- Volume 66 , Number 1
- Page: 60–1
Chromoblastomycosis simulating lepromatous leprosy
To the Editor:
Chromoblastomycosis is a chronic infection of the skin caused by any of the several species of dematiaceous fungi. In most cases it begins on the extremities, particularly the feet. We report a woman who developed multiple plaques of chromoblastomycosis on the skin of the cheek and earlobe and mucosae of the nostrils and nasal septum. The buccal branch of right facial nerve also was involved, resulting in paralysis of the orbicularis oris. All of these features closely simulated leprosy clinically, and the patient was wrongly diagnosed and treated as having lepromatous leprosy by a general practitioner.
A 42-year-old widow developed multiple papules on the right earlobe, right cheek and mucosa of the nostrils 3 months following an injury from thorns from a cactus. The papules increased in size and spread peripherally to form an oval annular plaque of 4 × 3 cm on the cheek, a diffuse, infiltrated plaque on the right earlobe and an erythematous, verrucous plaque and ulceration of lower part of the cartilagenous portion of the nasal septum and right ala nasi (Figs. 1 and 2). There was no sensory deficit in the plaques and the oral cavity was normal. There was no nerve thickening but the buccal branch of the right facial nerve was affected, causing paralysis of the orbicularis oris of that side (Fig. 1). All other cranial nerves were normal. There were no other skin or mucosal lesions. All systems were clinically normal.
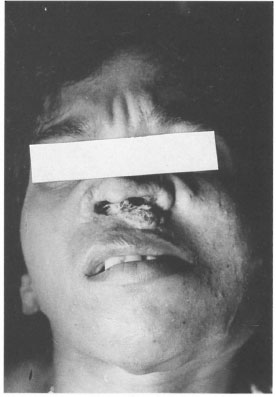
Fig. 1. Verrucous plaque of chromoblastomycosis on the face extending into the nasal cavity causing destruction of the nasal septum. Note facial asymmetry due to paralysis of the buccal branch of right facial nerve.
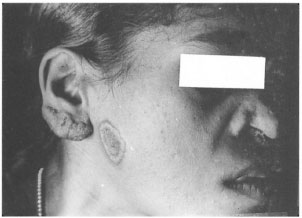
Fig . 2. Infiltration of the earlobe, an annular plaque on the cheek and destruction of ala nasi.
Routine laboratory tests on blood, such as total and differential leukocyte count, hemoglobin, ESR, blood sugar and blood urea, were within normal limits. The blood VDRL (Venereal Disease Research Laboratory) test was negative. Urinalysis was normal. The slit-skin smears from the earlobe and from the plaque, and scrapings from the nasal mucosa did not show acid-fast bacilli. The Mantoux test was negative. Epidermal scrapings from the earlobe and from the plaque on the cheek when examined in 10% KOH showed a few thick-walled, rounded, brownish-black bodies (sclerotic cells). A skin biopsy from the plaque on the cheek revealed a hyperkeratotic and acanthotic epidermis with small neutrophilic abscesses and tuberculoid formations in the dermis composed of epithelioid cells and multinucleated giant cells. Culture of the biopsy specimen from the nasal lesion in Sabouraud's agar yielded growth of Cladosporium carrionii. X-rays of the skull, face and chest did not show any abnormality except deformity of nasal septum corresponding to clinical destruction of the part. The CSF was normal and there were no fungal bodies in it.
The patient was treated with ketoconazole 200 mg twice daily orally for 2 months, but did not show any response. On discharge she was prescribed oral itraconazole but did not turn up for follow up.
Infiltration of the earlobe, presence of a raised plaque on the cheek, destruction of the cartilage of the nasal septum and nostril, and isolated paralysis of the buccal branch of the right facial nerve were the features that simulated lepromatous leprosy in our patient. These made the general practitioner diagnose and treat the case wrongly as leprosy. Chromoblastomyeosis commonly affects the skin only. Involvement of the nasal mucosa as occurred in our patient is extremely rare, although one such case was reported by Jakanitzu, el al. (1). Although the verrucous nature of the surface of the plaques, demonstration of "sclerotic cells" in the epidermal scrapings and characteristic histopathologic features easily differentiate chromoblastomycosis from leprosy lesions, some difficulty may occur if one is not aware of the possibility of chromoblastomycosis. A cutaneous plaque of chromoblastomycosis closely simulating tuberculoid leprosy clinically and histopathologically has been reported from India (2). Chromoblastomycosis developing in a residual patch of leprosy also has been reported (3). These reports and the present report underline the importance of considering chromoblastomycosis also in the differential diagnoses of all types of leprosy.
- K. Pavithran, M.D., D.V.D.,
M.N.A.M.S.
Professor
Department of Dermatology & Venereology
Medical College Hospital
Calicut 673 008, Kerala, India
REFERENCES
1. Jakanitzu, N., Grant, J. A., Threlkeld, R. and Wible, L. Primary chromoblastomycosis of the nasal septum. Am. J. Clin. Pathol. 58(1972)365-370.
2. Pavithran, K. Chromoblastomycosis masquerading as tuberculoid leprosy. Int. J. Lepr. 60(1992)657-658.
3. Pavithran, K. Chromoblastomycosis in a residual patch of leprosy. Indian J. Lepr. 60(1988)444-447.