- Volume 66 , Number 2
- Page: 170–81
The occurrence of reactions and impairments in leprosy: experience in the Leprosy Control Program of three Provinces in Northeastern Thailand, 1978-1995. III. Neural and other impairments
ABSTRACT
Aim: This the third paper in a series of three papers on the occurrence of reactions and impairments in leprosy in Thailand, and focuses on the prevalence and incidence of neural and other impairments in leprosy. Study design: A population-based, prospective cohort study. Study subjects: All 640 newly diagnosed and registered leprosy patients in three provinces of northeastern Thailand between October 1987 and September 1990 were included [420 paucibacillary (PB) and 220 multibacillary (MB)]. This group of patients was followed up until the end of 1995. Methods: Clinical data; data on the sensibility and motor function of eyes, hands and feet, and data on wounds and bone loss were obtained where appropriate. The occurrence of neural and other impairments at first examination, during treatment and during surveillance was ascertained. Results: The relationship between impairment prevalence (grades 2 of the combined PB and MB groups and grades 1 and 2 together of the combined PB and MB groups) and duration of disease (before diagnosis) was found to be statistically significant. Increased delay in detection led to increased problems of impairments. Too many patients still develop new/additional impairments while on treatment and thereafter. The incidence rate of nerve function impairment (NFI) among patients without impairments at first examination while on treatment was 1.7 [95% confidence interval (CI) 0.45-4.4] per 100 person-years at risk (PYAR) for the PB group and 12 (CI 8.4-17) per 100 PYAR for the MB group. Additionally, 2% of the PB and 11% of the MB patients who already had impairments at first examination developed new NFI while on treatment. The outcome, comparing the first examination with the last examination during/after surveillance [changes in the voluntary muscle test (VMT), the sensory test (ST), wound count and bone loss], indicated that of the PB patients 3.7% improved, 3.7% got worse and 3.9% kept the same impairment; of the MB patients 19% improved, 18% got worse and 2.9% kept the same impairment. During treatment most of the new/additional impairments were due to new/increase in NFI; during surveillance slightly more than 50% were due to new/increase in NFI. Eighty-three percent of the MB patients without impairments at first examination who developed NFI during treatment improved (completely or partially) after receiving prednisolone. Only 62% of the MB patients with a grade 1 impairment at first examination and who dcvelopcd a severe reaction or recent silent neuropathy improved after receiving prednisolone. There is a necd for an indicator to measure new/additional impairments while on treatnient and thereafter. It is proposed to measure changes in impairment by measuring changes in VMT, ST, wound count and bone loss.RÉSUMÉ
But: Cet article est le troisième d'une série de trois articles traitant de l'apparition d'états réactionnels et de déficits hanséniens en Thaïlande, et expose en particulier la prévalence et l'incidence des complications invalidantes de lèpre, nerveuses et autres. Population d'étude: La totalité des 640 nouveaux cas de lèpre [420 paucibacillaires (PB) et 220 multibacillaires (MB)] diagnostiqués dans les 3 provinces contigues de la Thaïlande du nord-est, enregistrés de octobre 1987 à septembre 1990, fut étudiée. Ce groupe de patients a été suivie jusqu'à la lin de 1995. Méthode: Les données cliniques et les données, lorsque jugées appropriées, concernant les fonctions sensitives et motrices des yeux, des mains et des pieds lurent obtenues. L'apparition de complications invalidantes de lèpre, nerveuses et autres, fut déterminée au cours de premier examen, au cours du traitement et durant le suivi post-traitement. Résultats: La relation entre la prévalence des déficits hanséniens (le grade 2 des groupes combinés PB et MB et les grades I et 2 ensemble des groupes combinés PB et MB) et la durée de la maladie (avant traitement) est statistiquement significative. Un délai de détection important mène à une augmentation des problèmes d'infirmités. Trop de patients développent encore des déficits ou ces derniers empirent pendant ou après le traitement. Le taux d'incidence des déficits fonctionnels nerveux (DFN) durant le traitement, parmi les patients sans déficits détectés durant l'examen initial, est de 1,7% [intervalle du confiance de 957r> (IC) 0,45-4,4] pour 100 personnes-années à risque (PAAR) chez, les patients PB et de 12 (IC: 8,4-17) pour 100 PAAR chez, les patients MB. De plus, 2% des cas PB et 11% des cas MB qui avaient déjà des déficits au moment du premier examen clinique ont développé de nouvelles DFN durant le traitement. A la lin de cette étude, si le premier examen clinique et le dernier examen durant/après la période de suivi sont comparés [modifications du test musculaire volontaire (TMV), du test sensoriel (TS), du nombre de blessures et des pertes osseuses], alors on constate que parmi les palieuls PB. 3.7% se sont améliorés, 3,7% ont empires et 3,9% sont restés stables; parmi les patients MB, 19% se sont améliorés, 18% ont empires et 2,9% sont restés stables. Durant le traitement, la grande majorité ties nouveaux déficits et détériorations était due à des nouveaux DFN ou une augmentation des DFN; durant le suivi post-traitement, un peu plus de 50% était dû à des nouveaux DFN ou une augmentation des DFN. Quatre vingt trois pour cent des patients MB sans déficits au premier examen, qui développèrent des DFN durant le traitement vécurent uns amélioration partielle ou complète après l'administration de prednisolone. Seulement 62% des patients MB présentant un déficit de grade 1 durant le premier examen et qui ont développé une réaction sévère ou une neuropathic silencieuse récente se sont améliorés après l'administration de prednisolone. Il y a un besoin pressant de trouver un indicateur fiable pour mesurer les nouveaux déficits et détériorations cliniques durant et après le traitement. Il est proposé d'évaluer les variations de déficits en mesurant les modifications du TMV, du TS, du nombre de blessures et des pertes osseuses.RESUMEN
Objetivo: Este es el tercero de tres artículos sobre la oceurrencia de reacciones y el empeoramiento consecuente de la lepra en Tailandia. Este parte del estudio se refiere a la prevalência e incidencia de neuropatías y de otras alteraciones de la lepra. Diseño del estudio: Un estudio poblacional prospectivo de cohortes. Población de estudio: Los 640 casos nuevos de pacientes con lepra [420 paucibacilares (PB) y 220 multibaeilares (MB)] diagnosticados en tres provincias de Tailandia entre Octubre de 1987 y Septiembre de 1990. El seguimiento de los pacientes se continuó hasta finales de 1995. Métodos: Además de los datos clínicos se obtuvieron datos sobre las funciones sensorial y motora de los ojos, pies y manos, sobre la presencia de heridas y sobre la oceurencia de pérdida de hueso. Se estableció la ocerrencia de alteraciones neurológicas (y otras) en el momento del primer examen, durante el tratamiento y durante el tiempo de seguimiento. Resultados: Se encontró que la relación entre la prevalência de las alteraciones (grados 2 de los grupos PB y MB combinados y grados 1 y 2 de los grupos PB y MB combinados) y la duración de la enfermedad fue estadísticamente significativa. Mientras más prologado fue el retardo en la detección de casos, más alta fue la tasa de agravamiento de la enfermedad. Muchos pacientes desarrollaron alteraciones nuevas o adicionales durante el tratamiento y después del mismo. La tasa de incidencia de agravamiento en la función nerviosa (NFI, nerve funciton impairment) entre los pacientes sin alteración en el primer examen fue de 1.7 (95%, intervalo de confianza, IC, de 0.45-4.4) por 100 persona-años en riesgo (PYAR) para el grupo PB y de 12 (IC 8.4-17) por 100 PYAR para el grupo MB. Adicionalmente, el 2% de los PB y el 11 % de los MB que ya tenían disfunción en el primer examen, desarrollaron nuevas NFI durante el tratamiento. El resultado, comparando el primer examen [que incluyó los cambios en la prueba de los músculos voluntarios (VMT), la prueba sensorial (ST), la cuenta de lesiones y la pérdida de hueso] con el último examen efectuado durante o al final del tratamiento, indicó que el 3.7% de los pacientes PB mejoraron, el 3.7% empeoraron y el 3.9% no modificaron su grado de afección. De los pacientes MB, el 19% mejoró, el 18% empeoró y el 2.9% mantuvo su grado de afección. Durante el tratamiento, la mayoría de las alteraciones nuevas o adicionales se debieron a alteraciones neurológicas nuevas o adicionales; durante el seguimiento, un poco más del 50% de las alteraciones se debieron a NFI nuevas o adicionales. Ochenta y tres por ciento de los pacientes MB sin alteraciones en el primer examen que desarrollaron NFI durante el tratamiento, mejoraron completa o parcialmente después de recibir prednisolona. Sólo el 62% de los pacientes MB con afección del grado 1 en el primer examen que desarrollaron una reacción severa o una nueva neuropatía subclínica, mejoraron después de su tratamiento con prednisolona. Es necesario desarrollar algún indicador que permita medir las alteraciones nuevas o adicionales cuando los pacientes están en tratamiento y después del mismo. La medición de las cambios en las pruebas VMT y ST, la cuenta de lesiones y la pérdida de hueso, podrían servir para medir tales alteraciones.The ultimate test of a leprosy control program's effectiveness is the occurrence of impairments (any loss or abnormality of physiological, psychological or anatomical structure or function) among newly diagnosed leprosy patients and the occurrence of new or additional (N/A) impairments among patients on treatment and after treatment (37). Impairment is a very relevant measurement of progress in leprosy control (26). In evaluating any new treatment regimen, the incidence of impairments during and after treatment is as important a measure of the value of a new regimen as the relapse rate (34). Nerve function impairment (NFI), if not diagnosed and treated in time, will usually become permanent and may result in disabilities and handicaps (3).
This is the third paper in a series of three papers on the occurrence of reactions and impairments in leprosy in three provinces of northeastern Thailand, and focuses on the prevalence and incidence of neural and other impairments. The other two papers report on: I. General Overview of the Study (epidemiological observations, delay in detection, MDT completion, relapses) and II. Reactions.
PATIENTS AND METHODS
A total of 640 newly diagnosed leprosy patients [420 paucibacillary (PB) and 220 multibacillary (MB)] from three provinces (Mahasarakham, Roi-et and Kalasin) in northeastern Thailand were enrolled in this study. The study lasted from October 1987 until the end of 1995. (For an overview of the study see Part I.)
Routinely, impairment records (36) were made on registration, then every 3 months. In case of complications recordings were made monthly. Patients under surveillance were examined annually. To ensure the quality of the impairment examination and recording in this study, a special prevention of disability (POD) team from the Leprosy Control Center, Khon Kaen, Thailand, visited patients' homes for re-examination at least once during treatment and once during surveillance.
Where possible, the term "impairment" was used instead of the more common, but incorrectly, used term "disability" (any restriction or lack, resulting from impairment, of ability to perform an activity in the manner and within the range considered normal for a human being) (8, 37).
History taking; inspection of eyes, hands and feet; palpation of nerves; voluntary muscle testing (VMT) and sensory testing (ST) provided the relevant information needed for the early diagnosis of nerve function impairment (NFI). As a sensory test the ballpoint pen test (36) was used (hand: 10 sites; foot: 12 sites). The pen was aimed at making a dent as small as possible without applying any extra force except the weight of the (Bic-type) ballpoint pen. Assessment of the motor function was done with a three-grade scale (strong, weak, paralyzed).
A change in NFI (improvement or worsening) was considered meaningful if there was a change in ST of two or more points or a change in VMT of one point on the three-grade scale. Additionally, changes in wound count or increase in bone loss were taken into account. Improvement in the few patients who had reconstructive surgery was not graded.
For monitoring changes in nerve function or in impairments, baseline POD records were used (35, 36). As an outcome indicator for patient management (as opposed to treatment compliance), the proportion of patients with new or additional (N/A) impairments while on treatment and surveillance was used. A patient with a change (to the worse) in any of the parameters (ST, VMT, wound count, bone loss) was counted once (numerator). The denominator for this indicator was the total number of patients on the treatment and the surveillance cohort (minus the patients who were lost to follow up, transferred out or who had died).
In this study, the World Health Organization (WHO) disability three-grade (grade 0, grade 1, grade 2) system was used (38). WHO grade 1 generally refers to loss of protective sensation. In this study any loss of sensation (ballpoint pen not felt) or weakness was classified as WHO disability grade 1. Additionally, lagophthalmos was classified as WHO disability grade 2.
Statistical methods. When determining the difference between two unpaired observations in the case of a large sample the normal test was used (12). The chi-squared test was used for analyzing the difference between proportions and for trends. Relative risk was calculated by comparing the incidence rate of new impairments between the groups with and without impairments at the start of treatment. Incidence rates were calculated as the number of patients developing new NFI during the follow-up period divided by the cumulative person-years at risk (PYAR). Patients lost to follow up (had died, transferred out) only contributed to the denominator as long as they were followed up. The same was the case for patients developing new NFI. A p value of less than 0.05 was used as a level of statistical significance. Confidence intervals (CI) (95%) are given for the prevalence and incidence rates. Epi Info software, version 6 was used for part of the analysis.
RESULTS
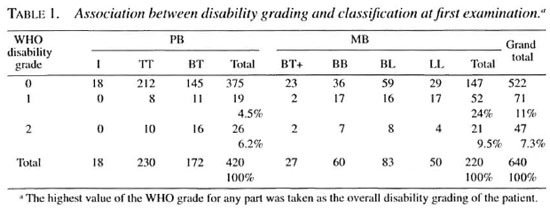
At first registration there was a (statistically significant) increasing proportion of patients with impairments (WHO disability grades 1 and 2 combined) for those with tuberculoid (TT) classification toward those with lepromatous (LL) (TT 7.8%, BT 15.7%, BT MB 14.8%, BB 40%, BL 28.9%, LL 42%; chi-squared for linear trend: 51.6; p value = 0.000001) (Table 1). Of all the nerves involved at first registration 36% were ulnar, 36% posterior tibial, 15% median, 7.4% common peroneal (lateral popliteal), 5% facial and 1.2% high radial (data not shown).
Seventeen (24%) out of 71 patients with WHO disability grade 1 at first examination were found to have only muscle weakness not accompanied by loss of sensation. Eight of these 17 patients had weakness of more than one muscle group (as supplied by different nerve trunks).
Impairment, classification, sex and age at diagnosis, mode of case detection. If the WHO grades I and 2 are combined then 11% (95% CI 8-14) of the PB and 33% (CI 27-39) of the MB patients had impairments at diagnosis (Table 1). The difference in the proportions of grade 1 impairments between PB (4.5%) and MB patients (24%) is statistically significant. The difference in proportions of grade 2 impairments between PB and MB patients was not statistically significant.
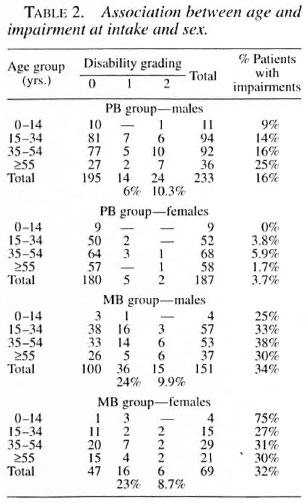
The association between impairment (WHO disability grading) at first examination and sex is shown in Table 2. In the PB male group, a much higher proportion of impairments was seen compared to the PB female group (highly significant). In the MB group no differences were seen in the proportion of impairments between men and women. When looking at impairment and age only in the PB male group, an increase in impairments with age was seen (not statistically significant). In the other groups (female PB, male and female MB), the proportions of impairments between the different age groups were similar.
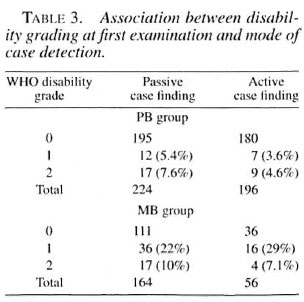
Although more patients, both PB and MB, in the passive case-finding group had impairments, this was not statistically significant (Table 3).
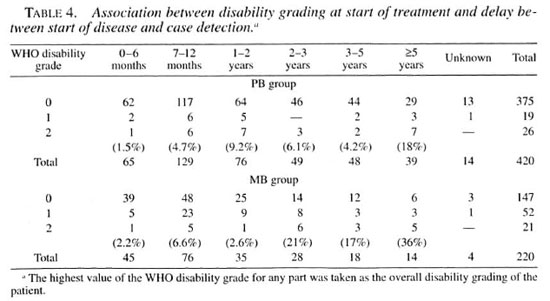
Impairments at diagnosis and duration of disease before detection. This relationship is shown in Table 4. The numbers of patients with impairments (grades 1 and 2) in the delay groups are rather small (many less than five). Nevertheless, the chi-squared test for linear trend (increase in impairments with an increase in delay in detection) when adding together the disability grades 2 of the PB and MB groups is 19.2, p value = 0.00001; when adding together disability grades 1 and 2 of the PB and MB groups it is 8.6, p value <0.005. The chi-squared test for linear trend of the disability grade 2 MB group is 16.3, p value = 0.00006.
Changes in impairments between first examination and RFT, between RFT and on average 3 years of surveillance and between first examination and end of surveillance. During treatment (comparing first examination with RFT) of the PB patients 1.2% (CI 0.2-2.2) improved (changed from WHO disability grade 1 to 0 or from 2 to 1); 1.7% (CI 0.5-2.9) worsened (chansied from WHO disability crade 0 to 1 or 2 or from 1 to 2); and 8.6% (CI 5.9-11.3) with impairments at first examination did not change. Regarding the MB patients during treatment, 11.27c (CI 7.0-15.4) improved; 11.7% (CI 7.4-16.0) worsened and 19.6% (CI 14.3-24.9) stayed the same (Tables 5 and 6).
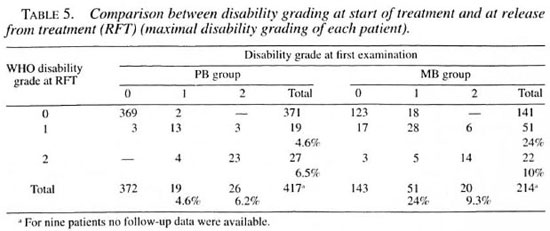
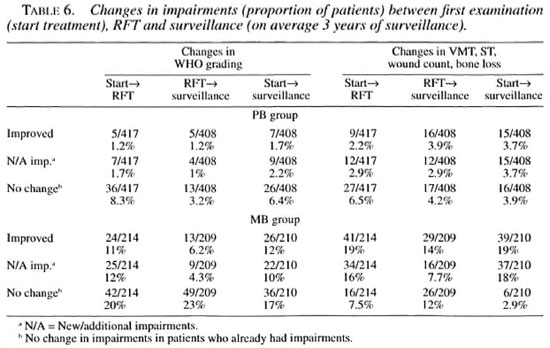
Changes in ST, VMT, wound count and bone loss between the first examination and RFT were taken into consideration. During treatment, 2.2% (CI 0.8-3.6) of the PB patients improved; 2.9% (CI 1.3-4.5) worsened and 6.5% (CI 4.1-8.9) of the patients with impairments did not change. Of the MB patients, 19.2% (CI 13.9-24.5) improved; 15.9% (CI 11-20.8) got worse; and 7.5% (4-11) did not change (Table 6).
More patients showed changes in VMT, ST, wound count and bone loss than in WHO disability grading. Changes for the worse in ST, VMT, wound count and bone loss when comparing first examination and after surveillance were seen in 3.9% of the PB and 18% of the MB patients. Changes for the worse expressed in changes in WHO grading when comparing first examination and after surveillance were seen in 2.2% of the PB and 10% of the MB patients (Table 6). These differences are not statistically significant. However, the difference in the no change category (no change in impairment in patients who had impairment already) between the two measurements is statistically significant for the MB group.
During treatment most changes for the worse (82%) came from new/additional NFI (changes in VMT and ST). Only a minority were due to new/additional tissue damage (wound count and bone loss). During surveillance, about 53% of the changes for the worse came from new/additional NFI and 47% from new/additional tissue damage.
One PB patient and 31 MB patients (14%) developed new NFI while on MDT treatment (and subsequently received prednisolone) which improved (completely or partially) before RFT. Some of these patients already had other impairments at first examination which, in most cases, did not improve. One PB and two MB patients developed new NFI on surveillance which improved (after receiving prednisolone) later (data not shown).
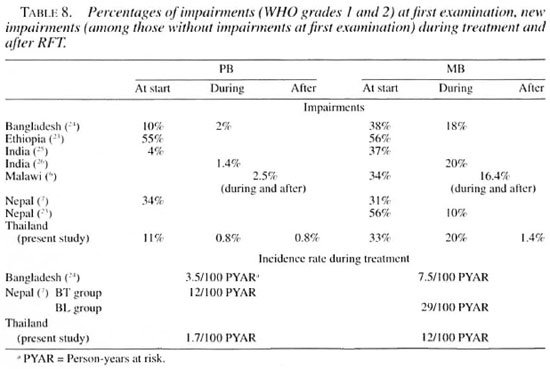
Incidence rate of new impairments during treatment and during surveillance. During treatment three PB (0.8%, CI 0-1.7) and 29 MB patients (20.3%, CI 13.7-26.9) without impairments at first examination developed new NFI while on treatment (some impairments improved before RFT) (data not shown). The incidence rate of new impairments during treatment among patients without impairments at diagnosis for the PB group was 1.7 (CI 0.454.4) per 100 PYAR (6 months' follow up); for the MB group 12 (CI 8.4-17) per 100 PYAR (24 months of follow up). One PB patient (2.2%) and 10 MB patients (14%) who already had impairments at first examination developed new NFI (of nerves previously not affected) while on treatment (data not shown).
Three PB (0.8%, CI 0-1.7) and two MB patients (1.4%, CI 0-3.3) without impairments at RFT developed new NFI while on surveillance. The incidence rate of new impairments among patients without impairments at RFT during the first 3 years of surveillance were 0.3 per 100 PYAR for the PB and 0.5 per 100 PYAR for the MB group. If the two MB patients who developed new impairments more than 2 years after the start of MDT and who received additional MDT had been included, the incidence rate would have become 1 per 100 PYAR. Two (4.4%) of the PB and six (8.5%) of the MB patients who already had impairments at RFT developed new NFI (of nerves previously not affected) while on surveillance (data not shown).
Risk ratio of developing new NFI between patients with and without impairments at first examination. Six (1.6%) out of 372 PB patients without impairments and 3 (6.7%) out of 45 PB patients with impairments at first examination developed new NFI during treatment and surveillance (data not shown). The risk ratio among PB patients developing new NFI between patients with and without impairments at first examination was 4 (Fisher exact test, p = 0.062, statistically not significant).
Thirty-three (23%) out of 143 MB patients without impairments and 16 (23%) out of 71 MB patients with impairments at first examination developed new NFI while on treatment and surveillance. The risk ratio among MB patients of developing new NFI between patients with and without impairments at first examination was 1 (data not shown).
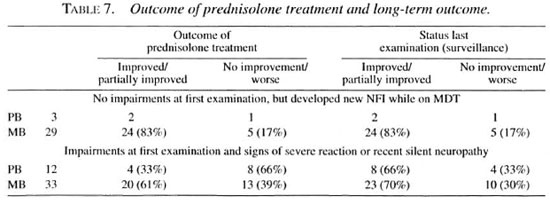
Outcome of prednisolone treatment and long-term outcome. The outcome of prednisolone treatment was better in patients who developed new NFI while on treatment but had no impairments at first examination (26 patients out of 32 improved) compared to patients who already had impairments at first registration (24 out of 35 improved) (Table 7). This was statistically significant with an odds ratio of 3.79 (1.18< OR < 12.69); p value <0.05). However, at last examination no statistically significant difference between the two groups was found. Some patients (7 of 21 out of the group of patients who already had impairments at first examination) continued to improve even after the prednisolone course had finished. The improvement of PB patients was less than that of the MB patients.
In several patients an improvement in ST and VMT was seen without having received prednisolone treatment. Six PB patients (13%) and 10 MB patients (14%) with impairments at first examination (but without signs of a severe reaction or recent silent neuropathy) had partially improved at RFT.
DISCUSSION
No one system of disability grading will meet all requirements (38). In this study, weakness and any loss of sensation (not only loss of protective sensation) was graded as WHO disability grade 1. In leprosy, changes in sensation are often an earlier sign of" nerve involvement than changes in muscle strength (7). In this study, 24% of the patients with early NFI of the ulnar nerve demonstrated motor function impairments without any loss of sensation. The same finding has been reported from Indonesia (5). In Bangladesh the most commonly involved nerves were the ulnar (motor function) and the posterior tibial (sensibility) (24). The ballpoint pen test, which was the only sensory test (ST) used in the first years of the study, underestimates the extent of the sensory impairment. According to a study from Ethiopia, if a 1-gram filament were routinely used instead of a 10-gram filament, almost twice as many instances of NFI would be diagnosed (9).
It is clear that 200 trig (threshold for "normal" touch sensibility measured with monofilaments) may identify early NFI, but protective sensation may be present at a level of a 2.0-gram Semmes-Weinstein monofilament (1, 11, 13). The equivalent filament in the ballpoint pen examination, if only the weight of the (Bic) ballpoint pen and no extra pressure is exerted on the skin, may be estimated to be between 5-10 grams. The purpose of ST with a ballpoint pen is unfortunately twofold. First, to identify any sensory NFI (i.e., evidence of neuritis) and, second, to ascertain if there is any loss of protective sensation (i.e., danger for further impairment). The ballpoint pen test is widely used and is the only sensory test in use in many field projects.
Prevalence of impairment at diagnosis and its risk factors. Risk factors for impairments found at diagnosis in leprosy have been studied widely (19, 22, 38). Risk factors often mentioned include classification, sex, age, mode of case finding, and duration of disease. In this study a much higher proportion of patients with impairments wasfound in the MB group compared to the PB group; statistically significant in the case of WHO disability grade 1. In the PB groupmale patients had a higher prevalence ofimpairments than did females. The prevalence of impairments in the MB group wassimilar between the sexes. This last finding has not been noted in other studies. It isgenerally said that the prevalence of impair-ments is higher in male patients (14).
Only in the PB male patients was an in-creasing prevalence of impairments (WHO grades 1 and 2 combined) seen with increasing age, but this was not statistically significant. Noordeen and Srinivasanshowed that the association between ageand impairment at diagnosis in their studywas, in fact, confounded by the duration ofdisease (19). A repeat of a similar computation cannot he made in this study becauseof the small numbers of male PB patients involved.
In this study a slightly higher proportionof patients from the passive case-finding group had impairments compared to the active case-finding group, but this was not statistically significant (if stratified in PB and MB).
Prevalence of impairment and duration of disease before diagnosis. The proportion of newly registered patients withWHO disability grade 2 is only meant to bea rough outcome indicator for the level of case-detection activities (early versus latecase detection). The relationship betweenimpairment prevalence and duration of disease was found to be statistically significant when the PB and MB groups were combined in case of the grades 2 and in case of the grades I and grades 2 together. This positive association between impairment prevalence and reported duration has been reported earlier (19, 22, 29).
Comparison among impairments atfirst examination, at RFT and after RFT (on average 3 years of surveillance). Table 8 shows the outcome of case management in the present study and from otherstudies. In Malawi, 2.5% of the PB patients developed new impairments and 3.3% worsened during and after WHO/MDT. Of the MB patients, 16.4% developed new impairments and 9.8% got worse during andafter WHO/MDT (6, 21). They (the Karonga Trial) concluded that the overall percentage of patients who developed new impairments during and after WHO/MDT remains disturbingly high (21).
In this study, during treatment most changes for the worse came from new/increased NFI. Also during the first 3 years after RFT slightly more than 50% of the changes came from new/increased NFI. It is likely that the longer the period after RFT, most if not all changes will be from new/increased tissue damage (wounds, bone loss).
Risk of new impairment during treatment and surveillance. In Malawi, in a group of newly diagnosed MB patients (who had no impairments at diagnosis) 13.9% developed new impairments during a 3-year follow-up period. Of the patients who already had impairments at diagnosis, 50% developed new impairments. The risk ratio among these patients was 3.6 (21). In a study from Nepal, a near twofold increase in risk was found (developing new impairments between those with and without impairments at diagnosis), which was almost equal in patients who "only" had sensory impairment at diagnosis to those who already had visible deformity. The presence or absence of impairment at diagnosis proved to be the major risk factor for developing new impairment (23). However, in our study impairments at first examination were not a risk factor for the subsequent development of new impairments.
In Malawi higher incidence rates of impairments among PB patients were found after rather than during treatment (22). In this study from northeastern Thailand similar incidence rates during and after treatment were found among PB patients. The incidence rate of new impairment among MB patients was much higher during treatment than during surveillance.
Nerve function impairment: steroid treatment outcome. In a study from Ethiopia, improvement in ulnar nerve function was obtained in 60% and in the median nerve in 67% of cases (30). In Nepal, after 3 months on corticosteroids 84% of the patients with sensory and 76% of those with motor impairment of the median nerve had improved, while only 60% and 47%, respectively, of patients with ulnar nerve lesions showed improvement. From the same Nepalese study a large proportion of patients (32%-47%) showed no functional improvement at all despite rigorous therapy for "recent" impairment (33). In the leprosy control program of Shoa Province, Ethiopia, 83% of the patients of the field program with NFI who were treated with a course of corticosteroids improved (partially or totally) (3).
The outcome of prednisolone treatment in this study showed an improvement in a higher proportion of those MB patients without impairments at first examination and less improvement in those MB patients with impairments at first examination (difference not statistically significant). The less impressive outcome in the MB patients with impairments at first examination could be partly due to the predominance of ulnar nerve involvement in these Thai patients, partly due the fact that in some patients the NFI was more established than stated, and partly to the fact that the present (comparatively short duration) steroid treatment, even if instituted quickly, is considered by many to be unsatisfactory (21). In the case of recent NFI, significantly better neurological recovery may be achieved by a high (starting) dosage, and long-term steroid therapy compared to short-term therapy (18, 28) .
Of the few MB patients with WHO grade 2 impairments improvement was shown by only 50% of the cases. The likeli-hood of good recovery for both sensibility and motor function is directly related to the severity of the nerve damage at the beginning of treatment (33).
Some PB and MB patients continued to improve after RFT after the course of prednisolone was finished. Another interesting observation is that some of the PB and MB patients with impairments at first examination (but without signs of a severe reaction or recent silent neuropathy) partially improved without having received any prednisolone (17).
Indicator for case management. Until now, no acceptable (simple and valid) tool has been developed to measure the outcome of case management, an indicator to measure N/A impairments while on treatment and surveillance. Such a tool should be sensitive enough to measure changes in impairment (26). The objective of impairment and disability prevention is that patients should not develop new impairments or disabilities apart from those which were irreversible at diagnosis (36). The WHO disability grading does not provide detailed information on patient impairments nor is it meant to be used to manage and follow up POD activities. The indicator N/A impairments which takes into account changes in ST, VMT, wound count and bone loss seems to be a more sensitive and valid indicator than the recording of changes by the WHO disability grading.
In Ethiopia, a score per patient of the sum of the disability grades for the four extremities (hands and feet), known as the "HF-impairment score," was shown to be more informative than just recording and comparing the overall patient disability grades (10). Even this "HF-impairment" score [in some projects the eye is included as well and called the "EHF-impairment score" (23)] will miss changes within one extremity as long as the disability grading does not change. For example: an increase in loss of sensation in one hand or the appearance of ulcers in a drop foot will not be counted in the EHF score. The advantage of the EHF score is that it reflects the seriousness of the total impairments per patient.
No operational targets or acceptable level of performance for the proportion of patients with N/A impairments have yet been set. Over the past 10 years most leprosy control programs supported by the Netherlands Leprosy Relief Association (NSL) have a program objective regarding prevention of further impairments during the course of treatment. The target varies, but many programs have adopted a figure of <5% of patients developing N/A impairments, usually measured by WHO disability grades. It is obvious that such targets should also include the (passive) surveillance period. In view of the above, it seems that primary and secondary prevention of impairment, i.e., prevention of NFI, should be given the utmost priority by the leprosy control program.
REFERENCES
1. BELL-KROTOSKI, J. A. Light touch-deep pressure testing using Semmes-Weinstein monofilaments. In: Rehabilitation of the Hand: Surgery and Therapy. 3rd edn. Hunter, J. A., Schneider, L. II. Maekin. F. J. and Callahan, A. D., eds. St. Louis: C. V. Mosby Co., 1990, pp. 585-593.
2. BLCX-BLLUMINK. M. Relapses among leprosy patients treated with multidrug therapy: experience in the Leprosy Control Program of the All Africa Leprosy and Rehabilitation Training Center (ALERT) in Ethiopia: practical difficulties with diagnosing relapses; operational procedures and criteria for diagnosing relapses. Int. J. Lepr. 60(1992)421-435.
3. BLCX-BLLLMINK, M. and BERHE, D. Occurrence of reactions, their diagnosis and management in leprosy patients treated with multidrug therapy: experience in the Leprosy Control Program of the All Africa Leprosy and Rehabilitation Training Center (ALERT) in Ethiopia. Int. J. Lepr. 60(1992)173-184.
4. BECX-BLEUMINK., M., BERHE, D. and 'T. MANNETJE, W. The management of nerve damage in the leprosy control services. Lepr. Rev. 61(1990)1-11.
5. BERNINK, E. H. M. and VOSKENS, J. F. J. Study on the detection of leprosy reactions and the effect of prednisone on various nerves. Indonesia. Lepr. Rev. 68(1997)225-232.
6. BOERRIGTER, G., PÖNNIGHAUS, J. M., FINE, P. E. M. and WILSON. R. J. Four-years follow-up results of a WHO-recommended multiple-drug regimen in paucibacillary leprosy patients in Malawi. Int. J. Lepr. 59(1991)255-261.
7. BRANDSMA. J. W. Terminology in leprosy rehabilitation and guidelines for nerve function assessment. Trop. Geogr. Med. 46(1994)88-92.
8. BRANDSMA, J. W., HEERKENS, Y. F, LAKERVELD-HEYL. K. and VAN MISCHNER, C. D. The international classification of impairments, disabilities and handicaps in leprosy-control projects. Lepr. Rev. 63(1992)337-344.
9. DE RIJK, A. and BYASS, P. Field comparison of l0-g and 1-g filaments for the sensory testing of hands in Ethiopian leprosy patients. Lepr. Rev. 65(1994)335-340.
10. DE RIJK. A., GABRE, S., BYASS. P. and BERHANU, T. Field evaluation of WHO MDT fixed duration at ALERT. Ethiopia: the AM FES project-1. MDT course completion, case holding and another score lor disability grading. Lepr. Rev. 65(1994)320-332.
11. KETS. C. M., VAN LEERDAM, M. E., VAN BRAKEL, W. H., DEVILLE, W. and BERTELSMANN, F. W. Reference values for touch sensibility thresholds in healthy Nepalese volunteers. Lepr. Rev. 67(1996)28-38.
12. KIRKWOOD, B. R. Essentials of Medical Statistics. Oxford: Blackwell Scientific, 1988.
13. KUIPER, M. and SCHREUDERS, T. The predictive value of sensation testing in the development of neuropathic ulceration on the hands of leprosy patients. Lepr. Rev. 64(1994)253-261.
14. LE GRAND. A. Women and leprosy: a review. Lepr. Rev. 68(1997)203-211.
15. LIENHARDT, C. and FINE, P. E. M. Type 1 reaction, neuritis and disability in leprosy. What is the current epidemiological situation? Lepr. Rev. 65(1994)190-203.
16. NAAFS. B. Treatment of reactions and nerve damage. Int. J. Lepr. 64 Suppl. (1996)s21-s28.
17. NAAFS. B., PEARSON, J. M. H. and BAAR, A. J. M. A follow-up study of nerve lesions in leprosy during and after reaction using motor nerve conduction velocity. Int. J. Lepr. 44(1976)188-197.
18. NAAFS, B., PEARSON, J. and WHEATE, H. Reversal reaction: the prevention of permanent nerve damage; comparison of short- and long-term steroid treatment. Int. J. Lepr. 47(1979)7-12.
19. NOORDEEN, S. K. and SRINIVASAN, H. Epidemiology of disability in leprosy. I. A general study of disability among male leprosy patients above fifteen years of age. Int. J. Lepr. 34(1966)159-169.
20. PEARSON, J. The use of corticosteroids in leprosy. Lepr. Rev. 52(1981)293-298.
21. PÖNNIGHAUS, J. M. and BOERRIGTER, G. Are 18 doses of WHO/MDT sufficient lor multibacillary leprosy; results of a trial in Malawi. Int. J. Lepr. 63(1995)1-7.
22. PÖNNIGHAUS, I. M., BOERRIGTER, G., FlNE, P. E. M., PÖNNIGHAUS, J. M. and RUSSELL, J. Disabilities in leprosy patients ascertained in a total population survey in Karonga District, northern Malawi. Lepr. Rev. 61(1990)366-374.
23. REED, N. K., VAN BRAKEL, W. H. and REED, D. S. Progress of impairment scores following commencement of chemotherapy in multibacillary leprosy patients. Int. J. Lepr. 65(1997)328-336.
24. RICHARDUS, J. H., FINLAY, K. M., CROFT, R. P. and SMITH, W. C. S. Nerve function impairment in leprosy at diagnosis and at completion of MDT : a retrospective cohort study of 786 patients in Bangladesh. Lepr. Rev. 67(1996)297-305.
25. SAHA, S. P. and DAS, K. K. Disability pattern amongst leprosy cases in an urban area (Calcutta). Indian J. Lepr. 65(1993)305-314.
26. SMITH, W. C. S. The epidemiology of disability in leprosy including risk factors. Lepr. Rev. 63 Suppl. (1992)23s-30s.
27. SRINAVASAN, H. and NOORDEEN, S. K. Epidemiology of disability in leprosy. 2. Factors associated with low disability. Int. J. Lepr. 34(1966)170-174.
28. SUGUMARAM, D. S. T. Steroid therapy for paralytic deformities in leprosy. Int. J. Lepr. 65(1997)337-344.
29. THAPPA, D. M, KAUR, S. and SHARMA, V. K. Disability index of hands and feet in patients attending an urban leprosy clinic. Indian J. Lepr. 62(1990)328-337.
30. TOUW, E. M. J., BRANDSMA, J. W. and ANDERSEN, J. G. Treatment of ulnar and median nerve funciton loss in borderline leprosy. Lepr. Rev. 55(1984)41-46.
31. VAN BRAKEL, W. H. and KHAWAS, I. B. Nerve damage in leprosy: an epidemiological study of 396 patients in West Nepal-part 1. Definitions, methods and frequencies. Lepr. Rev. 65(1994)204-221.
32. VAN BRAKEL, W. H. and KHAWAS, I. B. Silent neuropathy in leprosy: an epidemiological description. Lepr. Rev. 65(1994)350-360.
33. VAN BRAKEL, W. H. and KHAWAS, I. B. Nerve function impairment in leprosy: an epidemiological and clinical study-part 2: Results of steroid treatment. Lepr. Rev. 67(1996)104-118.
34. VAN BRAKEL, W. H., KHAWAS. I. B. and LUCAS, S. Reactions in leprosy: an epidemiological study of 386 patients in west Nepal. Lepr. Rev. 65(1994)190-203.
35. WATSON, J. M. Disability control in a leprosy control programme. Lepr. Rev. 60(1989)160-177.
36. WATSON, J. M. Essential Action to Minimise Disability in Leprosy Patients. London: The Leprosy Mission, 1986.
37. WORLD HEALTH ORGANIZATION. International classification of impairments, disabilities and handicaps. Geneva: World Health Organization, 1980.
38. WORLD HEALTH ORGANIZATION. A guide to leprosy control. Geneva: World Health Organization, 1988.
P. A. M. Schreuder, M.D., M.Se., Leprosy Control Center Region 6, Khon Kaen, Thailand.
Reprint requests to Dr. Schreuder at his present address: NSL Medical Officer, East Java Leprosy Control Project. Provincial Health Office, Jl. Karangmenjatlgan No. 22, Surabaya 60285, Indonesia.
Received for publication on 3 February 1998.
Accepted for publication in revised form on 17 April 1998.