- Volume 66 , Number 2
- Page: 201–7
Computed tomographic study of paranasal sinuses in lepromatous leprosy
ABSTRACT
Twenty patients (18 males, 2 females) with lepromatous leprosy and 10 age- and sex-matched controls were subjected to computed tomographic (CT) scans of the paranasal sinuses (PNS). The mean bacterial (BI) and morphological indexes were 3.4+ and 1%, respectively. Nasal symptoms were present in nine (45%) patients; 15 (75%) out of 20 patients showed significant abnormalities on CT scans of the PNS compared to none of the 10 controls. The maxillary and ethmoid sinuses were affected in 11 (55%) patients each, followed by the sphenoid sinus in four (20%) patients. Frontal sinus involvement was least frequent, only one (5%) patient showed CT changes. Mucosal thickening was the most common finding followed by soft-tissue densities and, rarely, a fluid level was seen in the PNS. Involvement of the PNS correlated with a high BI of 4+ or more (75% vs 37.5%). Paranasal sinus involvement is an integral part of lepromatous leprosy since histological involvement was present even when the CT scan was apparently normal.RÉSUMÉ
Les sinus paranasaux (SPN) de vingt patients (18 hommes, 2 femmes) affectés de lèpre Iépromateuse et 10 témoins de même êge et sexe furent examinés par scannographie. L'index bactérien (IB) moyen et l'index morphologique moyen était de 3.4+et 1%, respectivement. Neuf (45%) patients présentaient des symptômes au niveau du nez; parmi ces 20 patients, 15 (75%) montraient des anomalies significatives visibles sur les coupes tomodensitométriques des SPN, alors qu'aucune anomalie n'était visible chez les contrôles. Les sinus maxillaires et ethmoïdes étaient affectés chez 11 (55%) patients chacun, suivi du sinus sphénoïde chez. 4 patients (20%). L'atteinte du sinus ventral était la moins fréquente, seulement un (5%) patient montrait des lésions au tomodensitomètre. Des épaississements de la muqueuse respiratoire étaient la trouvaille la plus fréquente, suivie par des densités de type tissumou et, plus rarement, une accumulation de fluide fut constatée dans les SPN. L'atteinte des sinus paranasaux conviait avec un Ni élevé de 4+ ou plus (75% versus 37,5%). L'atteinte des SI'N est une caractéristique de la lèpre lépromateuse puisque une démonstration histologique de l'atteinte des SI'N était présente même lorsque les coupes tomodensitométriques étaient apparemment normales.RESUMEN
Veinte pacientes (18 hombres y 2 mujeres) con lepra lepromatosa y 10 controles de similar edad y sexo se sometieron al análisis por tomogralía computarizada (CT) de los senos paranasales (PNS). Los índices bacteriano (BI) y morfológico fueron 3.4+ y 1%, respectivamente. Nueve pacientes (45%) tuvieron síntomas nasales; 15 de los 20 pacientes (75%) mostraron anormalidades significativas en las CT de sus PNS. Ninguno de los 10 controles sanos mostraron alteraciones en las CT/PNS. Los senos maxilar y etmoideo estuvieron afectados en 11 (55%) de los pacientes y 4 pacientes (20%) mostraron alteraciones en los senos esfenoideos. La afección de los senos frontales fue la menos frecuente; sólo uno de los pacientes (5%) mostró cambios en la CT de esta parte de la cabeza. El engrasamiento de la mucosa fue el hallazgo más común seguido por opacidad de tejido blando y raramente se observó acumulación de líquido en los PNS. La afección de los PNS es una parte integral de la lepra lepromatosa puesto que llegaron a haber alteraciones histológicas aun cuando la TC fue aparentemente normal.The upper respiratory tract is one of the earliest sites to be involved in lepromatous leprosy which affects the mucosa of the nose, nasopharynx, and larynx (2). Maxillary antral mucosal involvement was reported in a previous study from our institute (3, 4, 6), and its involvement was associated with radiological changes, external nasal deformity and a high bacterial index (BI) (4). Involvement of the ethmoid, frontal and sphenoid sinuses by the lepromatous process has not been documented by direct studies in the reviewed English literature. This may be due to the relative inaccessibility of these areas and proximity to vital structures. In the present study we have used noninvasive computed tomography (CT) to demonstrate changes in the paranasal sinuses.
MATERIALS AND METHODS
Twenty consecutive untreated patients with lepromatous leprosy attending the Leprosy Clinic of Nehru Hospital attached to the Postgraduate Institute of Medical Education and Research, Chandigarh, India, were recruited. The diagnosis was based on clinical examination, slit-skin smears from six sites, and skin biopsy. The Ridley-Jopling (5) classification of leprosy was followed. Patients were questioned about nasal symptoms and the ears, nose and throat were examined. A CT examination was done using Somatome Hi Q (Siemens) and Shimad/At SCT 2000 scanners. Five-mm axial and coronal cuts of the paranasal sinuses (PNS) were taken in all of the patients, and 3-mm sections were taken in the region of the ethmoid sinuses. The age- and sex-matched controls undergoing CT scans for epilepsy or migraine were also studied for PNS. Mucosal thickening, partial or complete opacification, fluid level, polyp or integrity of bony boundaries of PNS were recorded. In the maxillary, frontal and sphenoid sinuses, mucosal thickening was defined as an increase in soft-tissue width along the bony boundaries of the sinus with the presence of air within the sinus. Soft-tissue density was defined as partial or complete opacification of the sinus cavity by a nondependent iso- or hyper-attenuating density. Fluid level was defined as soft-tissue density which formed a level with the air in the sinus in a dependent position. In the ethmoid gallery the presence of soft-tissue densities as defined above was taken to be abnormal when more than one air cell on each side was affected. It was based on results of a CT scan of PNS in the 10 controls.
In two selected patients, one each with abnormal and normal CT findings, an ethmoid sinus biopsy was carried out after informed consent.
RESULTS
Twenty patients (18 males, 2 females) with a mean duration of disease of 28 months formed the study group: 14 patients had lepromatous leprosy (LL) and 6 had borderline lepromatous leprosy (BL). Type 2 reaction [erythema nodosum leprosum (ENL)] was present in 12 LL and type 1 reaction in 2 BL patients. All but two BL patients were smear-positive with a mean BI and morphological index of 3.4+ and 1%, respectively. Nasal symptoms in the form of epistaxis or nasal stuffiness were present in nine (45%) patients.
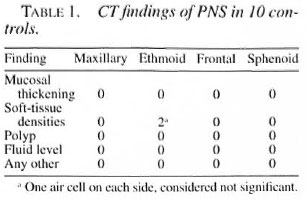
None of the 10 controls showed any abnormality in the CT scans of their maxillary, frontal and sphenoid sinuses. Two controls, however, showed soft-tissue densities in 1-2 air cells in the ethmoid galleries (Table 1).
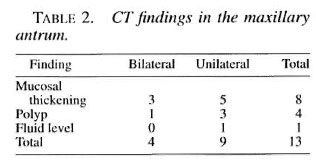
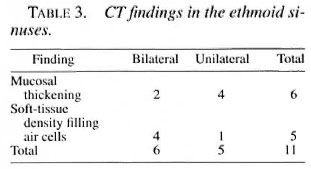
Computed tomography of PNS showed abnormal findings in 15 (75%) patients. Maxillary antrum and ethmoid air cells were involved in 11 (55%) patients each, sphenoid in 4 patients (20%), and frontal in 1 (5%) patient. The maxillary antrum and ethmoid were involved together in 5 patients, and the maxillary antrum and ethmoid alone in 4 and 2 patients, respectively. Two patients showed concurrent involvement of the maxillary ethmoid and sphenoid sinuses, and one each had maxillary antrum involvement in association with the sphenoid and frontal sinuses. Mucosal thickening was the commonest change observed in all PNS: in 8 patients in the maxillary antrum, in 6 patients in the ethmoid cells, and in 1 patient each in the sphenoid and frontal sinuses. The second most common change was soft-tissue densities seen as polyps in the maxillary antrum in four patients. Soft-tissue densities filling the ethmoid cells were seen in five patients; sphenoid sinuses in two patients. A fluid level was noted in one patient each in the maxillary antrum and sphenoid sinuses. CT changes in individual sinuses are summarized in Tables 2-4.

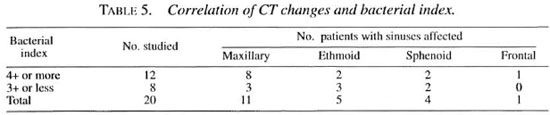
Correlation of CT changes and bacterial load. A BI of 4+ or more was frequently associated with involvement of the PNS, especially the maxillary antrum, compared to patients with a BI of 3+ or less (75% vs 37.5%; p >0.05, Table 5).
Correlation of CT changes and nasal symptoms. Eight out of nine patients with clinical symptoms showed PNS involvement on a CT scan.
Histological changes. An ethmoid sinus biopsy showed changes consistent with lepromatous leprosy with large numbers of acid-fast bacilli (AFB) in both patients, including the one with an apparently normal CT image.
DISCUSSION
The paranasal sinuses are an important part of the upper respiratory tract since they can produce ideal conditions for the growth of bacteria. They have been studied mostly by X-ray of PNS in occipitomental and occipitofrontal views (''''). All PNS, including the maxillary, ethmoid and frontal sinuses, have been reported to be affected. Maxillary antrum involvement is the commonest observed in 57%-60% patients followed by the ethmoid sinuses (33%) and the frontal sinuses (30%) (3-7). Barton ('), however, reported maxillary sinus involvement in all (100%) of his 16 cases.
The present CT scan study of PNS in leprosy is the first of its kind to the best of our knowledge. CT was chosen for this investigation because it gives a three-dimensional picture. Moreover, the details of soft tissue and opacity (homogenous or heterogenous) and the integrity of adjoining bone can be clearly delineated. A CT scan also can give us a better idea of the PNS pathology by ascertaining the extent and type of disease. The PNS contain air which is a natural contrast and, since these are cross-sectional images, the overlapping of bones which obscures details on plain X-rays is avoided. Pneumatization of sinuses can be assessed better in CT which may be seen as haziness on plain X-rays. The anterior ethmoid cells and sphenoid sinuses are better seen on CT than on plain X-rays. In addition, when both coronal and axial sections are reviewed together the extent of involvement of the PNS can be clearly delineated.
In our present study the involvement of the maxillary sinus was seen in 11 (55%) patients which is in agreement with previous radiological studies. In addition to mucosal thickening, polyps could be seen in four (20%) patients. Ethmoid cells are not easy to visualize in detail on an occipitofrontal view, but CT demonstrated their involvement in 11 (55%) cases. It was frequently associated with involvement of the maxillary antrum because of its proximity. Involvement of the ethmoid on CT was more frequent than previous reports (1, 7) . The involvement of the frontal sinus was least frequent; only one patient showed unilateral mucosal thickening in association with septate maxillary antrum. This is in contrast to reports of frontal sinus involvement in 44% and 30% of cases (1, 7), and may be due to partial pneumati/.ation of the sinuses being interpreted as hazy on plain X-rays. The sphenoid sinus was also involved in four (20%) patients in contrast to the lack of comment in previous reports since it cannot be delineated on plain X-rays. A careful evaluation of the CT scans of PNS in our 10 controls served as a baseline for determining what may be considered as abnormal because none of them showed abnormalities in the maxillary antrum, frontal or sphenoid sinuses. The ethmoid sinuses showed soft-tissue densities in 1-2 air cells in two controls that were considered within normal limits.
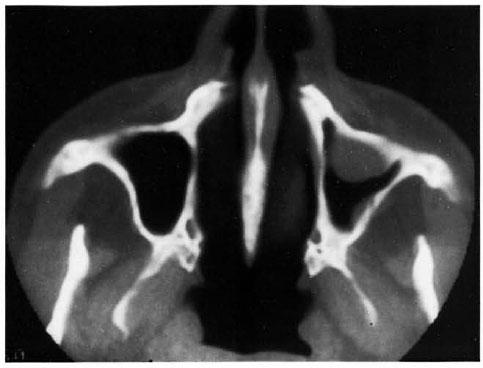
Fig. 1. Axial CT section showing a polyp on the anterior wall and mucosal thickening on the posterolateral wall of the left maxillary sinus.
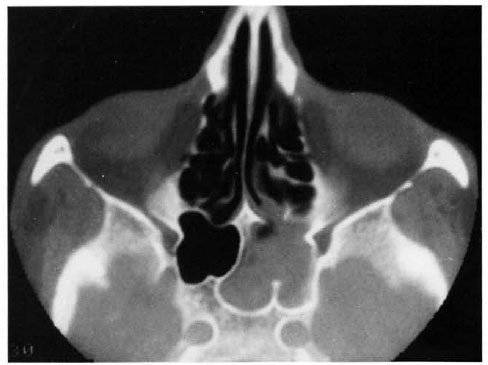
Fig. 2. Soft-tissue density within the left half of the sphenoid sinus.
Radiological abnormalities in the maxillary antrum were associated with histological involvement in 21 (70%) out of 30 cases in our previous report (4). Two patients who underwent ethmoid sinus biopsies showed involvement by the lepromatous process even when CT images were normal. Moreover, all but one patient with nasal symptoms had CT changes, suggesting that involvement of PNS is part and parcel of the upper respiratory tract involvement in lepromatous leprosy. They serve as an important reservoir of infection since a wide surface area is involved, and they may serve as a constant source of reinfection of the nasal mucosa. Further sinuscopic and histological studies are planned in addition to the CT scan of the PNS to validate the above findings.
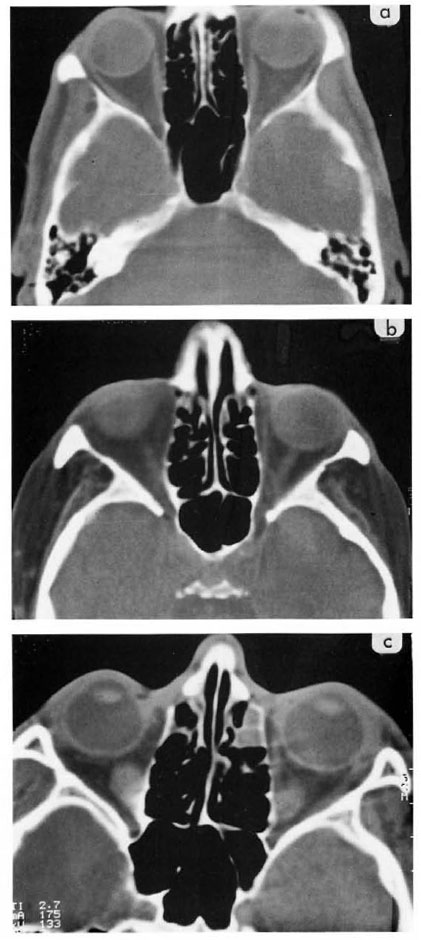
Fig. 3a. Normal axial CT section for ethmoid sinuses. Note bony septas are thin and barely visible. Fig. 3b. Mucosal thickening of the septas within the ethmoid sinus, especially the anterior cells on both sides. Fig. 3c. Soft-tissue density partially or totally obscuring cells in the ethinoid sinuses of both sides.

Fig. 4. Composite sections for the maxillary (top), ethmoid (middle), and frontal (bottom) sinuses. Mucosal thickening is seen in the left antrum and frontal sinuses in addition to soft-tissue densitiesWithin both ethmoid sinuses in leprotnatous leprosy.
REFERENCES
1. BARTON, R. P. E. Radiological changes in the paranasal sinuses in lepromatous leprosy. J. Laryngol. Otol. 93(1979)597-600.
2. BARTON, R. P. F. and DAVEY, T. F. Early leprosy of nose and throat. J. Laryngol. Otol. 90(1976)953-961.
3. HAUHNAR, C. Z., KAUR, S., SHARMA, V. K. and MANN, S. B. S. A clinical and radiological study of maxillary antrum in lepromatous leprosy. Indian J. Lepr. 64(1992)487-493.
4. HAUHNAR, C. Z., MANN, S. B. S., SHARMA, V. K., KAUR, S., MEHTA, S. and RADOTRA, B. D. Maxillary antrum involvement in multibacillary leprosy: a radiologic, sinuscopic and histologic assessment. Int. J. Lepr. 60(1992)390-395.
5. RIDLEY, D. S. and JOPLING, W. H. Classification of leprosy according to immunity: a live-group system. Int. J. Lepr. 34(1966)255-273.
6. SONI, N. K. Antroscopic study of maxillary antrum in lepromatous leprosy. J. Laryngol. Otol. 103(1989)502-503.
7. SONI, N. K. Radiological study of paranasal sinuses in lepromatous leprosy. Indian J. Lepr. 60(1988)285-289.
1 V. K. Sharma. M.D., M.N.A.M.S., Additional Professor., Depart-ment of Dermatology, Venereology & Leprology.
2 J. R. Bapuraj, M.D., P.D.C.C., Assistant Professor. Department of Radiodiagnosis and Imaging.
3 S. B. S. Mann, M.S., M.N.A.M.S., Professor and Head. Department of Otorhinolaryngology. Postgraduate Institute of Medical Education and Research, Chandigarh 160 012, India. Fax: 91-172-540401, 540450, 543078.
4 I. Kaur, M.D., Associate Professor., Depart-ment of Dermatology, Venereology & Leprology.
5 B. Kumar, M.D. M.N.A.M.S., Professor and Head, Department of Dermatology, Venereology & Leprology.
Received for publication on 17 June 1997.
Accepted for publication in revised form on 6 March 1998.