- Volume 66 , Number 4
- Page: 457–63
Monitoring the elimination of leprosy in Brazil
ABSTRACT
A decreasing trend in the prevalence rate of leprosy was reached in Brazil only after the introduction of the World Health Organization multidrug therapy (WHO/MDT) program in 1990. This paper analyzes leprosy morbidity indicators and the prevalence rate, and their utilization in monitoring the progress of leprosy elimination in Brazil. Since these indicators are modified by changes in health service procedures, comparing prevalence rates f rom different endemic countries or current prevalence rates with old ones f rom the same endemic region needs careful attention. The current official prevalence rate of 6.72/10,000 in-habitants in Brazil could be considered high when compared with rates f rom other countries, but it is important to remember that defaulters and patients being treated with old regimens are kept on the active registers in Brazil, while in most other endemic countries they are not.RÉSUMÉ
C'est seulement après l'introduction en 1990 du programme de polychimiothérapie recommendé par l'Organisation Mondiale de la Santé (PCT-OMS) que la prevalence de la lèpre a eu tandance à diminuer au Brésil. Cet article analyse les indicateurs de morbidité, le taux de prevalence de la lèpre, et leur utilisation pour le suivi des progrès de l'élimination de la lèpre au Brésil. Comme ces indicateurs soute changés par les modifications des procédures des services de santé, il apparait que la comparaison des taux de prevalence d'un pays endémique à l'autre ou des taux actuels et anciens de prévalence dans une même région endémique doit être faite avec la plus grande prudence. Le taux actuel officiel ile prévalence du Brésil de 6.72/10.000 habitants pourrait être considéré comme élevé si on le compare à d'autre pays. Cependant, il est important de garder à l'esprit que les personnes dont le suivi a été perdu et les patients traités avec les prescriptions anciennes restent inscrits aux registres au Brésil alors que. dans les autres pays, ils ne le restent pas.RESUMEN
En Brasil se alcanzó una disminución en la prevalência de lepra sólo hasta después de la introducción de la poliquimioterapia propuesta por la Organización Mundial de la Salud (OMS/PQT). en 1990. Este artículo analiza los indicadores de morbilidad y prevalência de la lepra y su utilidad en el monitoreo del progreso de su eliminación en Brasil. Puesto que estos indicadores son modificados por câmbios en los procedimientos de los servidos de salud. las comparaciones de las tasas de prevalência en diferentes países endémicos o de las tasas de prevalência actual con las tasas anteriores en una misma region endémica deben hacerse con mucha cautela. La prevalência oficial actual de 67.2/10.000 habitantes en Brasil pudiera considerarse alta en relación a las tasas de prevalência en otros países, sin embargo, es importante recordar que en Brasil, tanto los pacientes desertores como los tratados con esquemas anteriores se mantienen inscritos en los registros oficiales, y que esto no ocurre en la mayoría de los otros países endémicos.The aim of leprosy-endemic countries is to have a rate of 1 case per 10,000 inhabitants by the year 2000 (10). In the process of eliminating leprosy as a public health problem, care given to patients must be based on the primary health care network, offering World Health Organization multidrug therapy (WHO/MDT) to the largest number of patients possible. Among the 16 countries containing 90% of the known cases in the world, Brazil, India, Nepal, and Mozambique are in the unconfortable position of having had the highest prevalence rates during the last few years when compared with other endemic countries (10).
Since the prevalence rate has been chosen as the main morbidity indicator in monitoring the Leprosy Elimination Program, it is necessary to discuss how this coefficient is being calculated. Comparing the prevalence rates from different endemic countries, or the current prevalence rates with the old prevalence rates series from the same endemic region, needs careful attention. Changes in health service procedures as well as the implementation of new regimens of treatment of shorter duration and changes in the definitions of what is an active leprosy case modify this indicator.
Apart from the above, countries like Brazil which have many social and regional differences present certain specific problems. Some Brazilian states and regions have the technical and managerial structure to carry out a control program, based on case finding and case holding (including prevention of disabilities), while others, without the necessary structure, have difficulty in coping with the leprosy problem.
This work aims at analyzing the leprosy morbidity indicator, the prevalence rate and its use in monitoring the progress of the elimination program in Brazil.
MATERIALS AND METHODS
The data used in this analysis comes from a historical series of new cases, defaulters and registered cases based on reports by the National Leprosy Program (1,4,9). The prevalence rates which are shown begin in 1959 (no data before this year could be found).
According to the National Leprosy Program policy, the active register on 31 December of each year represents the total number of active leprosy cases. The total numbers of active leprosy cases are cases from the previous year (under control and defaulters) plus those registered in the reference year (new cases, transfers and relapses). It does not include the cases discharged (cures, deaths, diagnoses not confirmed, duplicates of clinical records, statistical discharges) in the same year (7).
The prevalence rates are based on the total number of active leprosy cases in the active register living in the political division (state) requiring specific treatment. The numerator of the prevalence rate, by definition, is the number of cases on treatment or under control (i.e., at least one visit in the reference year) and also those not under control (i.e., no visit in the reference year, or defaulters).
In Brazil, the active leprosy register of the health care services includes those patients who were under the old therapeutic regimen during the 1976-1990 period. Adding to that, the register took into account those patients who were using the WHO/MDT regimen.
The prevalence rates (including defaulters in the numerator) were quite stable between 1959 and 1975, remaining at about 13.0/10,000 inhabitants. After 1976 the trend increased, reaching a peak of 18.8/10,000 inhabitants in 1990. Since then there has been a decrease in the prevalence rate, which stood at 6.72/10,000 in 1996, the lowest value ever recorded (The Table; Fig. 1).
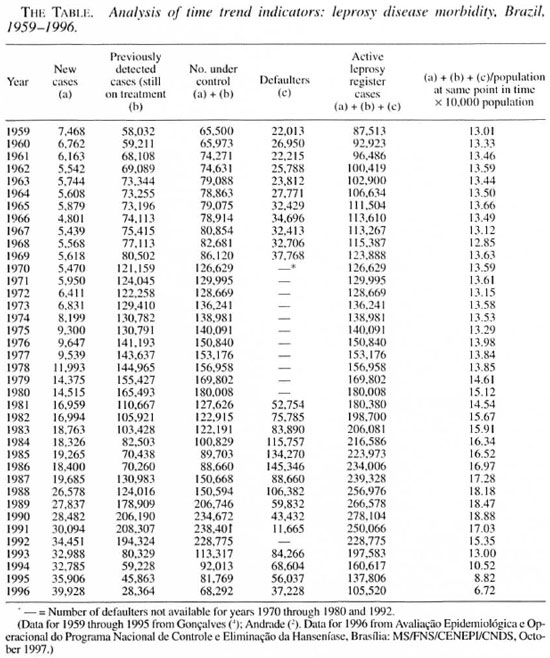
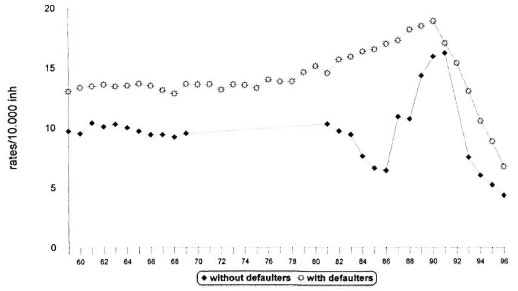
Fig. 1. Leprosy prevalence rates, Brazil, 1959-1996. Data for 1959 through 1995 from Goncalves (4); Andrade (2). Data for 1996 from Avaliação Epidemiológica e Operacional do Programa Nacional de Controle e Eliminação da Hanseníase. Brasilia: NIS/FNS/CENEPI/CNDA, October 1997. (______) = Number of defaulters not available for years 1970 to 1980 and 1992.
A progressively decreasing trend has been observed in the prevalence rates. Major changes in the definition of a case of leprosy might be considered as the main explanation. The Brazilian government policy definition estimates prevalence rates with defaulters in the numerator (Fig. 1). As expected, if one compares both rates-with and without defaulters in the numerator-a statistically significant difference between them can be observed (5). Thus, these rates may be considered independent.
Regarding cured cases, their release from the active register was 24.3% in 1987, 64.9% in 1994, and 58% in 1996 among the total number of cases on the registers. Interestingly, the largest increase occurred during the post-1991 period. Several important modifications for the release-from -treatment criteria were defined at that time. In the same period there was a decrease in prevalence rates (Fig. 2).
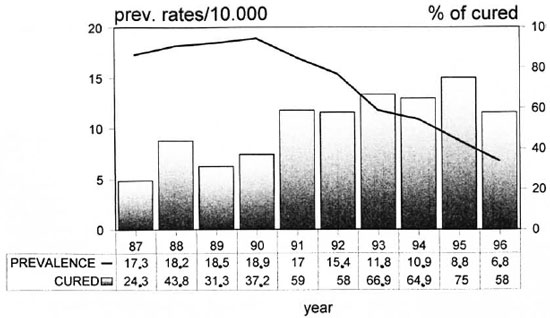
Fig. 2. Leprosy prevalence and cured rates, Brazil, 1987-1996. Data from MS/FNS/CENEPI/CNDS.
Figure 3 shows the relationship between the detection rate of new cases and the degree of disability between 1987 and 1996. During the 1982-1987 period, the mean detection coefficient was 1.42/10,000 inhabitants. From 1987, this indicator increased, reaching three peaks: 1.84/10,000 inhabitants in 1988, 2.30/10,000 inhabitants in 1992, and 2.54/10,000 inhabitants in 1996.
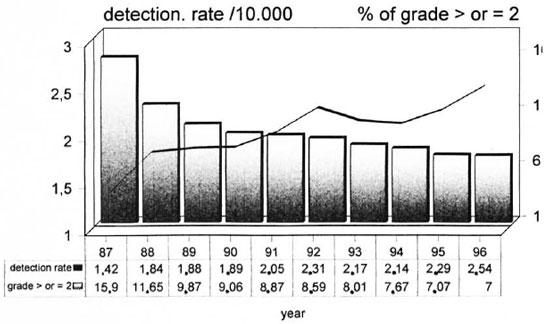
Fig. 3. Leprosy detection rates and disability grades, Brazil, 1987-1996. Data from MS/FNS/CENEPI/CNDS.
Throughout all of these periods, new cases were detected earlier than before, while the number of new cases having disabilities at the time of diagnosis continued to decrease. This suggests a general decline in the pool of infection(3).
DISCUSSION
From an analysis of the trends, the decreasing leprosy prevalence rates in Brazil during the period 1959 to 1996 followed an increase in the detection of new cases. It can be observed that the increased detection over the period 1987 to 1996 followed an important increase of the number of patients released from the active register and a decrease in the number of new cases with disabilities in the same period. The growth in the detection coefficient of new cases parallels the implementation of several new strategies to control this disease (3).
The current official prevalence rate of 6.7/10,000 in Brazil could be considered high when compared with other countries, but it is important to remember that defaulters and patients being treated with the old regimen are still kept on the active registers. In some endemic countries, defaulters are not counted in the numerator of the prevalence rate. This must be taken into consideration when comparing prevalence rates from different countries.
The practice of maintaining these defaulting patients on the active registers, where they are counted in the numerator of the prevalence rate, is certainly a major reason for the apparent high prevalence rates in Brazil. It is interesting to note that there have not been marked differences in the number of defaulters between the dapsone monotherapy period and the WHO/MDT regimen era (which began in 1986), despite the emphasis on patient follow up with the later regimen (2).
Nonstandardized procedures for discharging patients from the active treatment registers and the difficulties in recovering irregular attendance could create a misunderstanding of the actual prevalence, defined as the total number of cases on the active registers. It could cause an overestimation of the number of patients who actually need treatment and, consequently, an overestimation of the magnitude of the leprosy problem in Brazil. This should be considered when comparisons are made with other endemic countries which are using standardized WHO definitions of a prevalent leprosy case.
Interpreting changes in the prevalence rates must be done with caution because of changes in health service procedures. Differences in definition and/or interpretation of what is an active case of leprosy and the criteria used for releasing patients from treatment and MDT coverage should be considered.
In 1991, when WHO/MDT was implemented in Brazil, many old cases were already receiving older treatments which lasted longer. Thus, when prevalence rates were calculated, these long-registered cases were included in the numerator. Four years after the implementation of WHO/MDT as the official treatment, 25% of the patients in the active treatment registers were still receiving some other regimen. By 1996, this had fallen to 11%.
The old regimen, known in Brazil as D.N.D.S., consisted of a daily 100 mg dapsone dose (until clinical cure) or 100 mg of clofazimine per day (for those suspected of having dapsone-resistant disease) plus 600 mg rifampin daily for 3 months for lepromatous or borderline cases. These patients were treated for another 5 years after becoming inactive before the drugs were discontinued, and then there was a follow up of 5 more years without any specific treatment (6).
Indeterminate and tuberculoid cases were treated only with dapsone or clofazimine (100 mg per day until clinical cure). The Mitsuda-negative, indeterminate cases were treated for 5 years after the disease had become inactive, and there was a follow up for 5 more years. There was a follow up of the Mitsuda-positive and tuberculoid patients of 11 years after becoming inactive (6). These policies made it difficult to declare patients cured and thus remove them from the register, and they have resulted in a backlog of patients found in the prevalence rates, until the beginning of the 1990s.
The implementation of a therapeutic regimen in leprosy to a population base has a well-documented effect on prevalence. This indicator is also affected by several revisions to patient release procedures adopted by health care systems. The subsequent decline in the prevalence coefficient, beginning in 1991, could be explained by the gradual increase in WHO/MDT coverage and in the percentage of those struck off the active register due to discharge upon cure. One may consider that from 1991 to 1993 multibacillary (MB) cases were under the WHO/MDT regimen until smear negativity. However, they were still kept on the register and under surveillance for 5 more years. Those paucibacillary (PB) cases who took 6 monthly doses within a period of 9 months were followed up for 2 more years until released.
It is important to note that after 1993 policies for discharging patients from the active register became a lot less strict, including the new criteria for cure, MB treatment for 24 doses in 36 months of WHO/ MDT, and PB 6 doses within 9 months (8).
One of the most important changes in health procedures which contributed to the decrease in the period that patients were kept on the register was the redefinition of borderline tuberculoid (BT) cases as PB cases (previously all BT cases were classified as MB cases) and those indeterminate Mitsuda-negative cases were classified and treated as MB cases (8).
Thus, the period for which patients were kept on the active register and the date of release were dependent upon clinical classification and the duration of the regimen adopted. Until 1993 the criteria of posttreatment observation was also taken into account. Since the beginning of the WHO/MDT regimens, the period for which patients were kept on the register has decreased steadily, reaching 2.6 years in 1996. Simultaneously, WHO/MDT coverage increased by over 200% (from 24% in 1991 to 89% in 1996).
CONCLUSIONS
The leprosy elimination program is assessed through activities related to the care of patients under treatment. This needs a more accurate evaluation of who actually needs treatment. This has to be implemented at a local level and it is an activity which is not easily monitored by National Leprosy Program managers. When comparing prevalence rates (as used in Brazil) and prevalence rates which use, in the numerator, only the cases under control (Fig. 1), it seems clear that current prevalence rates are not an accurate measure of comparison between different leprosy elimination programs.
Brazil, with its many social and regional differences, presents certain specific problems. Some states and regions have a technical and managerial structure able to carry out a control program based on case finding and case holding (including prevention of disabilities) while other states and regions do not have the necessary resources required to cope with the leprosy problem.
An effective leprosy surveillance system should be based on a state's or even a city's desegregated data analysis. Compilation of data could help eliminate the inequalities and thus provide guidance in giving appropriate interventions to different needs.
Acknowledgment. We are grateful to Prof. Dr. M. Lechat, Prof. Dr. Elizabeth Moreira, and to S. Lyons for their suggestions which improved the quality of this paper.
REFERENCES
1. ANDRADE, V. L. G. Evolução da hanseníase no Brasil e perspectivas para sua eliminação como um problema de saúde pública, doctoral thesis. Brazilian School of Public Health, Oswaldo Cruz. Foundation. Rio de Janeiro. Brazil. 1996.
2. ANDRADE, V. L. G. Casos em abandono do tratamento inflando o coeficiente de prevalência da Hanseníase. Bol. Pneumol. Sanit. 5(1997)30-42.
3. ANDRADE, V. L. G., ALBUQUERQUE, M. F. M. and SABROZA, P. C. The importance of operational factors for the interpretation of indicators in the Hansen's disease endemic in Brazil. Acta Leprol. 10(1997)131-139.
4. GONÇALVES, A. Epidemiología e controle da hanseníase, Brasil. Bol. Oficina Panam. Saúde 102(1987)246-256.
5. KLEINMAN, J. C. Infant Mortality, Statistical Notes for Health Planner. Vol. 2. Washington, DC.: National Center for Health Statistics, 1976.
6. MINISTÉRIO DA SAUDE, BRASIL. Guia para o Controle da Hanseníase. 2nd ed. Brasília: Centro de Documentação do Ministério da Saúde. Secretaria Nacional de Programas Especiais de Saúde/Divisão Nacional de Dermatologia Sanitaria. 1984.
7. MINISTÉRIO DA SAÚDE, BRASIL,. Instrumento de Avaliação do Programa de Controle e Eliminação da Hanseníase. Brasília: Fundação Nacional de Saúde/Centro Nacional de Epidemiologia/Coordenação Nacional de Dermatologia Sanitária/MS, 1994 (mimeo).
8. MINISTÉRIO DA SAÚDE, BRASIL. Guia para o Controle da Hanseníase. Brasília: Fundação Nacional de Saúde. Centro Nacional de Epidemiologia/Coordenação Nacional de Dermatologia Sanitária. 1994.
9. MINISTÉRIO DA SAÚDE, BRASIL. Avaliação Epidemiológica e Operacional do Program Nacional de Controle e Eliminação da Hanseníase. Brasília: Fundação Nacional de Saúde/Centro Nacional de Epidemiologia-Coordenação Nacional de Dermatologia Sanitária/Ministério da Saúde. 1997 (mimeo).
10. WORLD HEALTH ORGANIZATION. Progress towards the elimination of leprosy as a public health problem. Wkly. Epidemiol. Rec. 20(1996)149-156.
1. M.D., M.Sc, Ph.D.. Ministry of Health, Brazilia, Brazil.
2. M.D., M.Sc, Professor, Samuel Pessoa Department. Escola Nacional de Saúde Publica. Fundação Oswaldo Cruz, Rio de Janeiro, Brazil.
3. M.D., M.Sc., Ph.D.. Collective Health Studies Department. Fundação Oswaldo Cruz. Clinical Medicine Department. Universidade Federal de Pernambuco, Recife. Brazil.
4. M.D., M.Sc., Dermatologia Sanitária R.J., Rio de Janeiro, Brazil (deceased).
Reprint requests to Dr. Vera Andrade, Rua Gal. Glicerio 82, Apt. 704. Laranjeiras. Rio de Janeiro. 22245 120 RJ. Brazil.
Received for publication on 15 January 1997.
Accepted in revised form on 14 October 1998.