- Volume 66 , Number 2
- Page: 190–200
Serial Mitsuda tests for identification of reactional tuberculoid and reactional borderline leprosy forms
ABSTRACT
The authors studied the Mitsuda reaction in 37 leprosy patients (18 reactional tuberculoid, 19 reactional borderline cases) and compared the results with clinical findings, histopathology and bacilloscopy. Evaluation of the Mitsuda reaction was carried out on days 30, 60, 90 and 120. Most of the reactional tuberculoid patients showed a Mitsuda reaction of +++ in opposition to the reactional borderline patients who showed only +. Bacilloscopic analysis revealed that in 75% of the reactional tuberculoid cases there were rare or no bacilli; bacilli were present in 95% of the reactional borderline cases. The authors conclude that reactional tuberculoid cases have a greater ability to clear bacilli than reactional borderline cases, and that the Mitsuda reaction is a useful tool for the differentiation between these two types of leprosy.RÉSUMÉ
Les auteurs ont étudié la réaction de Mitsuda chez. 32 patients atteints de lèpre: 18 cas tuberculoidcs réactionnels et 19 cas borderlines réactionnels. Ils ont comparé les résultats obtenus avec les données cliniques, histopathologiques et bacilloscopiques. La réaction de Mitsuda fut évaluée au jours 30, 60, 90 et 120. La grande majorité des patients tuberculoidcs réactionnels ont montré une réaction de Mitsuda +++, contrastant avec les patients borderlines réactionnels, qui ont montré seulement une réaction gradée +. L'analyse bacilloscopique a révélé que dans 75% des cas tuberculoidcs réactionnels, il y avait soit une absence, soit de rares bacilles; les bacilles étaient présents dans 95% des cas borderlines réactionnels. Les auteurs concluent que les cas tuberculoidcs réactionnels présentent une capacité à éliminer les bacilles plus importante que les cas borderlines réactionnels, et que la réaction de Mitsuda est un test intéressant à employer pour différencier ces deux types de lèpre.RESUMEN
Los autores estudiaron la reacción de Mitsuda en 37 pacientes con lepra (18 tuberculoidcs reaccionales y 19 casos intermedios reaccionales) y compararon los resultados con los hallazgos clínicos, hislopatológicos y baciloseópicos on esos pacientes. I.a evaluación de la reacción de Mitsuda se hizo a los días 30, 60, 90 y 120. La mayoría de los pacientes tuberculoidcs reaccionales mostraron una reacción de Mitsuda de 3+, en comparación con los pacientes intermedios reaccionales que tuvieron una reactividad promedio de l+. Los análisis baciloseópicos revelaron que el 75% de los casos tuberculoidcs reaccionales tuvieron escasos bacilos (o ninguno). Por el contrario, el 95% de los casos intermedios reaccionales tuvieron bacilos. Los autores concluyeron que los pacientes tuberculoidcs reaccionales tuvieron mayor capacidad para eliminar bacilos que los pacientes intermedios reaccionales y que la reacción de Mitsuda es una herramienta útil para la diferenciación entre estos dos tipos de lepra.According to the 1953 Madrid classification (28) leprosy presents two polar types, tuberculoid and lepromatous, and two groups, indeterminate and borderline.
The chronic evolution of all clinical forms of leprosy, with the exception of the indeterminate form, may be interrupted by acute episodes and sometimes these may constitute the only manifestation of the disease. When these acute phenomena occur in patients with a high degree of immunity we say that they have the so-called reactional tuberculoid disease, and when there is a lower resistance such cases are called reactional borderline cases (14, 15, 28, 36, 45, 46).
The reactional tuberculoid cases present with a highly positive Mitsuda test, are smear-negative or have only few bacilli, have none or little neural involvement, and do not tend to downgrade toward a more lepromatous form. On the other hand, borderline reactional patients have a weakly positive or negative Mitsuda test, are smear-positive for acid-fast bacilli (AFB), relapse very often without treatment, and have a more unfavorable outcome (35).
These acute cases have always elicited much discussion as to their classification in spite of their differences in some clinical aspects, bacilloscopy, Mitsuda test and evolution. The behavior of the Mitsuda test in these cases is variable (18, 27, 28, 42) and the more positive the test, the more tuberculoid the cases will be (36).
Several classifications for the histology of the Mitsuda test have been proposed, but a general agreement on this issue is lacking (1, 2, 6, 7, 30, 48). All pathologists agree that a positive test needs the existence of a tuberculoid granuloma, but most of them do not take into consideration the presence or absence of bacilli. In addition, some researchers believe that when there are bacilli in the granuloma the test is negative (2, 6, 7, 30, 37). However, this may not be true, and the presence of bacilli inside the macrophages in the granuloma may reflect only an inability of these cells to cope with the bacilli until the moment of the reading of the test, that is, on day 28.
In this sense, Convit, ei al. (16) in 1972, using a suspension with 640 million heat-killed bacilli per milliliter, noted that lepromatous patients and Mitsuda-negative contacts were not able to clear bacilli from tissues in contrast to tuberculoid patients who could do so.
Thomas, et al. (47) in 1980 studied leprosy patients with different forms of the disease diagnosed according to Ridley and Jopling's classification (41). Their purpose was to characterize in detail the histologic features of the Mitsuda test and its relationship with the clinical examination and the presence of bacilli in the histological preparations. Bacilli disappeared after 21 days in tuberculoid (TT) patients. The clearance of bacilli was not complete in the borderline tuberculoid (BT) group in spite of similar histological aspects. The bacilli persisted in 9 of 12 patients. The authors found a high number of bacilli in the borderline lepromatous (BL) and lepromatous (LL) forms.
According to these facts and taking into consideration the great similarity between the reactional tuberculoid and reactional borderline forms of the disease, the difficulty in their differentiation, and the importance of the evaluation of the capacity for the clearance of bacilli, we decided to study the behavior of the Mitsuda test in these two forms with the purpose to contribute to their differentiation and to observe the relationship to prognosis and therapy.
PATIENTS AND METHODS
We reviewed the charts of 104 leprosy patients from the files of the Lauro de Souza Lima Institute, Bauru, Brazil, who had been diagnosed as reactional tuberculoid and reactional borderline cases, following our own criteria based in part on the Madrid Congress Classification Commission (28). All of them had had an acute onset of their lesions. Reactional tuberculoid cases presented with erythematous, raised, well-edged papules, nodules and plaques all over the body; little or no neural involvement, skin smears were negative or had few bacilli, and a Mitsuda test was positive. A histopathological picture of these cases showed a well-developed tuberculoid granuloma with edema inside and outside the cells, sometimes touching the epidermis; few or no bacilli were detectable.
The reactional borderline cases showed erythematous and edematous raised papules, nodules and plaques (some of them with edges not so sharply defined as in the tuberculoid cases), in general with pronounced edema of the extremities and with several nerves involved. Skin smears of the lesions were always positive and the Mitsuda test was negative or weakly positive. The histopathological picture showed marked edematous epithelioid granulomas filling a great part of the dermis and separated from the epidermis by a Unna band. Bacilli were always present.
All of the patients were contacted but only 37 agreed to participate in the study. There were 19 females and 18 males, aged 12 to 74 years. Eighteen patients were classified as reactional tuberculoid (Group 1) and 19 as reactional borderline patients (Group 2) (Figs. 1 and 2).

Fig. 1. Reactional tuberculoid leprosy
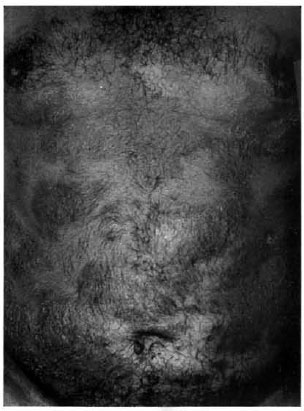
Fig. 2. Reactional borderline leprosy
The patients were submitted to dermatológica! and neurological evaluation, and smears and biopsies for bacteriological and histopathological evaluation were taken from the residual lesions. Clinical photographs that were taken at the beginning of their treatment were repeated at the same sites. Most of the patients exhibited only regressive lesions.
In all of the patients, 0.1 nil human lepromin antigen (6 x 106 bacilli/ml) produced at the Lauro de Souza Lima Institute was injected intradermally into four sites, two in each arm. Each site was chosen between the two points previously tattooed with Nankin ink (Fig. 3). The results of the skin tests were registered at four intervals (days 30, 60, 90 and 120), taking into consideration the clinical, histopathologic and bacillary aspects.
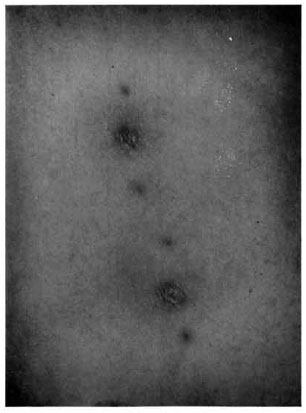
Fig. 3. Mitsuda reaction.
Clinical readings were made by the same person following criteria adopted by the World Health Organization (WHO) (49): (-) negative; (±) doubtful, infiltration less than 3 mm; (+) papule between 3 and 5 mm; (++) papule larger than 5 mm; (+++) papule equal to 10 mm or more with our without ulceration.
Five-millimeter punch biopsies were made for histologic and bacillary readings. In negative results, a more central area between the Nankin ink tattooed points was selected for taking the biopsy. The specimens were fixed in 10% formol and stained by the hematoxylin and eosin (H&E) and Faraco-Fite (17, 19) methods.
Histological classification criteria for the Mitsuda tests was that proposed by Fleury (1, 26, 48):
| Class | Histlogical classification of lepromin test |
| 1 | None or nonspecific chronic, focal inflammation |
| 2 | Chronic inflammation with histiocytes scattered along collagen fibers |
| 3 | Chronic, nontuberculoid. granulomatous inflammation |
|
4 |
Chronic, tuberculoid granulomatous inflammation |
|
4a. Inflammation occupying a dermal area less than 0.25 of the total dermis |
|
| 4b. Inflammation occupying a dermal area 0.25 to 0.50 of the total dermis | |
| 4c. Inflammation occupying a dermal area 0.50 to 0.75 of the total dermis | |
| 4d. Inflammation occupying a dermal area larger than 0.75 of the total dermis |
Classes 1, 2 and 3 were considered as negative, and class 4 was considered positive. Positives 4a and 4b were considered weakly positive; subclass 4c was considered moderately positive, and subclass 4d was considered strongly positive.
The criteria for registration of bacillary load in the histologic specimens was the bacterial index (BI) (39) adapted to this type of examination (48). Bacilli in the necrotic areas were not considered (39).
An analysis of valiancy (31) to compare the groups and intervals related to the sizes of the Mitsuda reactions was done.
Nonparanietric statistical methods of analysis (24) were selected for the histologic and bacilloscopic aspects of the Mitsuda test, mainly: a) Mann-Whitney method, to compare the groups separately at each interval; b) Friedmann method, to compare intervals in each group with calculation of statistics χ2 and p; c) Spearman correlation coefficient at each interval, to study the association among clinical and histological variables. Statistics were considered significant when a p value was <0.05.
RESULTS
The clinical readings in millimeters and the histological and bacillary values of the Mitsuda tests in the two groups which were obtained on days 30, 60, 90 and 120 are shown in Tables 1 and 2.
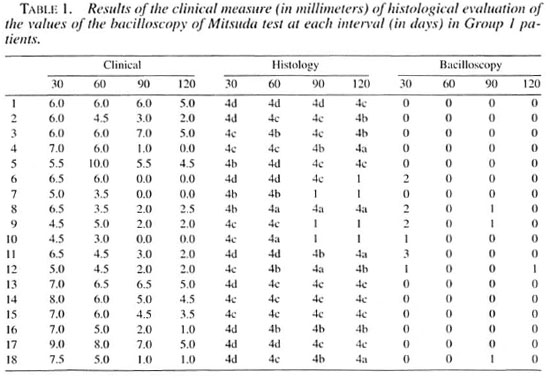
Group 1 (reactional tuberculoid) showed 100% positive skin tests at the intervals corresponding to days 30 and 60. Positive (++) tests were found in 77.78% of the cases on day 30. The intensity of these results decreased gradually at subsequent intervals.
Group 2 (reactional borderline) showed 73.69% positive skin tests at the three intervals; 63.6% of them were equal to one plus (+). In 21.05% of the patients in this group the results were negative and 5.26% doubtful. The positive results also decreased at subsequent intervals.
In summary, according to the clinical results, the values for the Mitsuda reaction decreased along the time of observation in the two groups, the values for Group 1 being higher than for Group 2. Table 3 and Figure 4 show the statistical evaluation of the clinical results of the Mitsuda test.
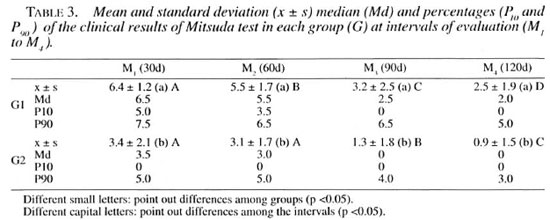
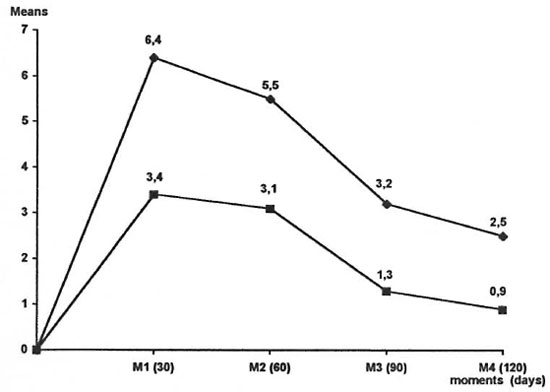
Fig. 4. Means of clinical results of Mitsuda test at each interval in Groups 1 and 2.  = Group 1;
= Group 1;  = Group 2.
= Group 2.
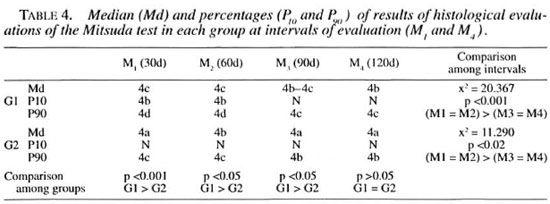
The histological results of the Mitsuda test in Group 1 patients showed that the test was always positive on days 30 and 60. In this group, 44.44% of the patients showed a 4d (high) reaction, 38.89% a 4c (moderate) reaction, and only 16.67% of the patients showed a 4b (weak) reaction at day 30. Necrosis occurred in 44.44% of the cases with a 4d reaction (62.50%) and a 4c reaction (28.50%). The intensity of the reaction gradually decreased at the other intervals.
A histological evaluation showed that in 21.05% of the patients in Group 2 the results were negative. Among 78.95% of the cases with positive results, 36.85% and 21.05% showed 4a and 4b (weak) reactions, respectively; 15.79% showed a 4c (moderate) reaction and only 5.26% showed a 4d (strong) reaction. These figures decreased at the other intervals.
Negative and weakly positive values (4b and 4a, respectively) predominated strongly in Group 2 cases at all intervals. The statistical results are found in Table 4.
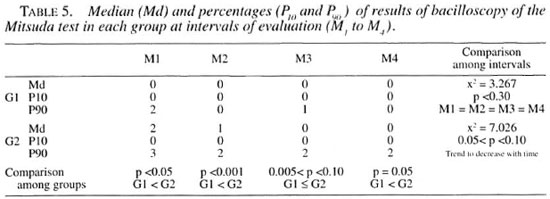
In Group 1 patients, 33.33% had positive results and among them only 5.5% showed results equal to (+++). Negative results were found in all cases at day 60. However, positive results were still found in 16.67% of the cases at day 90, but all with values equal to one plus (+). On day 120, only one patient presented a result equal to one plus (+).
In Group 2 patients, 73.69% had positive results, ranging from (+) to (+++). Positive bacteriological findings on days 60, 90 and 120 were 68.42%, 47.37% and 42.11%, respectively.
Positive bacteriological results were lower in Group 1 than in Group 2 patients at all intervals. There were no differences among the intervals in Group 1 patients, but a trend in decreasing of the bacillary load with time was observed in Group 2 patients. Statistical analysis of the bacteriological findings are given in Table 5.
DISCUSSION
Of the 37 patients studied, 81.09% were aged 31 to 60, and there were no differences between the sexes.
Reactional cases, in which the acute episodes are the disease itself, differ in several aspects. Edema of the extremities, neural involvement and malaise are most frequent in reactional borderline patients. There are also other differences from the bacterial, histopathological, immunological and evolutionary points of view. However, nowadays these cases are labeled as a single condition-reversal reaction-and the reactional tuberculoid is regarded as an old-fashioned term and not used.
Nevertheless, it is important to establish the differences that really exist between them because they, in fact, help to better understand Hansen's disease and these differences have implications in the therapeutics. It is often difficult to distinguish between the two due to their similarities. Therefore, the Mitsuda test could be a mainstay in identifying these clinical forms.
Clinical evaluation of this reaction was established by WHO (49). For a long time, the Mitsuda test has been utilized as an indirect criterion of resistance to infection with Mycobacterium leprae. In addition, from a histological point of view, a positive result is the finding of a tuberculoid granuloma and, in general pathology, it is well known that resistance to an infectious agent corresponds also to the presence of a tuberculoid granuloma (11, 22, 29, 32). Taking into consideration such facts, it could be useful to look for a correlation between the clinical aspects of these reactional cases and several features of the Mitsuda test.
In the first place, the size of clinical infiltration of the Mitsuda test was compared with the histological fraction. For this purpose the method of evaluating the Mitsuda test introduced by Fleury in 1987 based on Trindade (48), Arruda (1), Lastoria and based on Ridley's biopsy index (25, 26) was used.
Our results showed that after 30 days, 81.25% of the clinically positive, two plus (++) Mitsuda reactions presented a histological picture corresponding to moderate and strongly positive reactions, that is, the granuloma occupied fractions of the dermis between 0.5 and 0.75 and larger than 0.75, respectively.
On the other hand, 50.15% of the clinically positive, one plus (+) reactions showed a histologically weak positive result, with the granuloma occupying an area of dermis smaller than 0.5. Taking into consideration a positivity of the test in both groups, an association in 93.75% of the cases was demonstrated.
The clinical and histological results of the Mitsuda test were positive in all of our reactional tuberculoid cases (Tables 1 and 3) in accordance with the results of several authors (14, 18, 27, 35, 36, 47).
In 1940, Souza Campos (43) admitted that the Mitsuda test in reactional tuberculoid patients might be negative or weakly positive. Several authors also admitted the same thing (4, 13, 20, 21, 38). However, Cochrane (14) only admitted as reactional tuberculoid those cases with a positive Mitsuda reaction. Cases with a negative result were labeled by him as intermediate. Later, in 1947, Souza Lima and Souza Campos (43) reported different clinical results of the Mitsuda test in those cases. They found 22.34% negative results: in 3.4% the results were doubtful, 22.34% showed (+) results, 32.19% showed positive (++) results, and 19.31% showed positive results equal to (+++). These authors, taking into account the great variability of results of the Mitsuda test in reactional tuberculoid cases, also admitted that those cases with negative results might be considered as borderline. Other authors had the same opinion, and some of them admitted as reactional borderline also those cases with a weakly positive Mitsuda reaction (5, 12, 13, 20, 28, 35, 44, 45).
Therefore, many authors in the 1940s already considered that true reactional tuberculoid cases would have a positive Mitsuda test, would be more resistant to infection by M. leprae and, consequently, would have a more favorable evolution of the disease (14, 45). Reactional borderline cases, on the other hand, would be those cases with a negative or only weakly positive Mitsuda reaction with less resistance to M. leprae, and would have a less favorable evolution as well. Therefore, it is evident that early authors already admitted the possibility of the Mitsuda test to separate the reactional tuberculoid cases from the reactional borderline cases.
The results of our present study confirm these suppositions. In the reactional tuberculoid group there was the highest grade of positivity of the Mitsuda test whereas the reactional borderline group showed more weak or negative results. We obtained (+) and (++) positive results in Group 1. Most of them were (++) with histologically moderate and strong grades (Table 1). The mean of the results showed a moderate positivity (Table 3). These data agree with those of Opromolla, el al. (36) who took into consideration only values equal to or higher than 6 mm to identify this form of leprosy. These results also enable us to place the reactional tuberculoid cases at the tuberculoid pole of the disease.
On the other hand, in the reactional borderline group (Table 2) the amount of positive reactions was also high but the great majority showed only weak positivity. In this group the mean value of the Mitsuda reactions corresponds to weak positivity, lower than the reactional tuberculoid group.
The presence of necrosis is another feature that must be considered in the Mitsuda test. Schujman (42) observed necrosis in strongly positive Mitsuda reactions, and several other authors also reported this finding (22, 23, 26, 30, 37). However, the occurrence of necrosis was considered of no significance by Michalany and Michalany in 1983 because it occurred only in 54% of their cases (30).
In our Group 1 patients, 44.44% showed necrosis in the Mitsuda reaction. Necrosis occurred in 62.50% of the patients with more strong 4d and in 28.50% with 4c histological grades after 30 days. We did not observe necrosis in the reactional borderline group where weakly positive 4a and 4b reactions predominated. These results showed that there was a good correlation between necrosis and a histologically positive Mitsuda test, and its occurrence was more frequently observed in cases with more strong reactions.
Bacillary evaluation was considered to have great value, mainly related to the concept of lysis or lysis speed which is the same as clearance of bacilli (3, 8, 9, 34), The presence of bacilli in the Mitsuda test was more frequent in the reactional borderline group (Tables 1, 2, 5).
Of the reactional tuberculoid cases, 77.78% showed negative results or the presence of only a few bacilli on day 30. This suggests that these patients were able to clear the bacilli during this period. On the other hand, 22.22% of the reactional tuberculoid patients with bacilli at day 30 cleared them afterward so that at day 60 they showed negative results or only the rare presence of bacilli.
Bacilli were present in 73.69% of the reactional borderline cases at day 30 (Table 2), but if we consider the cases who were negative at day 30 and who at the other intervals showed the presence of bacilli, the number increases to 94.74%. The analysis of the presence of bacilli on other days of observation also showed a trend to decrease their numbers.
These facts suggested a different speed of clearance of bacilli and, consequently, a different "power" in dealing with them. As to this point a striking difference between the two groups was noted (Table 5). If these results would be extrapolated to the clinical situation, reactional borderline cases would have a lower ability to clear bacilli than would reactional tuberculoid cases.
The amount of bacilli in the histological sections of the Mitsuda test correlated with the size of the granuloma. Negative reactions and small granulomas showed more bacilli. Thus, the higher the ability to eliminate bacilli, the larger the granuloma.
Analyzing the reactional tuberculoid group (Table 1), there was decrease of positivity of the Mitsuda test at later intervals but the test remained positive until day 120. Similar behavior was observed in the reactional borderline group. In addition, there was a reduction in the histological reaction at later intervals and a progressive diminution in the number of bacilli as well.
These facts may suggest that the inflammatory reaction diminishes progressively in intensity as the bacilli are eliminated. More intense reactions remain longer even when bacilli are absent. It is also possible that the lysis of bacteria releases antigens which maintain the reaction. The latter explanation was proposed by Hadler (22) in 1953. In addition, this may occur in the lesions during the evolution of the disease as well, that is, the persistence of granuloma even after the disappearance of bacilli.
Reactional tuberculoid and reactional borderline cases are very similar and in many instances it is very difficult to distinguish between them. There are also no conditions with which to evaluate the persistence of bacilli in the lesions in cases under treatment which could help in this differentiation. However, this may be observed through serial Mitsuda tests, where the clearance of dead bacilli probably depends only on the cellular immune response of the patient.
Taking into consideration all of these facts, reactional tuberculoid patients should be linked to the tuberculoid pole of the disease. Ridley (40) when defining his TTs (secondary TT) seems to suggest the same thing.
Another interesting aspect of this study was that inactive patients showed the same clinical, histopathological and bacterial results of the Mitsuda reaction observed in the active phase of the disease.
When each case is evaluated separately it is noted that some patients of the reactional tuberculoid group behave as patients of the borderline group and vice versa. This does not invalidate the general conclusion because there should be different patterns of response of the cellular immune systems of each patient to M. leprae. Thus, a reactional tuberculoid patient may show a reactional pattern very close to that of a reactional borderline patient and, therefore, there is little difference in the granulomatous reactivity and clearance of bacilli. This is impossible to detect with the methodology employed here. However, without treatment minimal differences should be sufficient for reactional tuberculoid patients to be cured and the reactional borderline patients to maintain infection indefinitely or to have a bacterial deterioration with clinical and histological alterations.
Some in vitro studies confirm the statements above. Myrvang, el al. (33) and Bjune, el al. (10) have demonstrated that the polar types and borderline subgroups show different mean values of response to tests of cell-mediated immunity between them. However, inside the same group there are varieties of values with overlapping, and among patients and neighboring subgroups or of a subgroup with an adjacent polar type.
In conclusion, reactional tuberculoid and reactional borderline cases are different. The reactional tuberculoid form should be better evaluated in its response to the Mitsuda test because these patients are more resistant to M. leprae; they have fewer bacilli, they have a more favorable evolution, they are stable, and they do not become worse without treatment.
REFERENCES
1. ARRUDA, M. S. P. Contribuição ao estudos dos imunomoduladores na hanseníase-avaliação de reação de Mitsuda em pacientes portadores de hanseníase virclioviana inativa antes e após imunoterapia. Bauru, 1989. 148 p. Tese (Mestrado) Faculdade de Odontologia de Bauru-Universidade de São Paulo.
2. AZULAY, R. D., ANDRADE, L. M. C, SILVA, C, RABELLO NETO, A. V., AZULAY , J. D., GARRIDO NEVES, R. and MIGUEZ ALONSO, A. Comparison of the macroscopic readings and microscopic findings of the lepromin reaction. Int. J. Lepr. 28(1960)38-43.
3. BARBIERI, T. A. and CORRÊA, W. M. Human macrophage culture; the leprosy prognostic test (LIT). Int. J. Lepr. 35(1967)377-381.
4. BECHELLI, L. M. and QUAGLIATO, R. Teste de Mitsuda na lepra tubereulóide em reação. Rev. Bras. Leprol. 21(1953)51-58.
5. BECHELLI, L. M. and QUAGLIATO, R. Lepra dimorfa ("borderline"); sua classificação. Rev. Bras. Leprol. 28(1960)129-140.
6. BECHELLI, L. M., SOUZA, P. R. and QUAGLIATO, R. Correlação entre os resultados da leitura clínica e o exame histopatológieo de reação de Mitsuda. Rev. Bras. Leprol. 25(1957)21-58.
7. BECHELLI, L. M., SOUZA, P. R. and QUAGLIATO, R. Correlação entre os resultados da leitura clínica e do exame histopatológieo da reação de Mitsuda. Rev. Bras. Leprol. 27(1959)172-182.
8. BEIGUELMAN, B. Leprosy and genetics, a review of past research with remarks concerning future investigations. Bull. WHO 37(1967)461-476.
9. BEIGUELMAN, B. An appraisal of genetic studies on leprosy. Acta Genet. Med. Gemellol. 21(1972)21-52.
10. BJUNE, G, BARNETSON, R. ST.C , RIDLEY, D. S. and KRONVALL, G . Lymphocyte transformation test in leprosy; correlations of the response with inflammation of lesions. Clin. Exp. Immunol. 25(1976)85-94.
11. BUNGELER, W. and FERNANDEZ, J. M. M. Estudo clínico e histopatológieo das reações alérgicas da lepra. Iº parte: Investigações clínicas e histológicas sobre a reação a lepromina (reação de Mitsuda). Rev. Bras. Leprol. 8(1940)157-170.
12. CHATTERJEE , S. N. International classification of leprosy. In: Transactions of the Vllth International Congress of Leprosy, Tokyo, 1958. Tokyo: Japanese Leprosy Foundation, 1958, pp. 30-34.
13. CHAUSSINAND, R. Classification de la lèpre basée sur les exames cliniques, les recherches bactcriologiques et les résultás de la reaction de Mitsuda. In: Memória del V Congresso Internacional de Lepra, Hah/ma, 1948. Habana: Assoeiacion Internacional de la lepra, 1948, pp. 912-915.
14. COCHRANE, R. G. Development of lesions of leprosy with particular reference to tuberculoid leprosy and significance of the lepromin lest. Int. J. Lepr. 8(1940)445-456.
15. COCHRANE, R. G. Complicating conditions due to leprosy. In: Leprosy in Theory anil Practice. Cochrane, R. G. and Davey, T. F., eds. Bristol: Wright, 1964, pp. 331-336.
16. CONVIT, J., AVILA, J. L., GOIHMAN, M. and PINARDI, M. E. A test for the determination of competence in clearing bacilli in leprosy patients. Bull. WHO 46(1972)821-826.
17. FAKACO, J. Bacillos de Hansen e cortes de parafina; methodo complementar para a pesquisa de bacillos de Hansen em cortes de material incluído em parafina. Rev. Bras. Leprol. 6(1938)177-180.
18. FERNANDEZ, J. M. M. Reação leprótica tubereulóide. Rev. Bras. Leprol. 4(1937)425.
19. FITE, G. L., CAMBRE, P. J. and TURNER, M. H. Procedure for demonstrating lepra bacilli in paraffin sections. Arch. Pathol. 43(1947)624-625.
20. GARRIDO NEVES, R. Hanseníase-contribuição aos parâmetros da classificação. Niterói, 1986. 248 pp. lese (Professor Titular) Universidade Federal Fluminense.
21. GATTI, J. C. Lepromino reaeeión en la lepra tuberculoid en reaeeión. In: Memoria del V Congresso Internacional de Lepra, Habana. 1948. Ilabana: Association Internacional de la Lepra, 1948, p. 1273.
22. HADLER, W. A. Comportamento do cobaio e do rato narmais, injetados com lepromina por via intradérmica. Rev. Bras. Leprol. 21(1953)165-194.
23. HADLER, W. A. Influência da inoculação prévia de BCG sobre os resultados da reação de lepromina em cobaios. Bol. Serv. Nac. Lepra 15(1956)5-62.
24. HOLLANDER, M. and WOLFE, D. A. Nonparametric Statistical Methods. New York: J. Wiley, 1973, p. 315.
25. LASTORIA, J. C. Estudo da viragem da reação de Mitsuda em excolares do município de Barra Bonita, São Paulo, após estimulações com BCG e lepromina. Botucatu, 1984. 55 pp. (Tese-Mestrado-Faculdade de Medicina, Universidade Estadual Paulista).
26. LASIORIA, J. C, DILLON, N. L., CRESSONI, B. J. R., FLEURY, R. N., SOARES, F. A. and RIBEIRO, M. A. C. L. Estudo da viragem da reação de Mitsuda em escolares do município de Barra Bonita, São Paulo, após estimulações com BCG e mitsudina. In: Congresso Brasileiro de Dermatologia. 40, Florianópolis, I985. Resumos ... Florianóplis, 1985.
27. LOWE, J. and DHARMINDRA. Studies of lhe lepromin test; restuls of the Mitsuda test in cases of leprosy in different clinical types. Lepr. India 14(1942)3-19.
28. Memoria del VI Congresso Internacional de Leprologia, Madrid, 1953. Madrid: Assoeiacion Internacional de la Lepra, 1953, p. 1344.
29. MICHALANY, J. and MICHALANY, N. S. Patologia da Hanseníase com Especial Referência à Contribuição dos Pioneiros Hansenologistas de São Paulo. São Paulo: Platina, 1988, p. 37.
30. MICHALANY, N. S. and MICHALANY, J. Histopatologia da reação de Mitsuda em adultos sadios não comunicantes de hasenianos. Hansenol. Int. 8(1983)105-123.
31. MORRISSON, D. F. Multivariate Statistical Methods. New York: McGraw Hill, 1967, p. 338.
32. MOTA, I. Atividade imunológica dos linfócitos. In: Imunologia Básica e Aplicada. Bier, O. C., Mota, I., Silva, W. D. and Vaz, N. M., eds. Rio de Janeiro: Guanabara-Koogan, 1977, p. 37-52.
33. MYRVANG, B., GODAL, T., RIDLEY, D. S., FROLAND, S. S. and SONG, Y. K. Immune responsiveness to Mycobacterium leprae and histopathological spectrum of leprosy. Clin. Exp. Immunol. 14(1973)541-553.
34. OPROMOLLA, D. V. A. and FLEURY, R. N. Classification of leprosy. In: Leprosy; Proceedings of the XI International Leprosy Congress, Mexico City, 1978. Amsterdam: Excerpta Medica, 1980, pp. 254-260.
35. OPROMOLLA, D. V. A. and FLEURY, R. N. Formas clínicas. Nocoes de hansenolgia. Centro de Estudos "Dr. Rcynaldo Quagliato." Bauru: Hospital Lauro de Souza Lima. 1981, pp. 84-96.
36. OPROMOLLA, D. V. A., FLEURY, R. N., LASTÓRIA, J. C. and URA, S. The reaclional tuberculoidits position in the classification of leprosy. Quad. Coop. Sanit. 9(1988)59.
37. PETRI, V., MENDES, E. V. and BEIGUELMAN, B. Histology of the Mitsuda reaction of healthy adults with no known contacts with leprosy patients. Int. J. Lepr. 53(1985)540-545.
38. QUAGLIATO, R. Classificacáo de lepra. Madrid, 1953; criterio clínico. Rev. Bras. Leprol. 27(1959)17-32.
39. RIDLEY, D. S. Skin Biopsy in Leprosy; Histological Interpretation and Clinical Application. Basle: Ciba-Geigy. 1977, p. 57.
40. RIDLEY, D. S. Skin Biopsy in Leprosy; Histological Interpretation and Clinical Application. Basle: Ciba-Geigy, 1987, p. 63.
41. RIDLEY, D. S. and Jopling, W. H. Classification of leprosy according to immunity; a live-group system. Int. J. Lepr. 34(1966)255-273.
42. SCHUJMAN, S. Histopalologia de la reacción de Mitsuda; estudio progressivo y comparativo de las reacciones tisulares que provoca en las diversas formas clinicas de lapra. Rev. Bras. Leprol. 4(1936)469-475.
43. SOUZA CAMPOS, N. Lepra tuberculóide reacional. Rev. Bras. Leprol. 8(1940)251-263.
44. SOUZA CAMPOS, N. and RATH DE SOUZA, P. Reactional states in leprosy. Int. J. Lepr. 22(1954)259-272.
45. SOUZA LIMA, L. and MAURANO, F. Reação Leprótica. Rio de Janeiro: Serviço Nacional de Lepra, 1949, pp. 15-50.
46. SOUZA LIMA, L. and SOUZA CAMPOS, N. Lepra Tuberculóide. São Paulo: Renascença, 1947, pp. 173-215.
47. THOMAS, J., JOSEPH, M., RAMANJAN, K., CHACKO, C. J. G. and JOB. C. K. The histology of Mitsuda reaction and its significance. Lepr. Rev. 51(1980)329-339.
48. TRINDADE, M. A. B. Reação de Mitsuda em contatos consanguíneos de doentes de han sentase com formas bacilíferas. São Paulo. 1987. 55 p. (Tese- Mestrado-Escola Paulista de Medicina).
49. WORLD HEALTH ORGANIZATION. Guia para la lucha antileprosa. Genebra: Organización Mundial de la Salud. 1980, p. 110.
1 J. C. Lastoria. Assistant Professor, Department of Dermatology and Radiotherapy.
2 D. V. A. Opromolla, Director, Division of Research and Training.
3 R. N. Fleury, Pathologist, Institute Laura de Souza Lima, Bauru, Sao Paulo, Brazil.
4 F. Habermann, Assistant Professor. Department of Internal Medicine, Botucatu Medical School, UNESP. Rubiao Junior, Botucatu, Sao Paulo, Brazil.
5 P. R. Curi, Pull Professor, Department of Animal Nutrition, Veterinarian Medical School, UNESP, Botucatu, Sao Paulo, Brazil.
Reprint requests to Dr. D. V. A. Opromolla.
Received for publication on 22 April 1996.
Accepted for publication in revised form on 18 March 1998.