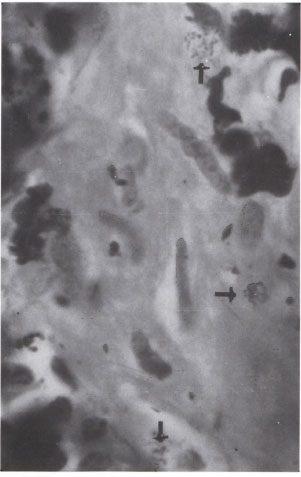
Fig. 5. Oil immersion field from Figure 4 showing three clumps of AFB in smooth-muscle cells. Note the presence of melanocytes (→) with pigment in between the muscle cells (modified Fite ×1000).
Comments. The lepromatous granuloma seen in areas of iris of this patient resembled much of that found in the skin of lepromatous patients, both in its content and in its appearance. Therefore, it is quite possible that infiltration of the iris by lepromatous granuloma may parallel that found in skin lesions and that the iris may be invaded by Mycobacterium leprae even in the early stages of the disease.
Infection of the iris by M. leprae was most likely through the blood stream during bacteremia. The organisms lodged in the tissue multiplied and the bacilli-filled macrophages increased in number, forming large granulomas admixed with neutrophils, lymphocytes, and plasma cells (Fig. 1). Although the granuloma hugged the lining at the posterior surface of the iris, the integrity of the epithelium containing the myoepithelial cells appeared to be preserved. Therefore, it is reasonable to state that the functional impairment of the dilator muscles of the iris in leprosy is primarily due to the impairment of the autonomic nervous system rather than a result of the destruction of the dilator muscles by the lepromatous granuloma. Earlier workers who investigated the pupillary function of the iris arrived at the same conclusion (12,14). In one report it is suggested that the autonomic nervous system may be impaired before any pathological changes are detected clinically (5). In another study it is stated that ocular sympathetic dysfunction was the cause of miotic pupils in leprosy (8).
It is apparent from this study that lepromatous granulomas infiltrating both the iris and the ciliary body were very similar in composition and intensity. Their anatomical relationship as one continues with the other facilitates such an almost identical histopathological appearance. It is likely that without proper antileprosy therapy the granulomatous inflammation may gradually destroy the ciliary muscles as well.
Acknowledgment. Financial support for this study from the American Leprosy Missions International, Greenville, South Carolina, U.S.A., is gratefully acknowledged. Thanks are also due to Miss K. Jayanthi for secretarial help and to Mr. K. Rajanna for the technical work.
REFERENCES
1. Allen, J. H. Pathology of ocular leprosy (ii) Miliary lepromas of the iris. Am. J. Ophthalmol. 61(1966)987-992.
2. Bloom, W. and Fawcett, D. W. The eye. In: A Textbook of Histology. 9th edn. Philadelphia: W. B. Saunders Co., 1962, p. 785.
3. Brand, M. E. and Ffytche, T. J. Eye complication in leprosy. In: Leprosy. 1st edn. Hastings, R. C, ed. Edinburgh: Churchill Livingstone, 1985, pp. 231-232.
4. Brandt, E, Zhou, H., Shi, Z., Rai, N., Thuladar, L. and Pradhan, H. Histopathological findings in the iris of dapsone treated leprosy patients. Br. J. Ophthalmol.74(1990)14-18.
5. Daniel, E. and Rao, P. S. S. Pupil cycle time in leprosy patients without clinically apparent ocular pathology. Int. J. Lepr.63(1995)529-534.
6. Daniel, E., Thompson, K., Ebenezer, G. J., Abraham. S. and Job, C. K. Pterygium in lepromatous leprosy. Int. J. Lepr. 64(1996)428-432.
7. Desikan, K. V. and Jon. C. K. Report of study of eye lesions in three aulopsied cases of leprosy. Lepr. India42(1970)1-3.
8. Ffytche, T. Iris in leprosy. Trans. Ophthalmol. Soc. U.K. 101(1981)325-330.
9. Hashizume, H. and Shionuma, E. Electronmicroseopie study of lepromatous changes in iris. Int. J. Lepr.33(1965)61-82.
10. Job. C. K. and Chacko, C. J. G. A modification of File's stain for demonstration of M. lepra in tissue sections. Indian J. I.epr.58(1986)17-18.
11. Joffrion. Van C. Ocular leprosy. In: Leprosy. 2nd edn. Hastings, R. C, ed. Edinburgh: Churchill Livingstone. 1994. p. 359.
12. Karacorly, M., Surel, Z., Cakiner, T, Hanya-Loglu, E., Saylan, T. and Mat C. Pupil cycle time and early autonomic involvement in ocular leprosy. Br. J. Ophthalmol.75(1991)45-48.
13. Lewallen, S., Hussein, N., Courtright, P., Ostler, H. and GELBER, R. Intraocular pressure and iris denervation in Hansen's Disease. Int. J. Lepr.58(1990)39-43.
14. Swift, T. R. and Bauschard, F. D. Pupillary reactions in lepromatous leprosy. Int. J. Lepr.40(1972)142-148.
15. Who Study Group . Chemotherapy of leprosy for control programmes. Geneva: World Health Organization. 1982. Tech. Rep. Ser. 675.
1. M.D., F.R.C.Path., F.A.M.S., F.I.C. Path., Consultant Pathologist, St. Thomas Hospital and Leprosy Centre, Chettupattu 606 801, TS. District, Tamil Nadu, India.
2. F.R.C.S., Consultant Ophthalmologist, Purulia Leprosy Home and Hospital, Purulia 723 101, West Bengal, India.
Received for publication of 23 December 1996.
Accepted for publication in revised form on 28 October 1997.