- Volume 65 , Number 1
- Page: 90–4
Pathologic changes in a tibial nerve with surviving M. leprae in a healed tuberculoid leprosy patient
ABSTRACT
A tibial nerve f rom a disease-arrested, borderline tuberculoid (BT) leprosy patient was dissected out and examined almost in its entirety using hematoxylin and eosin staining, a modified Fite's stain for acid-fast bacilli (AFB). solochrome cyanin stain for myelin, and van Gieson's stain for fibrous tissue. Fibrosis of the perineurium and epineurium and fibrous replacement of the nerve parenchyma, which was maxium at the ankle joint area, were seen. In focal areas inflammation was present, especially in the epineurium around blood and lymph vessels. Even 21 years after adequate antileprosy therapy, AFB were present in the endoneurium in all except 2 of the 10 segments of the nerve, evoking hardly an inflammatory reaction or other ill effects. It is pointed out that BT leprosy should also be considered a generalized disease, especially when there is peripheral nerve trunk involvement and, in such cases, a longer duration of currently available antileprosy therapy is advisable. Trauma to nerve trunks plays a major role in producing nerve destruction and paralysis.RÉSUMÉ
Un nerf tibial d'un malade tic la lèpre de type borderline-tuberculoide donl la maladie était arrêtée a été disséqué et examiné presque dans sou entièreté en utilisant une coloration à l'hémaloxylinc et à l'éosine, une coloration de Fite modifiée pour les bacilles acidorésistants (BAR), une coloration à la cyanine de soloebrome pour la myéline, et une coloration de van Gieson pour le tissu fibreux. On a observé une fibrose du perinèvre et de l'epinèvre et le remplacement libreux du parenchyme nerveux, qui était maximale dans la région de l'articulation de la cheville. Une inflammation était présente en foyers, particulièrement dans l'epinèvre autour des vaisseaux sanguins et lymphatiques. Même 21 ans après un traitement anti-lèpre adéquat, des BAR étaient présents dans l'endonèvre de tous les 10 segments de nerf, sauf 2, évoquant presque une réaction inflammatoire ou d'autres effets néfastes. Il est souligné que la lèpre BT devrait aussi être considérée comme une maladie généralisée, particulièrement lorsqu'un tronc nerveux périphérique est impliqué et. dans de tels cas, une durée plus longue du traitement anti-lèpre disponible actuellement est recommandable. Les traumatismes des troncs nerveux jouent un rôle majeur dans la destruction nerveuse et la paralysie.RESUMEN
Se disectó un nervio tibial de un caso curado de lepra tuberculoide subpolar (BT) y se examinó usando las tinciones de hematoxilina-eosina. una tinción modificada de Fite para bacilos ácido-resistentes (BAAR), una tinción de solocromo-cianina para miclina, y la tinción de van Gieson para tejido fribroso. Se observó fibrosis del perineurio y del epineurio. y reemplazamiento librótico del parénquima del nervio el cual fue máximo en el área de la articulación del tobillo. También se observó inflamación en áreas focales, especialmente en el epineurio. alrededor tie los vasos sanguíneos y linfáticos. Se encontró que aun después de 21 años del tratamiento antileproso, 8 de los 10 segmentos del nervio estudiado mostraron BAAR en el endoneurio, pero su presencia difícilmente estuvo asociada con una reacción inflamatoria o con otros electos mal definidos. Se hace incapié en que la lepra BT debe considerarse también como una enfermedad generalizada, especialmente cuando hay afección periférica del tronco nervioso y que en tal caso es aconsejable prolongar la duración tic la terapia antileprosa, til truma a los troncos nerviosos juega un papel importante en la destrucción nerviosa y en la parálisis consecuente.Histopathological studies of the entire length of a peripheral nerve trunk in leprosy are very rare because to obtain such specimens is very difficult. Such studies are very informative and contribute much to the understanding of the disease process and its management (5-8). In chronic granulomatous disease like leprosy and tuberculosis, the organisms are known to survive in healed lesions for long periods. These persisting acid-fast bacilli (AFB) may serve occasionally as the nidus for relapses, or they may lie dormant without producing any ill effects. The detailed study of the pathological changes in the tibial nerve of one such healed borderline tuberculoid (BT) patient is presented in this paper.
MATERIALS AND METHODS
A 40-year-old female reported with a large planter ulcer involving the right heel which extended into the ankle joint producing sinuses on both sides of the joint. She had a history of having had two hypopigmented anesthetic patches, one on the medial aspect of the right thigh and the other on the posterior aspect of the right leg 24 years ago. No nerve trunk involvement was recorded then. A diagnosis of BT leprosy was made, and she was treated with dapsone 100 mg daily. The patches disappeared in 3 years and the treatment was discontinued. While she was undergoing antileprosy therapy she developed right ulnar palsy and recurrent planter ulcers, first in the right forefoot and later in the right heel. Over time the forefoot was completely destroyed by recurrent ulceration and the heel ulcer persisted and extended into the ankle joint.
On examination she had no skin patches. All peripheral nerve trunks appeared normal. However, the right common peroneal nerve felt slightly thickened and hard. The right forefoot was missing. There were one large fungating ulcer in the right heel and two other fungating ulcers on either side of the ankle joint. All three ulcers were intercommunicating and were discharging foulsmelling pus. Biopsy examination of the edges of the three ulcers showed squamous cell carcinoma, and a piece of tissue protruding from the ulcer showed chronic osteomyelitis. X-ray revealed total disorganization with pyogenic arthritis of the ankle joint and osteomyelitis involving both the tibia and the fibula. The right inguinal group of lymph nodes was enlarged. An above-knee amputation was performed and the enlarged inguinal group of lymph nodes was excised.
The entire specimen of the leg was immersed in 10% neutral buffered formalin and was also perfused with the fixative through the popliteal vein. The lymph nodes were also fixed in the same fixative. After 4 weeks of fixation of the leg, the tibial nerve was dissected from a level above the popliteal fossa to the ankle joint. Because the foot and the heel were extensively destroyed by the ulcers, the tibial nerve and its branches beyond the ankle joint could not be obtained. Samples of the nerve tissue were taken every 3 to 4 cm along the length of the nerve for histopathological study. They were processed for paraffin sections: 5- µ m sections were cut, one was stained with hematoxylin and eosin (H&E) for routine study, one with acid-fast stain according to a modified Fite's technique (4), one with van Gieson stain for evaluating fibrosis, and one with solochromc cyanin stain (3) for studying the integrity of myelin. Representative pieces of tissue from the edge of the ulcers, lymph nodes and pieces of bone were also subjected to histopathologic examination.
RESULTS
Histopathologic examination. Specimens from the edges of the ulcers from all three sites confirmed the diagnosis of lowgrade, well-differentiated, squamous cell carcinoma. Several pieces from the enlarged inguinal lymph nodes showed only reticuloendothelial hyperplasia consistent with chronic lymphadenitis, and there was no evidence of tumor. The bone showed evidence of chronic osteomyelitis.
Ten segments, each measuring 3 to 4 cm in length, from the entire tibial nerve dissected from an area above the knee joint to the ankle joint were available for histopathologic study. The number of fascicles varied from 18 in segment 1, just above the knee, to 32 in segment 10, near the ankle joint. The first four segments of the tibial nerve situated around the popliteal fossa showed moderate thickening, fibrosis and hyalinization of the perineurium (Fig. 1). The epineurium was infiltrated with lymphocytes, macrophages and many plasma cells found mainly around lymph and blood vessels (Fig. 2), but there was no granuloma. There was only minimal fibrosis of the endoneurium in which many axons could easily be seen (Fig. 3) and it, also, was free of any inflammation. The van Gieson stain showed the presence of much collagen in the perineurium and only little collagen in the endoneurium. Solochrome cyanin stain confirmed that most of the axons in these fascicles were well myelinated. Two entire sections from each segment stained for AFB were carefully screened under an oil immersion lens and one or two AFB in each were found inside thin, spindle-shaped Schwann cells surrounded by collagen bundles in the first four segments.
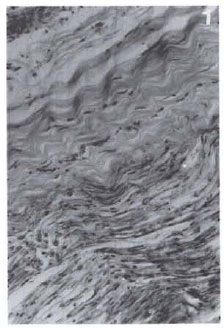
Fig 1. Photomicrograph of a longitudinal section of the tibial nerve at the knee joint level showing thickening fibrosis and hyalinization of the perineurium (I I&E x250).
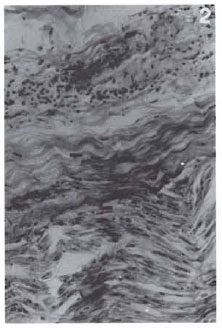
Fig 2. Photomicrograph of a longitudinal section of the tibial nerve at the knee joint level showing inflammation of the epineurium with a perivascular collection of lymphocytes, plasma cells and macrophages (H&Ex250).
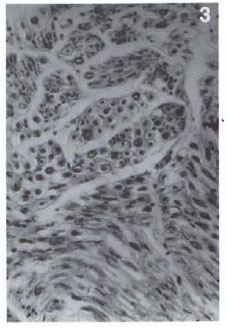
Fig . 3. Photomicrograph of ft cross section of the tibial nerve at the knee joint level showing minimal fibrosis of the nerve parenchyma. Most of the nerve fibers appear normal and are well myelinated (solochrome cyaninstain x400).
A significant but gradual change in the histopathological appearances of segments 5 to 10 was noticed. There was minimal perineurial thickening with fibrosis and hyalinization. The endoneurium showed considerable fibrosis and hyalini/.ation with replacement of most of the normal axons (Fig. 4). Not all fascicles were involved to the same extent. The fibrosis was patchy in some but was almost total in others. Segment 10 showed the maximum fibrous replacement of normal nerve parenchyma. The endoneurium was also infiltrated with a few scattered lymphocytes and occasional plasma cells. The epineurium had edema and scattered areas of infiltration with plasma cells, lymphocytes and a few macrophages mostly around blood and lymph vessels. There was no granuloma formation in any of the segments. The van Gieson stain confirmed the presence of collagen replacing much of the endoneurium and perineurium. In all of the solochrome-stained sections almost complete demyelination of the axons was evident. Acid-fast staining showed one or two AFB in the endoneurium, amid collagen bundles in all segments except segments 5 and 7.
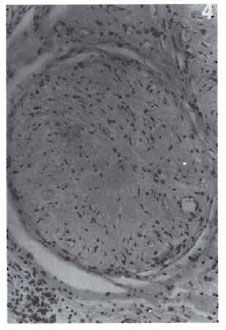
Fig. 4. Photomicrograph of a cross section of the tibial nerve at the ankle joint level. There is almost total replacement of the normal nerve parenchyma by hyalinized fibrous tissue ( H&E. x250).
DISCUSSION
This patient first reported to the hospital with only two hypopigmented anesthetic patches localized in the right leg and thigh. While she was undergoing dapsone antileprosy therapy for 3 years she developed ulnar palsy and trophic ulcers in the heel and forefoot, indicating involvement of the right tibial nerve and common peroneal nerve. From these findings it is clear that BT leprosy is also a generalized disease and can progressively develop multiple nerve lesions. Therefore, careful and periodic examination and assessment of peripheral nerves during treatment and during posttreatment follow up is imperative, especially in those patients who manifest early signs of nerve involvement. This patient had dapsone monotherapy for 3 years which was then considered adequate, and yet she developed progressive paralysis of several nerves. Also Mycobacterium leprae had persisted in the nerve tissue for nearly 24 years. The present policy of giving every paucibacillary patient 6 months of multidrug therapy with rifampin and dapsone (7). or even a shorter course with newly introduced drugs like ofloxacin and minocycline, may not be acceptable for all patients. Appropriate treatment with antiinflammatory drugs like corticosteroids to prevent paralysis and adequate antileprosy therapy to kill and eliminate persistent organisms should be administered. Antileprosy therapy should be tailored to the needs of individual patients and, if necessary, should be given for a longer duration evenas in multibacillary patients. There have been instances in which patients who were discharged as cured after a period of antileprosy therapy developed paralysis overtime (6).
It is interesting to find in this patient that inflammation was confined mostly to the epineurium and that it was mostly around blood and lymph vessels. There was no granuloma but only nonspecific inflammation. It is quite possible that this inflammation is an extension of the extensive chronic inflammatory lesion in the skin, subcutaneous tissue and bones of the foot. The absence of granuloma and a minimal involvement of the nerve parenchyma, and that involvement only in the portion of the nerve near the ulcers, make it less likely to be a reaction to the presence of M. leprae and its antigens.
Finding AFB in the fibrosed endoneurium of all except 2 of the 10 segments of tibial nerve in this I3T patient shows that a few AFB can persist for long periods in nerves of healed leprosy patients without causing ill effects. It is well known that in the Ghon complex, the lesion heals with iibrous scarring and often with calcification. Most M. tuberculosis die, but a few remain viable in the lesion for many years and these may be responsible for a relapse at a later date (2). In this patient during 3 years of dapsone therapy most of the organisms would have died leaving behind a few in the fibrosed healed nerve. It is possible that if the immune mechanism diminishes or fails these organisms may multiply and be responsible for a relapse.
The maximum destruction of the tibial nerve was at the ankle joint area where it had extensive fibrous replacement of the normal nerve parenchyma. This is expected because during active disease the largest number of M. leprae would have been concentrated in this area. It is well known that the nerve at this site is subcutaneously placed and its temperature, therefore, is lower than the core body temperature, thus facilitating the multiplication of M. leprae (1). Also, the portion of the nerve at the ankle joint was much more traumatized than the nerve segments in any other area. Trauma to the nerves plays a very significant and perhaps predominant role in causing the destruction of the nerve and subsequent paralysis.
It is certainly interesting to record the persistence of M. leprae in 8 out of the 13 segments of a tibial nerve mostly surrounded by hyalinized fibrous tissue.
Acknowledgment. We acknowledge with gratitude the linancial support received from American Leprosy Missions International, 1 ALM Way; Greenville, South Carolina, U.S.A. We tire grateful to Mr. K. Rajanna for technical help and Miss K. Jayanthi for secretarial assistance.
REFERENCES
1. BINFORD, C. H. Comprehensive program for inoculation of human leprosy into laboratory animals. Pub. Health Rep. 71(1956)995-996.
2. CONNOR, D. H. and GlBSON, D. W. Infection and parasitic diseases. In: Pathology. Emannuel, R. and Faber, J. L.. eds. Philadelphia: J. B. Lippincott Co., 1988, chapter 9, pp. 326-451.
3. DRURY, R. A. B. and WALLINGTON, E. A. Carleton's Histologic Technique. 5th edn. Oxford: Oxford University Press, 1980, p. 381.
4. JOB, C. K. and CHACKO, C. J. G. A modification of Fite's stain for demonstration of M. leprae in tissue sections. Indian J. Lepr. 58(1986)17-18.
5. JOB, C. K. and DESIKAN, K. V. Pathologic changes and their distribution in peripheral nerves in lepromatous leprosy. Int. J. Lepr. 36(1968)257-270.
6. JOB, C. K., VICTOR, D. B. I. and CHACKO. C. J. G. Progressive nerve lesion in a disease-arrested leprosy patient; an electron microscope study. Int. J. Lepr. 45(1977)255-260.
7. WHO STUDY GROUP. Chemotherapy of leprosy for control programmes. Geneva: World Health Organization, 1982. Tech. Rep. Ser. 675.
8. ZHAO, B., SHU, W. Y., XIA, M. Y. GU, C. I., Lou, H. Y. and GAO, X. I. Study of the pathologic changes in posterior tibial nerve in arrested borderline leprosy patients. (Abstract) Int. J. Lepr. 52(1984)731.
1. M.D., F.R.C.Path, Thomas Hospital and Leprosy Center, Chettupattu 606 801, T.S. District. Tamil Nadu, India.
2. M.B.B.S., D.C.P., Thomas Hospital and Leprosy Center, Chettupattu 606 801, T.S. District. Tamil Nadu, India.
3 M.B.B.S.. D.T.M.&H., Thomas Hospital and Leprosy Center, Chettupattu 606 801, T.S. District. Tamil Nadu, India.
4. M.D., St., Thomas Hospital and Leprosy Center, Chettupattu 606 801, T.S. District. Tamil Nadu, India.
Received for publication on 14 May 1996.
Accepted tor publication in revised form on 30 July 1996.