- Volume 66 , Number 4
- Page: 451–6
Incidence of nerve damage in leprosy patients treated with MDT
ABSTRACT
The incidence rates of sensory and motor impairments during and after multidrug therapy (MDT) are reported for a prospective cohort of patients who had no nerve damage at registration (N = 1621). Sensory and motor loss increased with age and both were high among multibacillary patients as compared with paucibacillary patients. The lateral popliteal (common peroneal) and posterior tibial nerves seem to be most affected for sensory loss; whereas the posterior tibial and ulnar nerves are mainly responsible for motor loss. No significant difference by gender was found. Implications for prevention of disability (POD) activities are discussed and suitable recommendations made.
RÉSUMÉ
Les taux d'incidence des atteintes sensorielles et motrices pendant et après la polychimiothérapie (PCX) sont rapportés à partir d'une cohorte prospective de patients qui ne présentaient pas de lésions nerveuses à l'examen initial (N = 1621). Les pertes sensorielles et motrices augmentaient avec l'âge et elles étaient toutes deux plus élevées parmi les patients multibacillaires que chez les patients paucibacillaires. Les nerfs poplité latéral (péroné commun) et tibial postérieur semblent être les plus souvent affectés par les pertes sensitives tandis que, pour les pertes motrices, les nerfs tibial postérieur et ulnaire sont les plus souvent impliqués. Il n'y avait pas de différence significative entre les deux sexes. Les conséquences pour les mesures de prévention des infirmités (PDF) sont discuttées et des recommendations appropriées sont proposées.
RESUMEN
Se reporta la incidencia de daño sensorial y motor ocurrido durante y después de la poliquimioterapia en pacientes con lepra, que al momento de su registro no tenían daño nervioso (N = 1621). Las disfunciones sensorial y motora aumentaron con la edad y fueron mayores en los pacientes multibacilares que en los paucibacilares. Los nervios poplíteo lateral (peroneal común) y tibial posterior fueron los más afectados en cuanto a pérdida sensorial, mientras que los nervios tibial posterior y ulnar, fueron los más afectados en su función motora. No se encontró ninguna diferencia significativa en relación al sexo de los pacientes. Se discuten algunas acciones para prevenir la discapacidad y se hacen algunas recomendaciones.
The prevention of nerve damage and its consequent disabilities are considered priority concerns in the management of leprosy today (10,17). Compared to the dapsone era, the risk of developing deformity in patients treated with multidrug therapy (MDT) is reported to be lower but to still occur and is correlated with age, type and duration of disease and prior therapy (9,12,15). The fact that impairment of nerve function occurs during and after MDT is a serious concern and requires more intensive studies (2,5). A cohort of leprosy patients were followed up prospectively during and after MDT in Gudiyatham Taluk in Tamil Nadu, India. The magnitude of nerve involvement and associated factors were carefully studied. In this paper, the incidence of sensory and motor impairments during and after MDT among newly detected leprosy patients who had no nerve involvement at registration are reported and the findings discussed.
SUBJECTS AND METHODS
All newly registered leprosy patients (NEW) treated with MDT at Karigiri hospital during July 1990 to December 1992 were included in this cohort study. Further, those currently on MDT [under treatment (UT)] or on surveillance after completing MDT [released from treatment (RFT)] as of 30 June 1990 were added to the cohort. Patients were classified on the basis of clinical features using the Ridley-Jopling scale and further broadly classified as paucibacillary (PB) or multibacillary (MB) (11). The patients were assessed at baseline, at initiation of therapy for NEW patients, at RFT, and every 6 months both during treatment and after RFT for 3 years.
Impairments of nerve functions were assessed for both sensory and motor deficits, using standard methods (16). Sensory testing was done with Semmes-Weinstein monofilaments using the technique described by Bell-Krotoski.
For the hand, the 2-gram filament was used, and sensation was tested at 7 points: 3 in the ulnar distribution area, 3 in the median distribution area, and 1 in the radial nerve area on the dorsum of the thumb web.
For the foot, the 4-gram filament was used, with sensation being tested at a total of 6 points: 5 on the plantar surface in the posterior tibial distribution area, and 1 point on the dorsum of the foot in the lateral popliteal distribution area.
A voluntary muscle test (VMT) was done using the MRC scales, testing only selected muscles for each nerve: ulnar nerve (abductor digiti minimi), median nerve (abductor pollicis brevis), common peroneal or lateral popliteal nerve (tibialis anterior and extensor hallucis longus), posterior tibial nerve (intrinsics of the foot) and facial nerve (orbicularis oculi).
The incidence rates for sensory and motor impairments were calculated separately by dividing the number of persons who were normal at the first assessment but developed (during follow up) new nerve impairments (sensory or motor) by number of persons normal initially and expressed per 1000 person-years.
Data were analyzed on microcomputers using appropriate software. Tests of significance for proportions (Z) and for association (chi-squared) were used.
RESULTS
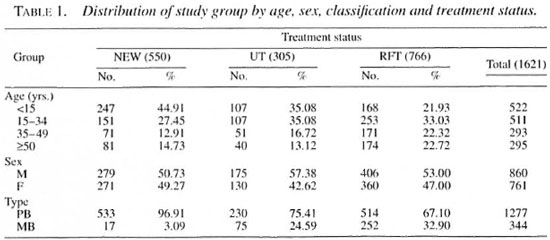
Of 3064 patients examined, 1621 had no nerve impairment at the time of registration and were the subjects of this study. Of these, 550 were NEW, 305 were already on treatment (UT) and 766 had been reJeased from treatment (RFT). Comparisons by age, sex and type of leprosy are shown in Table 1. There were no significant differences in the sex ratio among the three groups, but NEW and UT groups were generally younger as compared to those RFT. MB patients comprised less than 5% among new registrations as compared to 25% in UT and nearly 35% in RFT. Therefore, detailed analyses were done separately by type of leprosy.
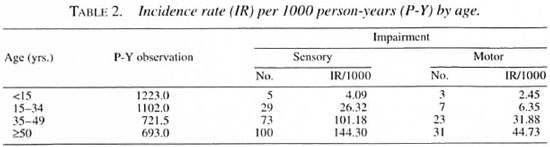
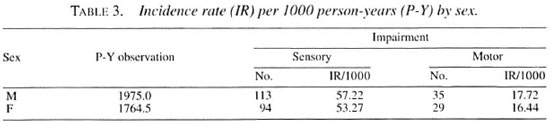
The incidence rates by age and sex are presented in Tables 2 and 3, respectively. A steep increase by age is noted for both sensory and motor loss. There were no significant differences by sex for sensory or motor loss.
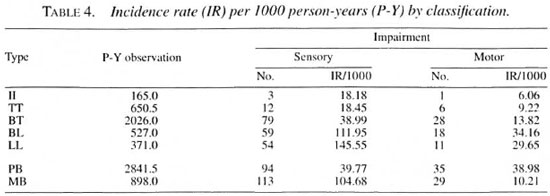
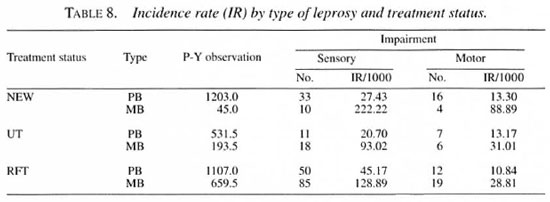
The incidence of both sensory and motor impairment are significantly higher for MB patients, being nearly fourfold for sensory loss and tripled for motor impairments (Table 4).
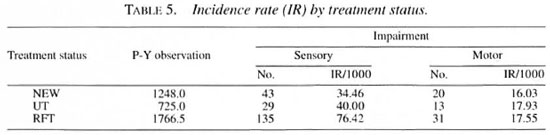
Incidence rates by treatment status are shown in Table 5 which depicts increasing sensory loss from NEW patients to those RFT, but no such change is seen for motor impairments.
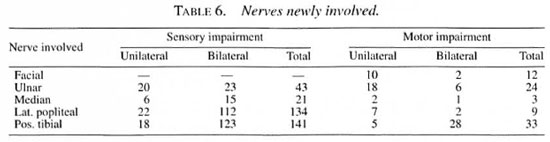
New nerve impairments by type of nerve involved are given in Table 6. The lateral popliteal and posterior tibial nerves seem to be those most affected for sensory loss followed by the ulnar and then the median nerves. The posterior tibial and ulnar nerves seem to be mainly responsible for motor loss. Unilateral facial nerve involvement was also not unusual.
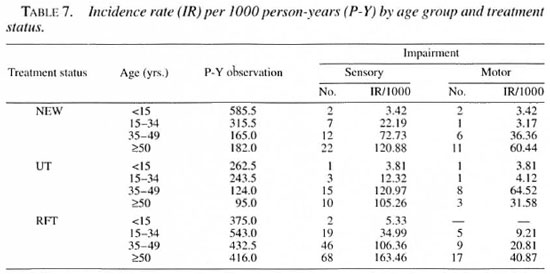
The incidence rates by age and treatment status are presented in Table 7. The gradient by age is maintained in all three groups but the extent seems to vary. There were no differences by sex in any of the three treatment groups.
The incidence rates by type of leprosy in the three treatment groups show consistently higher rates for MB patients (Table 8). The apparently higher sensory loss in new MB patients compared to other groups may be more a function of the small numbers of MB patients seen.
The incidence of reactions and its relationship to nerve damage will be reported in a future communication.
DISCUSSION
Epidemiological studies on the prevalence of disabilities in leprosy have been reported (8,14,16,18). Data on the incidence of disabilities are, however, rather scarce but are more useful in measuring program effectiveness and managing care after cure programs (5,6,13). Peripheral neuropathy may be present before the patient notices any signs or symptoms of nerve function impairment. Early effective chemotherapy is expected to prevent the development of such-nerve damage in new patients. However, antibacterial therapy by itself does not seem adequate to prevent new nerve damage during and after chemotherapy (10). In a study at Chingleput in South India (13), Sundar Rao, et al. reported an incidence of only 0.681 per 1000 person-years during MDT. which is attributed to a high proportion of monolesion cases, early detection of disease, and administration of clofazimine in MB cases. On the other hand, studies in Malawi showed the risk of developing disabilities among patients without any disabilities at registration as 5 per 1000 person-years, which was slightly higher after the completion of treatment than during treatment (9).
The findings of the present study also reveal higher rates in older ages and among MB patients after completion of treatment. The lack of significant differences by gender needs further study. In an epidemiological and clinical study in Nepal, van Brakel and Khawas (16) report that nerve function impairment was not an infrequent complication affecting patients on regular antileprosy treatment. Despite variations in actual rates due to possible differences in testing criteria and selection of patients, it is clear that disabilities do occur at higher rates after rather than during treatment (9,12). This poses a challenge in leprosy control programs to be alert in early detection of reactions and nerve damage in order to prevent disability and deformity.
In the event of neuritis having occurred, the patients respond excellently with steroids, the dosage depending upon the severity and gradually tapered every 2 weeks. When there is a delay in reporting and not much appreciable improvement after steroids, some of these patients are subjected to nerve decompression which has resulted favorably in restoring nerve function.
The present findings are based on patients who showed no signs of nerve impairment at the start of MDT. Sensory impairments were significantly higher as compared to motor loss. Thus, the occurrence of new disability while on treatment and even after completion could dampen the enthusiasm and motivation of patients to continue therapy. This requires adequate patient counseling and education to accept certain inevitable but, hopefully, minor disability. Involvement of the patient and the patient's family in maintaining their confidence to continue appropriate therapy is the essence of a care-after-cure program (1,4). Prevention, detection and management of nerve function impairment should thus be given priority in all field/control activities (3,8). The incidence of disability can be a more valid measure of program effectiveness than prevalence or even incidence of disease in the post-MDT era (13). Further studies on incidence rates of disabilities and their correlates are thus urgently required.
Acknowledgment. We thank all staff, especially physiotechnicians, paramedical workers and their supervisors, for assistance in the field. We are grateful to the Impact Foundation, U.K., for its financial support and to Dr. H. Srinivasan for consultancy.
REFERENCES
1. BECX-BLEUMINK, M. and BERHE, D. Occurrence of reactions, their diagnosis and management in leprosy patients treated with multidrug therapy; experience in the leprosy control program of the All Africa Leprosy and Rehabilitation Training Center (ALERT) in Ethiopia. Int. J. Lepr. 60(1992)173-184.
2. BECX-BLEUMINK, M., BERHE, D. and 'T MANETJE, W. The management of nerve damage in the leprosy control services. Lepr. Rev. 61(1990)1-11.
3. BRANDSMA, J. W., DE JONG, N. and TJEPKEMA, T. Disability grading in leprosy: suggested modifications to the WHO disability grading form. (Editorial). Lepr. Rev. 57(1986)361-369.
4. IYERE, B. B. Leprosy deformities: experience in Molai Leprosy Hospital. Maiduguri. Nigeria. Lepr. Rev. 61(1990)171-179.
5. Job, C. K. Nerve damage in leprosy. Int. J. Lepr. 57(1989) 532-539.
6. KEELER, R. F and RYAN, M. A. The incidence of disabilities in Hansen's disease after the commencement of chemotherapy. Lepr. Rev. 51(1980)149-154.
7. NAAFS, B., PEARSON, J. M. H. and BAAR, A. J. M. A follow-up study of nerve lesions in leprosy during and after reaction using motor nerve conduction velocity. Int. J. Lepr. 44(1976)188-197.
8. NOORDEEN, S. K. and Srinivasan, H. Epidemiology of disability in leprosy. Int. J. Lepr. 34(1966)159-169.
9. PONNIGHAUS, I. M, BOERRIGTER, G., FINE, P. E. M., Ponnighaus. J. M. and RUSSEL,. J. Disabilities in leprosy patients ascertained in a total population survey in Karonga district, northern Malawi. Lepr. Rev. 61(1990)366-374.
10. Proceedings of International Workshop on Leprosy Research, Bangkok, Thailand, 11-13 March 1996. Int. J. Lepr. 64 Suppl. (1996) S1-S92.
11. RIDLEY, D. S. Skin Biopsy in Leprosy. 3rd edn. Documenta Geigy. Basle: Ciba-Geigy Ltd., 1990.
12. SHARMA, P., Kar, H. K., Beena, K. R., Kaur, H. and NARAYAN, R. Disabilities in multidrug leprosy patients: before, during and after multidrug therapy. Indian J. Lepr. 68(1996)127-136.
13. Smith, W. C. S. and PARKHE, S. M. Disability assessment as a measure of progress in leprosy control. Lepr. Rev. 57(1986)251-259.
14. Sundar Rao. P. S. S., Karat, S., Karat, A. B. A. and FURNESS, M. A. Prevalence of deformities and disabilities among leprosy patients in an endemic area. Int. J. Lepr. 38(1970)1-11.
15. Sundar Rao. P. S. S., Subramanian, M. and Sub-RAMANIAN, G. Deformity incidence in leprosy patients treated with multidrug therapy. Indian J. Lepr. 66(1994)449-454.
16. VAN BRAKEL, W. H. and Khawas, I. B. Nerve damage in leprosy: an epidemiological and clinical study of 396 patients in West Nepal-part I. Definitions, methods and frequencies. Lepr. Rev. 65(1994)204-221.
17. WHO Expert Committee on Leprosy. Seventh report. Geneva: World Health Organization, 1998. Tech. Rep. Ser. 874.
18. Zhang, G., Li. W., Yan, L., Chen, X., Zheng, T. and Ye, G. An epidemiological survey of deformities and disabilities among 14.257 cases of leprosy in 11 counties. Lepr. Rev. 64(1993)143-149.
1. M.B.B.S., D.Ortho.. M.S.(Ortho.), Head.
2. M.Sc., Bio-Statistician.
3. M.B.B.S., Medical Officer. Branch of Surgery.
4. M.A., M.P.H.. Dr.PH., F.S.S.. F.S.M.S., Director. Schieffelin Leprosy Research and Training Center. Karigiri 632 106. N.A.A. District, Tamil Nadu. India.
Reprint requests to Dr. P. S. S. Sundar Rao at the above address or FAX 91-416-74274.
Received for publication on 16 September 1998.
Accepted for publication in revised form on 28 October 1998.