- Volume 66 , Number 4
- Page: 445–50
Sensitivity and specificity of methods of classification of leprosy without use of skin-smear examination
ABSTRACT
A 12-month cohort of 2664 new leprosy cases in Bangladesh has been analyzed to provide information about the sensitivity and specificity of two different methods of classifying leprosy into paucibacillary (PB) and multibacillary (MB), if the results of skin-smear examination are not taken into account. The two methods are: 1) a procedure based on counting skin lesions recommended by the World Health Organization (WHO) (<6 skin lesions = PB, >6 skin lesions = MB); and 2) the "Bangladesh method" (<10 skin and nerve lesions = PB, >10 skin and nerve lesions = MB). In the latter system, any degree of nerve enlargement is taken to be a nerve lesion. The WHO method was found to be 89% sensitive and 88% specific at detecting smear-positive MB cases f rom among the cohort; the Bangladesh system, 92% sensitive and 88.6% specific. The WHO method did not detect 18 smear-positive cases as MN; the Bangladesh method left 13 smearpositive cases unclassified as MB. Several of these "missed" (false-negative) cases had a high bacterial index. The WHO system of classifying leprosy cases as MB is simple to apply and has a reasonable balance between sensitivity and specificity. However, it must be recognized that the system will lead to a small but significant number of skin-smear-positive MB cases being treated with a PB treatment regimen.
RÉSUMÉ
Une cohorte de 2664 nouveaux cas de lèpre au Bangladesh, sur une période de douze mois, a été analysée dans le but d'obtenir des renseignements sur la sensibilité et la spécificité de deux différentes méthodes de classification de la lèpre: paucibacillaire (PB) versus multibacillaire (MB), quand l'examen du suc dermique n'est pas pris en compte. Les deux méthodes sont les suivantes: 1 ) une procédure basée sur le dénombrement des lésions cutanées recommendée par l'Organisation Mondiale de la Santé (OMS) (<6 lésions cutanées = PB, >6 lésions cutanées = MB); et 2) la "méthode bangladaise" (<10 lesiones cutanées et nerveuses = PB, >10 lesiones cutanées et nerveuses = MB). Selon ce dernier système, tout degré d'épaississement d'un nerf est considéré comme lésion nerveuse. Cette étude a montré que la méthode de l'OMS présentait une sensitivité de 89% et une spécificité de 88% pour la détection des cas MB positifs à l'examen du suc dermique. Le système bangladais pour sa part était sensible à 92% et spécifique à 88.6%. La méthode de l'OMS n'a pas détecté 18 cas de lèpre MB positifs au test du suc dermique; la méthode bangladaise n'a pas permis de classer comme MB 13 cas positifs au test du suc dermique. Plusieurs de ces cas "manques" (faux négatifs) présentaient des index bactériens élevés. La système de classification des cas de lèpre de l'OMS est simple à appliquer et présente un équilibre raisonnable entre senstivité et spécificité. Cependant, il faut raeonnaître que ce nouveau système aura comme conséquence la présence d'un nombre réduit, mais significatif, de cas MB positifs au test du suc dermique qui seront traités avec un traitement destiné aux patients PB.
RESUMEN
Se estudiaron 2664 casos nuevos de lepra en Bangladesh para determinar la sensibilidad y especificidad de dos métodos de clasificación de la lepra como paucibacilar (PB) o multibacilar (MB) que no toman en cuenta los exámenes baciloscópicos. Los dos métodos son: 1) un procedimiento recomendado por la Organización Mundial de la Salud (OMS) basado en la cuenta de las lesiones en la piel (<6 lesiones = PB, >6 lesiones = MB); y 2) "el método Bangladesh" (<10 lesiones en piel y nervios = PB, >10 lesiones en piel y nervios = MB). En el último método, cualquier grado de afección nerviosa se toma como lesión. Se encontró que la sensibilidad del método de la OMS fue del 89% y su especificidad del 88% (al hacer referencia a los datos bacteriológicos); el sistema Bangladesh tuvo una sensibilidad del 92% y una especificidad del 88.6%. El método de la OMS no detectó 18 casos bacteriológicamente positivos; el método Bangladesh dejó fuera 13 casos bacteriológicamente positivos. Varios de estos casos "falsos negativos" tuvieron indices bacteriológicos correspondientes a casos MB. El sistema de la OMS es simple de aplicar y está razonablemente balanceado en sensibilidad y especificidad. Sin embargo, debe reconocerse que la aplicación de este método puede ocasionar que un pequeño pero significativo número de casos MB sean tratados como PB.
The classification of leprosy is closely linked to chemotherapy as seen in the pre-multidrug therapy (MDT) era, when the Ridley-Jopling system (9) was used to determine the duration of dapsone therapy. The introduction of MDT in 1982 included a revised and simplified classification into two groups, multibacillary (MB) and paucibacillary (PB) (16). MB was classified using skin-smear results when the bacterial index (BI) was >2+. This was revised by the World Health Organization (WHO) Expert committee in 1988 (13) so that the finding of a positive smear at any site led to MB classification. In 1993 the WHO Study Group suggested that clinical methods alone could be used for classification where facilities for skin smears were unavailable or unreliable (15).
The quality of skin smears and of microscopy has been found to be one of the weakest links in most leprosy control programs (13). Becx-Bleumink has drawn attention to the undue emphasis placed on skin-smear examinations, and in the conclusion of her detailed analysis of leprosy classification at ALERT, Ethiopia, stated that "... patients can be classified based on clinical signs and, hence, in the absence of skin-smear services for routine classification purposes." (1).
Between 1993 and 1997 some clinical methods were developed based upon the numbers of skin lesions, nerve lesions and body areas affected, or combinations of these (11). In Bangladesh, the national program guideline classified as MB those cases whose total number of skin patches and palpably enlarged nerves ("nerve lesions") is 10 or more and/or the skin smear is positive and classified as PB those cases where total number of skin patches and nerve lesions is less than 10 and which are smear negative (12). This system of classification was in place until the end of 1997. The Bangladesh Technical Guide states: "... absence of skin smear examination facility should not be considered as contra-indication for commencement of MDT in detected cases." Some leprosy control programs in Bangladesh do not have access to a skin-smear examination facility and so they rely on the purely clinical grounds described above to classify leprosy as MB or PB for treatment purposes, while others do have access to such facilities and so routinely use the skin-smear result as an adjunct to classification.
The WHO is now advocating the use of a similar clinical system to classify leprosy that may be used in the absence of a skinsmear examination facility. This system classifies patients having six or more skin lesions as MB and less than six skin lesions as PB (l4). This system of classification was introduced into Bangladesh on 1 January 1998.
The limitation of using a purely clinical system for classifying leprosy cases is that a paucilesional smear-positive case will be falsely classified as PB and will receive inadequate chemotherapy, with the attendant risk of relapse. On the other hand, large numbers of smear-negative patients would be classified as MB and treated accordingly. This has to be weighed against the gains of making MDT available to a larger population without the expense and complication of a skin-smear examination service.
In this paper, a large data base of leprosy cases is analyzed to determine the proportion of paucilesional smear-positive cases that will be missed if classification is dependent on a count of skin/nerve fesions alone. This study makes no use of histopathology in the classification of leprosy, but regards a classification system based on clinical and bacteriological findings as the "gold standard." It is recognized that this is not as sensitive as a system using skin and nerve biopsy. However, at the field level it is not practical to use histopathological services for anything other than research. The possible impact on leprosy control is discussed.
MATERIALS AND METHODS
The Danish-Bangladesh Leprosy Mission (DBLM) is a large leprosy control project covering four districts of northern Bangladesh with a total population of 5.5 million, an area known to have a high prevalence of leprosy (8). DBLM follows the Bangladesh national guidelines for leprosy classification and treatment as described earlier. All newly detected leprosy cases had body charts drawn and slit-skin smears taken by leprosy control assistants (LCAs). Skin smears were taken from one earlobe and two active skin patches, or from both earlobes and the forehead if a clear skin lesion could not be identified. Confirmation of diagnosis and prescription of MDT are then made by an experienced leprosy control supervisor (LCS) based on the clinical findings, classifying as PB or MB according to the protocol described earlier. The skin smears were read at one of DBLM's two laboratories in Nilphamari or Thakurgaon, and the results posted back to the field, where the classification was changed if a "PB" case was found to be smear positive. The result entered was the average BI calculated by adding the results from each site and dividing by 3. Fractions were rounded up to the next whole integer.
The following nerves were routinely palpated by field staff and the degree of enlargement recorded: facial, supra-orbital, great auricular, supraclavicular, radial, ulnar, median, radial cutaneous, ulnar cutaneous, common peroneal (lateral popliteal), infrapatellar, musculocutaneous, sural and posterior tibial. Enlargement in any degree of one of these nerves was regarded as a "nerve lesion" and counted toward the total number of lesions used in classifying as PB or MB.
DBLM has a computer data base of all its registered leprosy cases (26,000). The cohort of cases registered between 1 April 1995 and 31 March 1996 constitutes the study group for the Bangladesh Acute Nerve Damage Study (BANDS), a prospective cohort study aimed at investigating the epidemiology and response to treatment of acute nerve damage in leprosy. The computer data base includes fields recording the number of skin patches and nerve lesions as well as smear results. This data base, which has been regularly audited, has been analyzed in a simple manner to show the difference in the number of cases that would be classified as MB or PB, depending on whether or not skin-smear results are taken into account.
The computer data base is written in Microsoft FoxPro for Windows, version 2.6. Statistical analysis was carried out using Epi Info version 6.01.
RESULTS
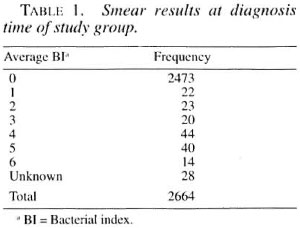
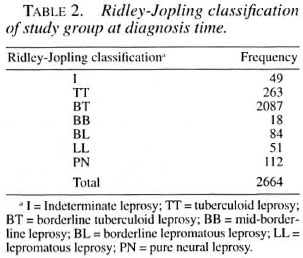
Table 1 shows the numbers of patients with different BIs. A total of 163 patients were smear positive, with a majority of the positive cases (98, 60.1%) having an average BI of 4+ or more. A smear result was not available for 28 cases who were all small children for whom smear taking proved impossible in the clinical setting. These 28 cases have been excluded from the study group, leaving a total of 2636 who were analyzed using different mathematical filters. Table 2 shows the Ridley-Jopling classification of the patients at diagnosis, with the addition of the indeterminate (I) and pure neural (PN) groups recognized by the Indian classification (6).
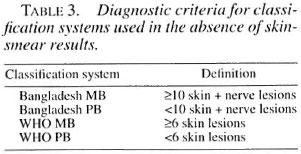
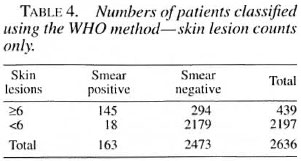
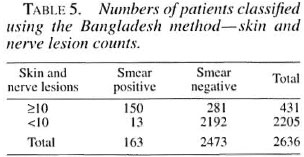
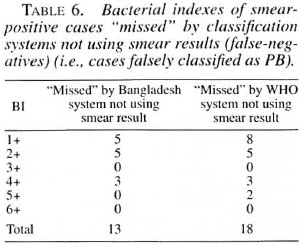
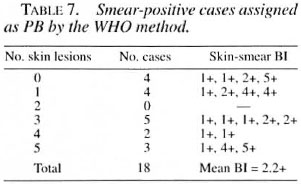
The two different classification systems are summarized in Table 3. Tables 4 and 5 show the results of classifying the cases by the WHO and Bangladesh classification systems without using smear results. The sensitivity of the WHO system compared with the "gold standard" of smears was 89.0% and the specificity was 88.1%. Using the Bangladesh system, the sensitivity was 92.0% and the sensitivity was 88.6%. The average Bis of these "missed" cases are shown in Table 6. Table 7 shows the characteristics of the smear-positive cases assigned PB by the WHO method.
DISCUSSION
The above analysis shows a high degree of concordance between the two methods of classification when smear results are used. Both methods classify approximately the same number of cases as MB (WHO/MB = 439, Bangladesh/MB = 431 out of the study group of 2636). However, the groups do not quite correspond. When the Bangladesh system is used for classification, 34 out of 431 MB cases are classified as PB by the WHO system (7.9%, 95% CI 6.6%-9.2%). Conversely, if the WHO system is used for classification, 42 out of 439 MB cases are classified as PB by the Bangladesh system (9.6%, 95% CI 8.2%-11.0%). Thus, each system of classification excludes nearly 10% of the patients who would be included by the other system. Operationally, it is unlikely that there would be much effect whichever system is used.
There is, however, a small number of smear-positive paucilesional cases who were missed by both classification systems when the smear result was not used. There is a hard core of 13 cases which neither system of classification picked up as MB without the smear result, and an additional five cases if the WHO system is used alone. Thus, 18 out of the total of 163 smear-positive cases would be missed (11.0%, 95% CI 6.2%-15.8%) by the WHO classification system in the absence of smear results and diagnosed as PB. When the Bangladesh system is used alone without smear results, 13 out of the total of 163 smear-positive cases would have been missed (8.0%, 95% CI 3.8%-12.1%). The results indicate that the Bangladesh system of classification, when used without smear results, is slightly more sensitive and specific than the WHO system at detecting smear-positive cases, but the difference is not significant (p = 0.345).
Out of the 18 cases who would have been falsely diagnosed as PB by application of the WHO criteria without using smear results, four cases were recorded as having no skin patches; these were all LL. There were a total of nine lepromatous (BL/LL) cases in this group. The body charts of all these cases show markings of infiltration, so potentially all could have been diagnosed as lepromatous and, thus, MB by alert leprosy control workers or doctors. However, signs of infiltration are often missed and sometimes not noticed until the positive smear result prompts a more thorough examination. A classification system focusing on patch counts alone is very open to this potential oversight.
Groenen, et al. in a clinical/histopathological study carried out in Bangladesh, concluded that skin-smear reading facilities can be perfectly satisfactory, given reasonable supervision (4). In the two hospitals in which their study was carried out (one was DBLM Nilphamari), no positive slides were missed and no BI readings differed by more than one unit from the control in 95% of the cases. They also found that inclusion of skin-smear results would considerably improve the reliability of the classification strategy if the results were used optimally by improving both the specificity and the sensitivity of MB diagnosis (5).
In the DBLM project area, the proportion of smear-positive cases among the total caseload is not high (6.1%), but remains moderately high among MB cases (37.8% of Bangladesh-classified MB cases). However, in other parts of Bangladesh the smear-positive rate among the total cases remains much higher (20%-30%), as in other countries. In such situations, this study indicates that there is likely to be a considerable number of paucilesional smear-positive cases who will be missed by a classification system that relies on counting skin patches (and nerve) lesions alone, possibly resulting in a subsequent relapse.
A prospective study on the effectiveness and safety of WHO/MDT among a cohort of patients in Thailand has recently been published (2). When the authors used a purely clinical classification system (>6 lesions = MB), they found that 12% of the "true" MB patients would be undertreated. They defined MB as cases with clinically diagnosed LL, BL or BB features, or any other cases with a BI of 2+ or more at any site. Their MB classification criteria were more stringent than ours, but the percentage of "missed" (false-negative) paucilesional MB cases is very similar to the 11% we found.
The issue of relapse continues to provoke discussion. Although a relapse after MDT has generally been found to be less than 1%, Jamet, et al. (7) found a 20% relapse rate among patients with a BI of 4+ or more after a long period of follow up. Recently, a bacteriological study found the incidence of viable Mycobacterium leprae extracted from the nerves and skin of 26 MB leprosy patients released from MDT to be alarmingly high (46% from nerves, 23% from skin) (10). Desikan has drawn attention to the risk of relapse after MDT, recommending that attempts must be made to improve the standard of field laboratories rather than closing them down, and suggesting that particular attention should be paid to the issue of MB cases with a high BI at diagnosis (3).
The potential problems of relapse among MB patients with high Bis is likely to be magnified if they only receive PB/MDT. Classification of leprosy using clinical methods without the use of skin-smear examination is less than ideal. Continued use of skin smears is recommended where they are being reliably done. In regions where no bacteriological services are available or of unreliable quality, then both the Bangladesh and WHO methods can be considered. The Bangladesh is marginally more specific and more sensitive than the WHO approach, but the latter is much simpler. The WHO system provides a reasonable balance of sensitivity and specificity. It would be difficult to improve on one without a deterioration in the other. However, the results may be different if applied to different populations.
Although the WHO system of classifying leprosy cases as MB is simple to apply and has a reasonable balance between sensitivity and specificity, it must be recognized that the system will lead to a small but significant number of MB cases being treated with a PB regimen.
REFERENCES
1. BECX-BLEUMINK, M. Allocation of patients to PB or MB drug regimens for the treatment of leprosy: a comparison of methods based mainly on skin smears as opposed to clinical methods; alternative clinical methods for classification of patients. Int. J. Lepr. 59(1991)292-303.
2. DASANANJALI, K., SCHREUDER, P. A. M. and PIRAYAVARAPORN, C. A study on the effectiveness and safety of the WHO/MDT regimen in the Northeast of Thailand; a prospective study, 1984-1996. Int. J. Lepr. 65(1997)28-36.
3. DESIKAN, K. V. The risk of relapse after multidrug therapy in leprosy. (Editorial). Lepr. Rev. 68(1997)114-116.
4. GROENEN, G., SAHA. N. G., RASHID, M. A., HAMID, M. A. and PATTYN, S. R. Classification of leprosy cases under field conditions in Bangladesh. 1. Use-fulness of skin-smear examinations. Lepr. Rev. 66(1995)126-133.
5. GROENEN, G. SAHA, N. G. RASHID. M. A., HAMID. M. A. and PATTYN, S. R. Classification of leprosy cases under field conditions in Bangladesh. II. Reliability of clinical criteria. Lepr. Rev. 66(1995)134-143.
6. HASTINGS, R. C, ED. Leprosy. Edinburgh: Churchill Livingstone, 1985.
7. JAMET, P., Jr, B. and THE MARCHOUX CHEMOTHERAPY STUDY GROUP. Relapse after long-term follow up of MB patients treated by WHO multidrug regimen. Int. J. Lepr. 63(1995)195-201.
8. RICHARDUS, J. H. and CROFT, R. P. Estimating the size of the leprosy problem: the Bangladesh experience. Lepr. Rev. 66(1995)158-164.
9. RIDLEY, D. S. and JOPLING, W. H. Classification of leprosy according to immunity; a five-group system. Int. J. Lepr. 54(1966)255-273.
10. SHETTY, V. P., SUCHITRA, K., UPLEKAR, M. W. and ANTIA. N. H. Higher incidence of Mycobacterium leprae within the nerve as compared to skin among MB leprosy patients released from multidrug therapy. Lepr. Rev. 68(1997)131-138.
11. VAN BRAKEL, W. H.,. DE SOLDENHOFF, R. and Mc-DouGALL, A. C. The allocation of leprosy patients into paucibacillary and multibacillary groups for multidrug therapy, taking into account the number of body areas affected by skin, or skin and nerve lesions. Lepr. Rev. 63(1992)231-246.
12. TB AND LEPROSY CONTROL SERVICES. Technical guide and operational manual for leprosy control in Bangladesh. Dhaka: Government of Bangladesh. 1995.
13. WHO EXPERT COMMITTEE ON LEPROSY. Sixth report. Geneva: World Health Organization, 1988. Tech. Rep. Ser. 768.
14. WHO EXPERT COMMITTEE ON LEPROSY. Seventh report. Geneva: World Health Organization. 1988. Tech. Rep. Ser. 874.
15. WHO STUDY GROUP. Chemotherapy of leprosy. Geneva: World Health Organization. 1994. Tech. Rep. Ser. 847.
16. WHO STUDY GROUP. Chemotherapy of leprosy for control programmes. Geneva: World Health Organization. 1982. Tech. Rep. Ser. 675.
1. M.A., B.M., B.Ch., M.R.C.G.P., D.T.M.&H., Danish Bangladesh Leprosy Mission. Nilphamari 5300. Bangladesh.
2. M.D., Ph.D., Professor and Head.
3. M.Sc., M.Sc, Aberdeen.. Department of Public Health. University of Aberdeen, Scotland.
4. M.D., Ph.D., Epidemiologist. Department of Public Health. Erasmus University, Rotterdam. The Netherlands.
Reprint requests to Dr. Richard P. Croft. 70 Culver Lane. Reading RG6 IDY. U.K. e-mail: richard@rcroft.demon.co.uk
Received for publication on 22 September 1998.
Accepted for publication in revised form on 28 October 1998.